Chapter Two Theoretical basis of combined movement theory
Introduction
Some of the reasons for this controversy are:
We are still developing a body of evidence to establish the physiological and psychological effects of manual therapy. Ultimately, manual therapy is a method of intervention for musculoskeletal dysfunction that encourages accelerated recovery. In light of this we must consider how we are measuring our effectiveness. The measurement of manual therapy against other treatments when judged in terms of change in disability, and reported 12 months after our intervention, may not be a sensitive method of capturing our effect (McCarthy & Cairns, 2005).
Spinal manipulation
• A small amplitude, high velocity thrust, applied to a spinal joint
• Extends beyond a restriction in range
• Occurs at the beginning of resistance
The effects of manipulation?
• Tearing adhesions in the capsule
• Lengthening of the joint capsule
• Freeing trapped menisci or loose synovium
Tearing adhesions in the capsule or stretching joints?
Imagine a scenario where your patient has attended with pain at three quarters range, right rotation, depicted in the top line of Figure 2.1. You feel a manipulative technique will be potentially of value in your management programme. The starting position you would adopt for the manipulative thrust would be formed by a combination of three physiological movements. In extension, ipsilateral flexion and contra-lateral flexion, the amount of rotation developed will be much less than the amount of rotation required to stretch or ‘tear’ an adhesion. Thus, it is unlikely that we are aiming to lengthen or tear tissue with our manipulative thrusts, whereas we feel we are aiming to lengthen tissues with our mobilization/stretching techniques.
Is the thrust element of the technique applied at end of range? Physiotherapists familiar with the Maitland Concept will be used to the nomenclature of grades of movement as described by Geoff Maitland (Maitland, 1986). Grades I and II refer to passive movement (of small and large amplitude respectively) performed in the early part of the range. In this range the therapist will not perceive resistance to movement. Grades III and IV are (large and small amplitude) movements conducted in a range where resistance is detected by the therapist. Small amplitude movement in early ranges of resistance are noted as IV− whilst movement at end of range as IV+. Manipulative thrusts techniques have been notated as Grade V, suggesting that the technique is conducted beyond the end of range and indeed some therapists may perform a high velocity thrust at the end of passive range. In common with many other manual therapists and osteopaths we feel there are disadvantages to performing manipulative thrusts at the end of passive range and numerous advantages to avoiding this starting position (Evans & Breen, 2006). This assertion is based on an understanding of the effects of passive manipulation and mobilization and represent an individual viewpoint on the objectives of the technique. However, there are many views on the objectives of manipulative technique and some manual therapists may feel they should conduct a manipulation as an end-of-range technique in order to stretch tissue.
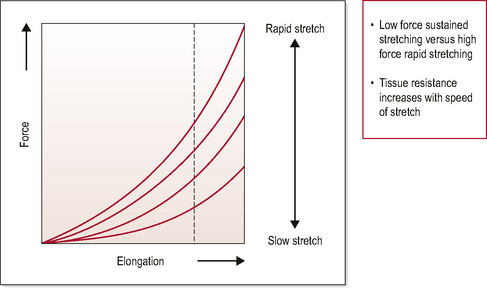
One of the aims of manual therapy is to elongate soft tissue. In the process of stretching connective tissue a stress/strain curve has been identified that represents the behaviour of the tissue. Figure 2.2 depicts the relationship between the application of a strain on tissue and its resultant change in length. The relationship is speed specific with changes in the speed of application resulting in differing lengthening characteristics (Lederman, 2005).
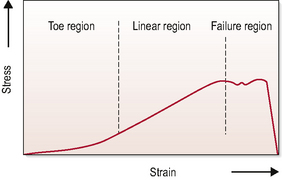
Figure 2.2 Stress–strain curve for soft tissue. Distinct areas: ‘the toe’, ‘the linear/elastic region’ and the ‘area of plastic deformation’. The toe area of the curve represents the initial stage of deformation where the crimping of bunches of collagen fibres occurs. The linear region of the curve represents deformation without micro-failure of collagen. The area after approximately 3–5% deformation represents micro-failure of collagen fibres and plastic deformation. At around 8% deformation there is macro-failure. Stress = force applied; Strain = deformation. (Threlkeld, 1992)
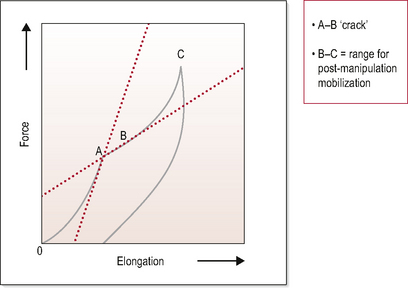
Connective tissue that is loaded quickly will deform less than tissue loaded slowly, with the same amount of force. This is an important factor when considering manipulative thrusts and lengthening tissue. Figure 2.3 illustrates the fact that greater force is required to elongate tissue if applied quickly rather than slowly. Less force is required to lengthen hypomobile soft tissue if applied slowly, and as quick, forceful movements have greater potential to evoke nociceptive afferent barrage, the therapist should consider carefully the use of thrust techniques when deliberately trying to reduce hypomobility, particularly in the presence of pain.
