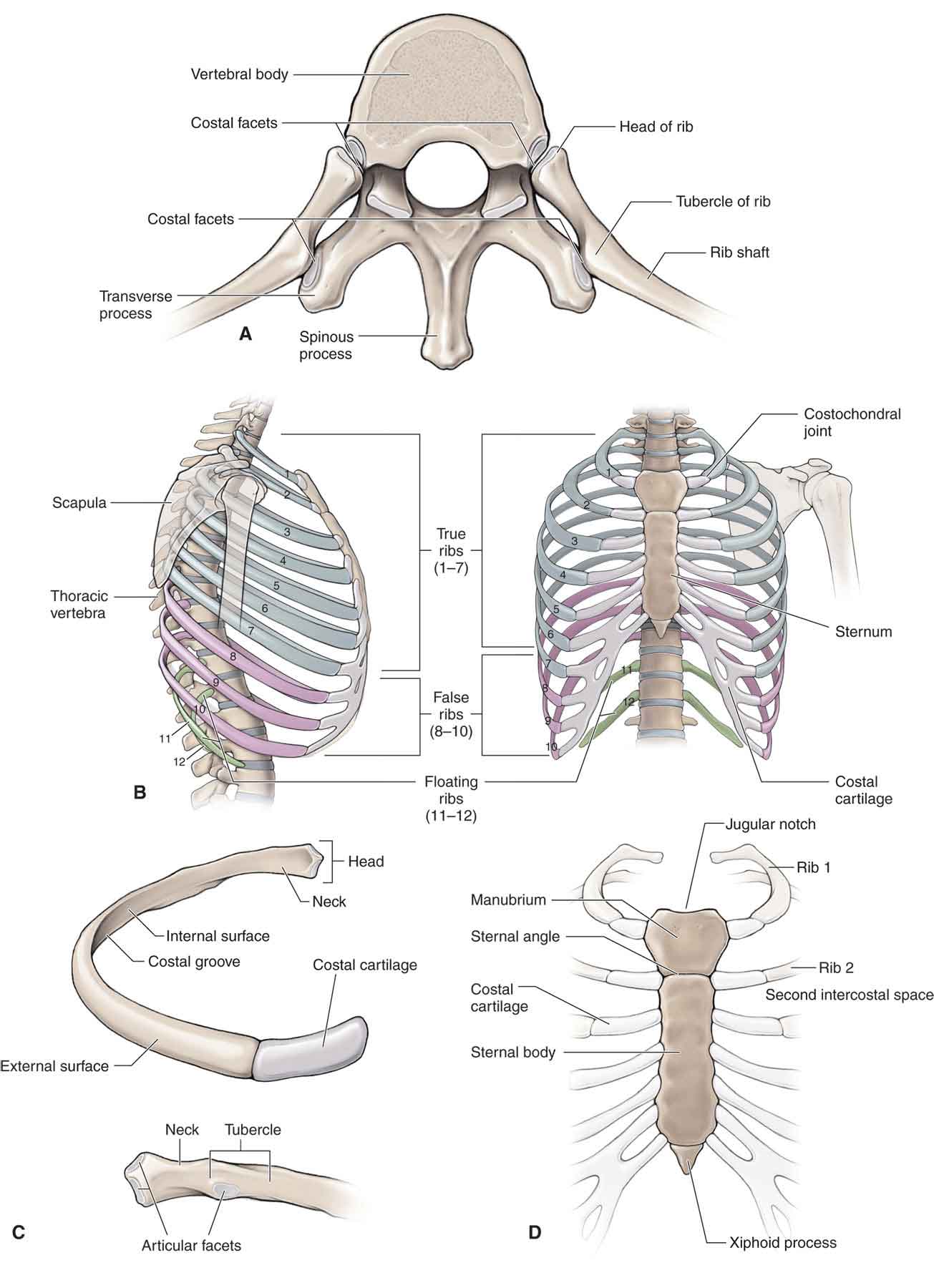
