Ultrasound is sound that occurs at frequencies above the 17,000- to 20,000-Hz limit of human hearing. As such, it shares the characteristics of sound in general: its waves consist of alternating compressions and rarefactions; it requires
a medium for transmission; it transmits energy; and it can be focused, refracted, and reflected. Although arguments are made for a variety of frequencies, most therapeutic ultrasound treatment occurs between 0.8 and 3 MHz due to the practical considerations of focusing, penetration, and standardization.
Biophysics
Ultrasound has both thermal and nonthermal effects. Heat production, with its goals of hyperemia, enhanced soft-tissue extensibility, and lessened pain and muscle tone, is the best known. Nonthermal processes—which include cavitation, streaming, standing waves, mechanical deformation, and shock waves—may also be sought because of their ability to alter cell membrane permeability and function (
58). The first of these nonthermal processes, cavitation, occurs when high-intensity ultrasound passes through a liquid and produces small bubbles that may either rhythmically oscillate in size (stable cavitation) or grow and abruptly collapse (unstable cavitation). In either case, large temperature and pressure changes may occur (
59) and produce localized tissue distortion and injury. Pressure asymmetries produced by the presence of an ultrasonic beam can generate large shear forces that in turn may lead to media movement (streaming, microstreaming), tissue damage, or accelerated metabolic processes (
58,
60). Standing waves are generated from the superposition of sound waves and produce fixed regions of high and low pressure at half-wavelength intervals (which for 1 MHz ultrasound [tissue velocity 1,500 m/s] is about 0.75 mm) (
61). Graphic effects are possible; ultrasound exposure produces repetitive bands of red blood cells in chick embryo vessels (
62).
Ultrasound penetration into tissue depends on a number of factors. Frequency is particularly important as penetration decreases by a factor of 6 as the frequency increases from 0.3 to 3.3 MHz (
63). Orientation is also critical. For example, about 50% of a 0.87-MHz ultrasound beam penetrates 7 cm in a direction parallel to muscle fibers, but the same beam penetrates only 2 cm in a transverse direction (
63). Tissue type is also significant. Fifty percent of an ultrasound beam penetrates several centimeters in muscle, only a few tenths of a millimeter in bone, and 7 to 8 cm in fat (
63,
64). In practice, 3-MHz ultrasound is used for superficial tissues such as those of the hand and temporomandibular joint, as most of its energy is absorbed within 1 to 2 cm of the skin’s surface. Lower frequency beams are used when deeper penetration is desired.
Ultrasound treatments are frequently delivered to anisotropic tissue, and it should be remembered that localized areas of temperature elevations of 5°C or more may occur at sound absorption discontinuities such as those that occur at bone-soft-tissue interfaces (
63,
64,
65). Heat is lost from tissue as the result of conduction and cooling effects of the local blood flow.
Technique
There are two philosophies of ultrasound therapy. The most widely held is that ultrasound’s benefits are due to heating. This approach typically uses an unmodulated, continuouswave (CW), or high-intensity pulsed beam with intensities of 0.5 to 2.5 W/cm2. The second approach emphasizes ultrasound’s nonthermal properties. In this case, the beam is modulated to deliver brief pulses of high-intensity ultrasound separated by longer pauses of no power and as a result lower average energy intensity. Thus, heating is minimized and ultrasound’s nonthermal effects are emphasized.
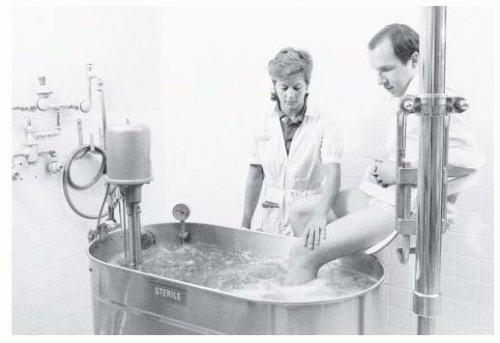
Ultrasound is usually delivered by moving the applicator (
Fig. 63-6) over the treated area in slow (1 to 2 cm/s), overlapping strokes. Treatments cover areas of about 100 cm
2 and last 5 to 10 minutes. Indirect ultrasound, while less common, is used to treat irregular surfaces such as the foot and ankle where it is difficult to keep the applicator in contact with the skin. In these situations, the body part is placed in a container filled with degassed water. The applicator is held a short distance away (0.5 to 3.0 cm) and moved without touching the skin. Power intensities may need to be higher due to transmission losses.
Coupling between the applicator and the skin is not a trivial issue. The treatment area should be cleansed before treatment, and a coupling agent is necessary. Degassed water (water that has been allowed to sit for several hours) is used for indirect ultrasound because the dissolved gases in water fresh from the tap form bubbles during treatment and attenuate the beam. Little practical difference exists between commercial gels and mineral oil for direct applications, with transmissivity similar to that for degassed water (
68). However, mineral oil becomes watery and most people use the commercial products because of the convenience. Coupling agents should not be salt based (e.g., those used for EMG or ECG), as the salt may damage the applicator.
