Chapter Five Neurological assessment
Introduction
There is no ideal neurological examination technique. There are conventional ways to perform an examination, a conventional order of examination and conventional ways to elicit particular signs (Fuller, 1993). This chapter aims to address one of the main concerns for post-graduate manipulative therapists, namely how to establish the extent of the neurological examination. The chapter is designed to supplement the more comprehensive texts on neurological examination (Donaghy, 1997; Fuller, 1993; Harrison, 1996; Perkin, 1992) and not to represent a compendium of all neurological testing procedures. The essential message of the chapter is that whilst the vast majority of patients will require a basic screening examination of both central and peripheral nervous systems the examination must be expanded if central nervous system (CNS) dysfunction is identified.
History
An assessment of the patient’s neurological function is made with every patient and during the taking of the patient’s history, decisions regarding the likelihood of neurological dysfunction will be made by all but the most inexperienced therapist. During the subjective examination, hypotheses regarding the patient’s primary dysfunction may be made following various models of clinical reasoning (Doody & McAteer, 2002). A process of clinical reasoning based on hypothetico-deductive reasoning and pattern recognition will enable the therapist to recognize, formulate and test likely hypotheses of dysfunction during both the subjective and the physical examinations. (See Chapter 3.)
The history has been described as the most important and most productive part of the neurological assessment, the purpose of which is to answer the questions ‘where is the lesion and what is it?’ and ‘is it one lesion or does the condition involve a system within the nervous system?’ Thus, in order to ensure high sensitivity and specificity to neurological dysfunction there are some techniques, commonly used by expert clinicians (King & Bithell, 1998), to make the subjective examination more valid. Development of an awareness of neurological time courses, patterns of presentation, and mechanisms of pain production should increase diagnostic confidence.
Pattern recognition
Thinking of the history of a neurological dysfunction as having a shape, with an onset, a rate of evolution to maximum deficit, and a time at maximum deficit, or a rate of continuing progression or recovery to the present state, is a helpful way of visualizing a pattern of symptoms (Fuller, 1993) (Fig. 5.1).
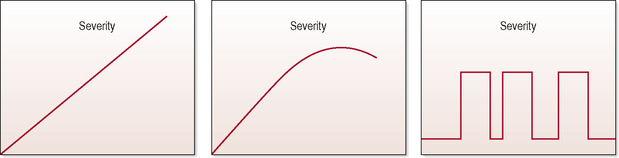
Figure 5.1 • Typical patterns of symptom presentation. (A) Tumour/degenerative; (B) infection/inflammation; (C) epilepsy migraine. (Fuller, 1993)
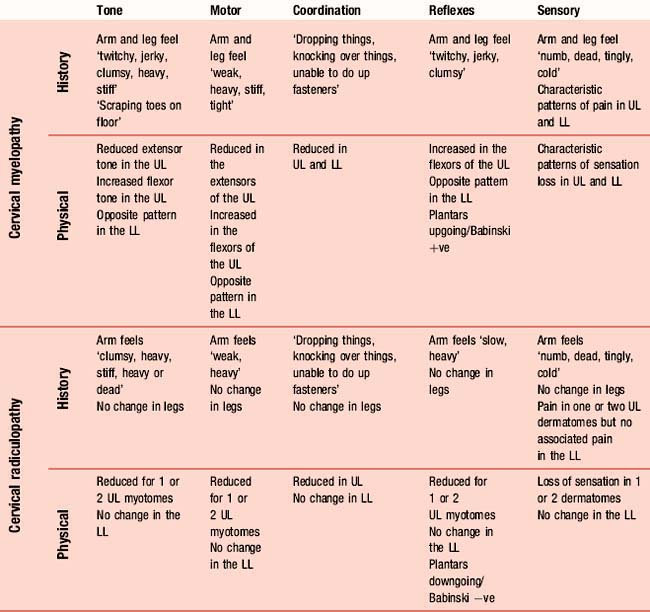
The physical neurological examination is traditionally structured into five components: assessing alterations in tone, muscle power, coordination, reflexes, and sensory perception (Perkin, 1992). A physical examination will elicit characteristic patterns of presentation from each component which, when combined with subjective information, will enable a clinical diagnosis to be made. Developing an appreciation of subjective patterns of presentation based on these five components should increase the validity of the subjective examination. Thus, by asking about perceptions of weakness (motor power), clumsiness (coordination), limb stiffness and shaking (tone), as well as pain, there will be a greater likelihood of identifying relevant dysfunction in the physical examination. Table 5.1 shows the features typical of two spinal conditions, cervical myelopathy and cervical radiculopathy, and highlights the subjective and physical characteristics of these upper and lower motor neuron lesions as an illustration of their distinguishable features.
Predominant symptom mechanism
The history should guide the therapist regarding the predominant mechanism of symptom production. In the case of pain, a sensitive and specific subjective examination will enable a hypothesis to be made regarding the predominant pain mechanism and thus whether a neurological examination is required. For example, if a patient has nociceptive ‘pinpoint’ pain in their cervical spine and no cues from their history to suggest neurological dysfunction, a neurological examination is not necessary. However, if the pain refers to the shoulder, a neurological examination would be indicated in order that possible radicular pain production and neural conduction loss could be evaluated. Thus, if the decision to conduct an examination is based on a pain mechanism model rather than on the extent of the referred pain, a more rational approach can be adopted. Whilst there is still some debate regarding the validity of the methods of identifying predominant pain mechanisms, the definitions of pain mechanisms are well accepted (Butler, 1995) (Table 5.2).
Table 5.2 Describing the main mechanisms of pain
| Pain mechanism | Description |
|---|---|
| Peripheral nociceptive | Local sources within muscles, joints and soft tissues |
| Peripheral neurogenic | Sources in peripheral nerves, nerve roots and cranial nerves |
| Central | Sources within neurons and synapses in the central nervous system |
| Efferent | Pain related to efferent mechanisms, influenced by motor neurons including those of the autonomic nervous system |
| Affective | Related to neurons and circuitry more concerned with the person’s affect |
Central or peripheral nervous system lesion
Typically the physical examination is structured around assessment of tone, power, coordination, reflexes and finally sensation testing (Hawkes, 1996). One of the rationales for this order of testing relates to the need to expand the subsequent components of the examination in the presence of potential CNS dysfunction. For example, symptoms from the history and signs of altered tone and power would indicate an expansion of coordination, reflex and sensory testing components, whilst no such signs and symptoms would suggest only a screening reflex and sensory screen was indicated. This is a principle that applies throughout all the components of the physical examination.
Tone
Extrapyramidal disorders affecting the basal ganglia, such as Parkinson’s disease, lead to a more uniform increase in tone distributed amongst flexor and extensor muscle groups with muscular rigidity in trunk and limb muscles (Perkin, 1992). Tremor and involuntary movements are common with loss of speed in intricate movement such as finger-to-thumb opposition and during gait (Harrison, 1996). The rigidity, associated with extrapyramidal lesions, and the spasticity, associated with an upper motor neuron lesion (UMNL), can be reliably tested with two quick upper limb tests: wrist circumduction and the pronator catch test respectively (Donaghy, 1997). The wrist circumduction test involves gripping the patient’s wrist with one hand and repeatedly circumducting the hand, whilst the pronator catch test involves abruptly supinating the patient’s wrist and detecting a sudden jerk of resistance. If these signs are positive, an expansion of the examination of tone would be indicated, to include the lower limbs (Table 5.3).
Table 5.3 The expanded and contracted tone, coordination and reflex examination
| Examination | Test | Rationale |
|---|---|---|
| Contracted | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|