What about the pop/cavitation?
In the 1970s, Sandoz conducted a series of experiments looking at distraction of finger joints. He noted that if cavitation occurred during distraction (signified by an audible popping sound), there was a gain of 5–10° in the range of passive movement of the metacarpophalangeal joint in all directions and the active range of movement was also increased, but to a lesser extent. Sandoz also noted that regardless of the direction of the distraction to the metacarpophalangeal joint, the refractory period remained the same and a radiolucent space appeared on the X-ray film. Sandoz (1976) went on to review what was known about the mechanical effects of joint cavitation at the time and produced a summary diagram (Fig. 2.4).
In Figure 2.4, two important features of the effects of distraction on a synovial joint can be identified. Firstly, the phenomenon of cavitation does not occur at the end of the joint’s distraction range but rather in the middle of range. Secondly, there is a change in the profile of resistance to movement exhibited in the range preceding cavitation and immediately following it. Post cavitation there is a reduction in the force required to distract the joint; it is less resistant to movement.
This leaves the question of whether cavitations at the finger joints are the same as those that occurred at the facet joint. Méal and Scott (1986) and Conway et al (1993) conducted studies examining the sound signals created by distractions of the fingers and those produced by spinal manipulation. Observing that the sound signals had similar acoustic nature led them to postulate that a similar mechanism was occurring and that joint gapping resulting in an increased range of movement was likely. Since then Cramer et al (2000) and Cramer et al (2002) have examined the effect of manipulation on the zygapophysial (facet) joints using magnetic resonance imaging (MRI). Following a successful pilot study on 16 healthy subjects they went on to randomize 64 healthy volunteers into four groups (Cramer et al, 2002). All participants had their initial scan whilst lying supine, then group one were placed in a side-lying posture and re-scanned. The second group had a manipulation and then were re-scanned in a supine position. The third group received a manipulation and were then placed in a side-lying position and re-scanned and finally, the fourth group were turned onto their side briefly and then re-scanned in a supine position. The second scan was conducted within 15–20 minutes of the intervention.
 Clinical relevance
Clinical relevance
Following cavitation, there is a palpable change in the resistance profile of the passive movement. What was perceived as a short sharp build-up in resistance can immediately be perceived to change to a longer range of resistance, starting at the same point in range, but extending further into passive range. This perception can be depicted using movement diagrams (Fig. 2.5), as described by Maitland (1986).
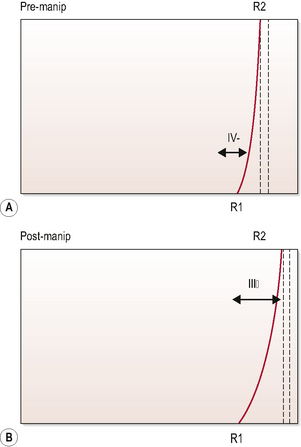
Figure 2.5 Depiction of the perception of resistance felt during a passive movement. Using right lateral flexion of C4/C5 as an example, (A) shows the resistance profile towards the end of the range of movement. (B) shows the profile perceived after cavitation. The short resistance profile in (A) would indicate that a grade IV mobilization would be an appropriate mobilization to treat in resistance, whilst the longer profile in (B) suggests a grade III would be indicated. For more detail on the selection of grades see Maitland (1986).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Clinical relevance
Clinical relevance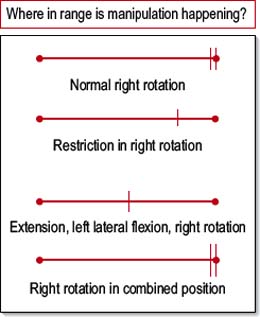
 Clinical relevance
Clinical relevance