Phonophoresis is a variant of ultrasound in which biologically active substances are combined with the coupling medium in the hope that the ultrasound will force the active material into tissue. Although this technique has been in use since the 1960s, neither its effectiveness, penetration, optimal frequency, appropriate coupling mediums/active materials nor amount of material lost to the subcutaneous circulation is well established. Although claims of increased cortisol concentrations at depths of several centimeters after corticosteroid phonophoresis have been made, our own research as well as that of others (
69,
70) finds limited evidence for deep penetration. Clinical reports are mixed. Thus, although some clinical studies report phonophoresis with a variety of agents successful in terms of improved shoulder range of motion and pain following the treatment (
71) as well as in the treatment of keloids and sarcoid nodules (
72), other work involving an assortment of musculoskeletal conditions may find the approach no more effective than ultrasound alone (
73).
Indications
Musculoskeletal Conditions. The research relating to musculoskeletal condition is surprisingly inconclusive (
74). For example, a study of 63 patients with calcific shoulder tendonitis treated with pulsed ultrasound (0.89 MHz, 2.5 W/cm
2) found that the treated patients had significantly larger improvements in their pain and decrease in calcium deposits relative to their sham controls at the end of an intensive 6-week treatment program. However, this difference had disappeared at follow-up 9 months later (
75). Although ultrasound may be more beneficial than corticosteroid injection in the treatment of shoulder pain, other studies and reviews find it no more effective than placebo or nonsteroidal anti-inflammatory medications for a variety of conditions ranging from subacromial bursitis or lateral epicondylitis (
76) to heel pain (
77). More tellingly, perhaps, an evidence-based practice guideline panel came to the conclusion that although therapeutic ultrasound was effective in the treatment of calcific tendonitis of the shoulder, there was no compelling evidence of its clinical benefits for other sources of musculoskeletal pain (
78). Although these studies raise legitimate issues about its effectiveness in such conditions, many physicians and therapists remain convinced that ultrasound is useful for the treatment of at least some musculoskeletal pain. In support of this, several reviews have found evidence of some benefits in the form of increased motion and lessened stiffness from the cautious use of ultrasound in
patients with rheumatoid arthritis (
79,
80,
81). A recent small scale study of ultrasound treatment of myofascial trigger points found significant pain relief from conventional relative to low-intensity ultrasound stimulation (
82).
Contractures. Ultrasound is effective in increasing the range of motion of the heel cords, periarthritic shoulders, and contracted hips (
83,
84). In fact, due to its penetration and focusing capabilities, it is the only agent that can significantly heat (by 8°C to 10°C) the hip joint (
65). Hand and Dupuytren contractures also may benefit from ultrasound (
85), although a small study of burns did not find treatment beneficial (
86). Collagen and tendon extensibility increases as temperatures increase and decreases as tissue cools. As a result, stretching should begin during heating and should continue as the tissue cools and “sets.”
Soft-Tissue Wounds and Inflammation. Ultrasound treatment of wounds and inflammation is based on the belief that either its heat (by increasing blood flow, metabolic, or enzymatic activity) or nonthermal effects (perhaps by changing cell wall permeability) accelerate healing. Laboratory studies offer some support (
87). Human studies, however, provide a more mixed picture with a recent review of decubitus ulcers concluding that the evidence was too weak to assess (
88). Some feel that inflammation and swelling are indications for ultrasound. Others believe that the heating and membrane permeability changes associated with treatment prohibit its use in acutely inflamed conditions such as in recent trauma and active rheumatoid arthritis.
Trauma. Although ultrasound may aggravate tissue damage and swelling if used too soon after an injury, subacute hematomas (
89) and postpartum perineal pain (
90) may improve more rapidly with treatment. Ankle sprains are a common indication for ultrasound treatment. Even here, benefits are unclear with a systematic review involving more than 570 patients concluding that current evidence, at best, supported the presence of limited benefit (
74). A number of clinical and animal studies find evidence that ultrasound at intensities on the order of 1 W/cm
2 may provide at least short-term benefits in the treatment of symptomatic carpal tunnel syndrome (
91,
92). Although these reports are intriguing, benefits are not always evident and remain controversial (
93).
Fractures. Low-intensity ultrasound improves the repair of bony injuries (
94). For example, 30 mW/cm
2 pulsed 1.5-MHz ultrasound accelerates the healing of closed and open grade 1 fractures (
95,
96). Although ultrasound is not typically used for this purpose, its use has been approved by the Food and Drug Administration (FDA) for the treatment of some fractures. In view of the fact that 5% to 10% of fractures heal slowly (
97), there may be a wider applicability for this treatment in the future.
Other Indications. Postherpetic neuralgia is often resistant to conventional treatment. Treatment with both pulsed and continuous 1- to 1.5-MHz ultrasound has been evaluated. Unfortunately, the studies have again often been poorly controlled, and the results are unclear; some investigators have found improvement (
98,
99), whereas others have not (
100). As ultrasound has thermal, and possibly nonthermal, effects on nerve conduction (
101), further evaluation seems appropriate. Plantar warts, keloids, scars, and even chronic sinusitis are additional refractory conditions for which pulsed and conventional ultrasound has inconclusive benefits (
102,
103,
104).