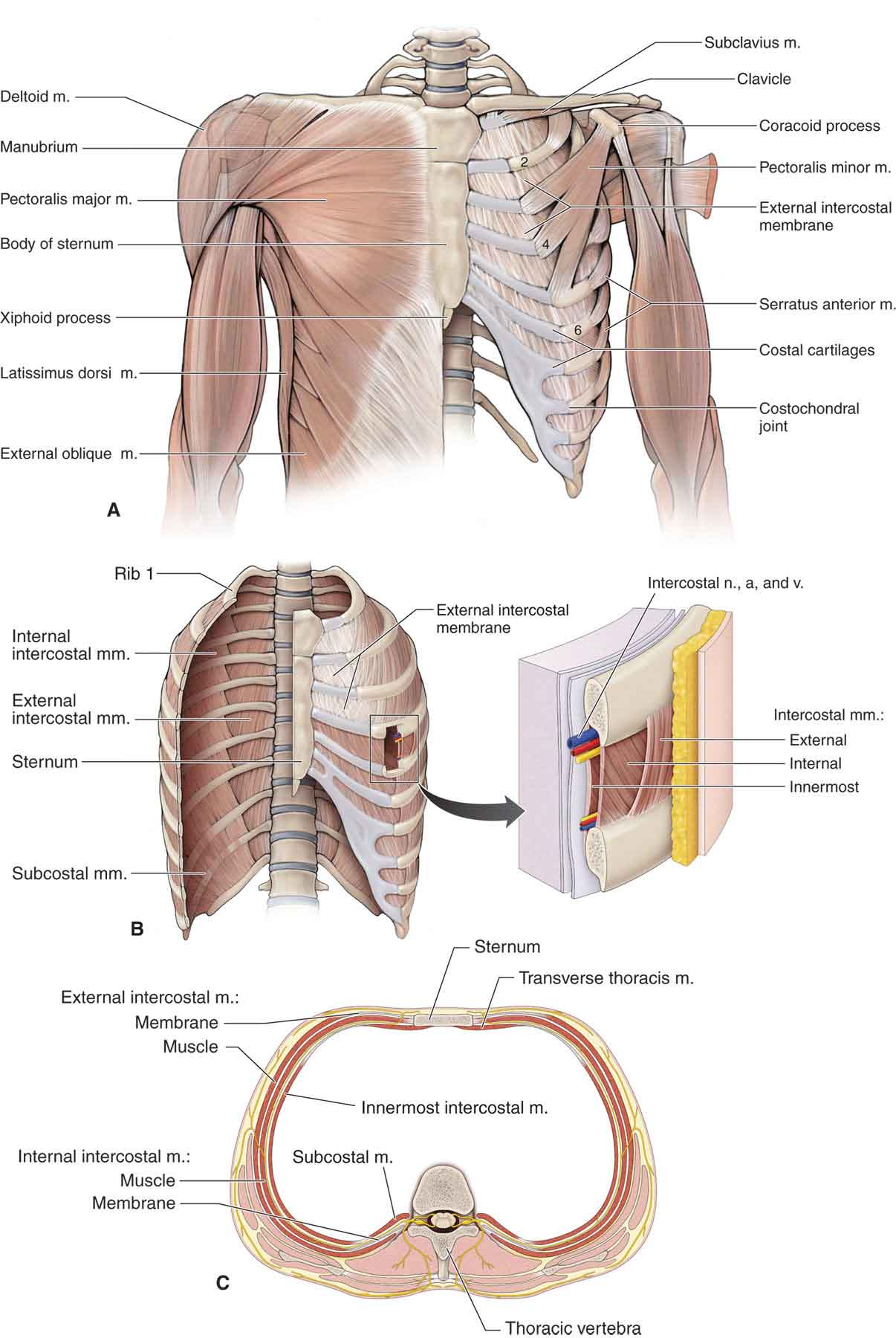
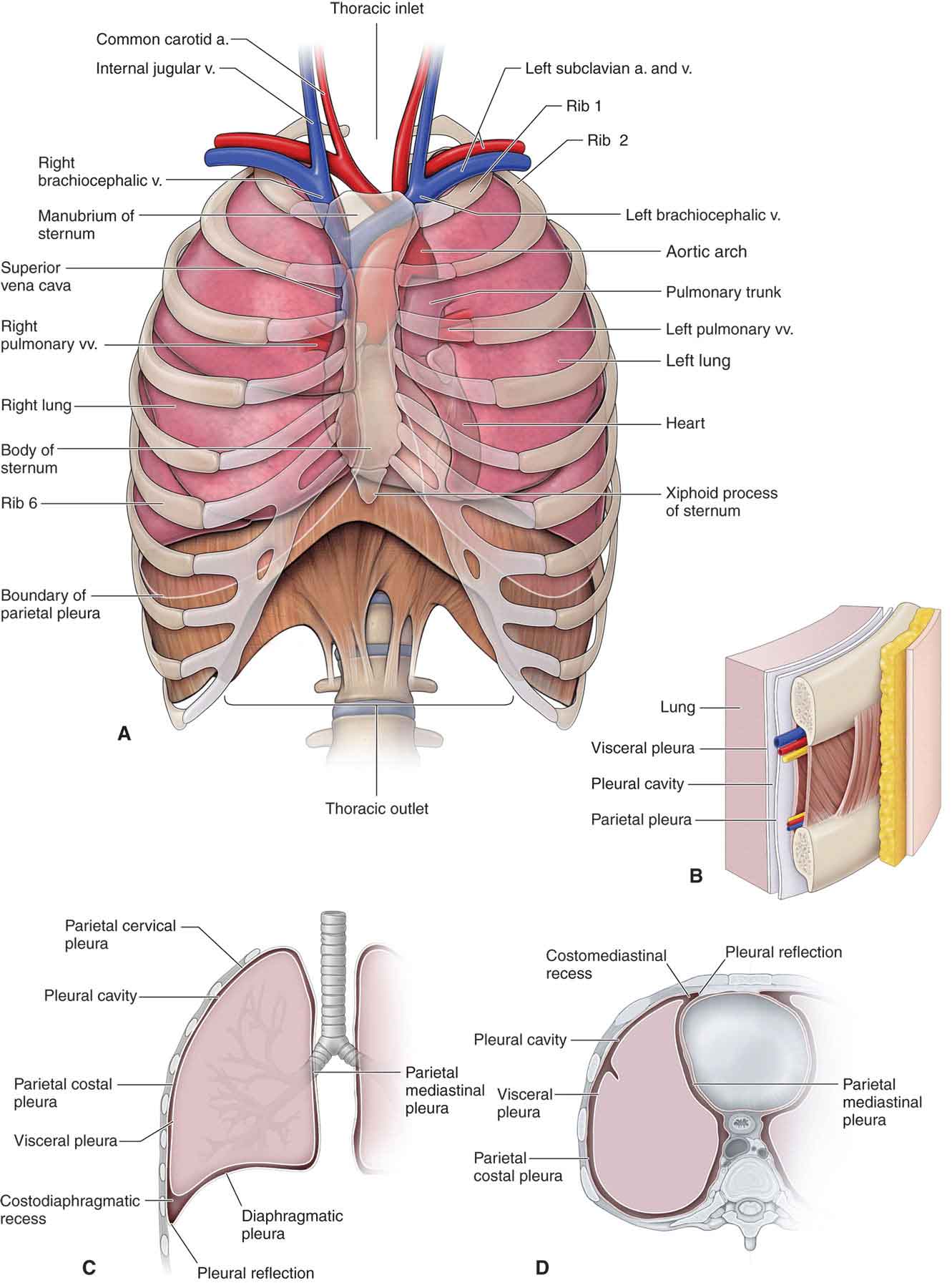
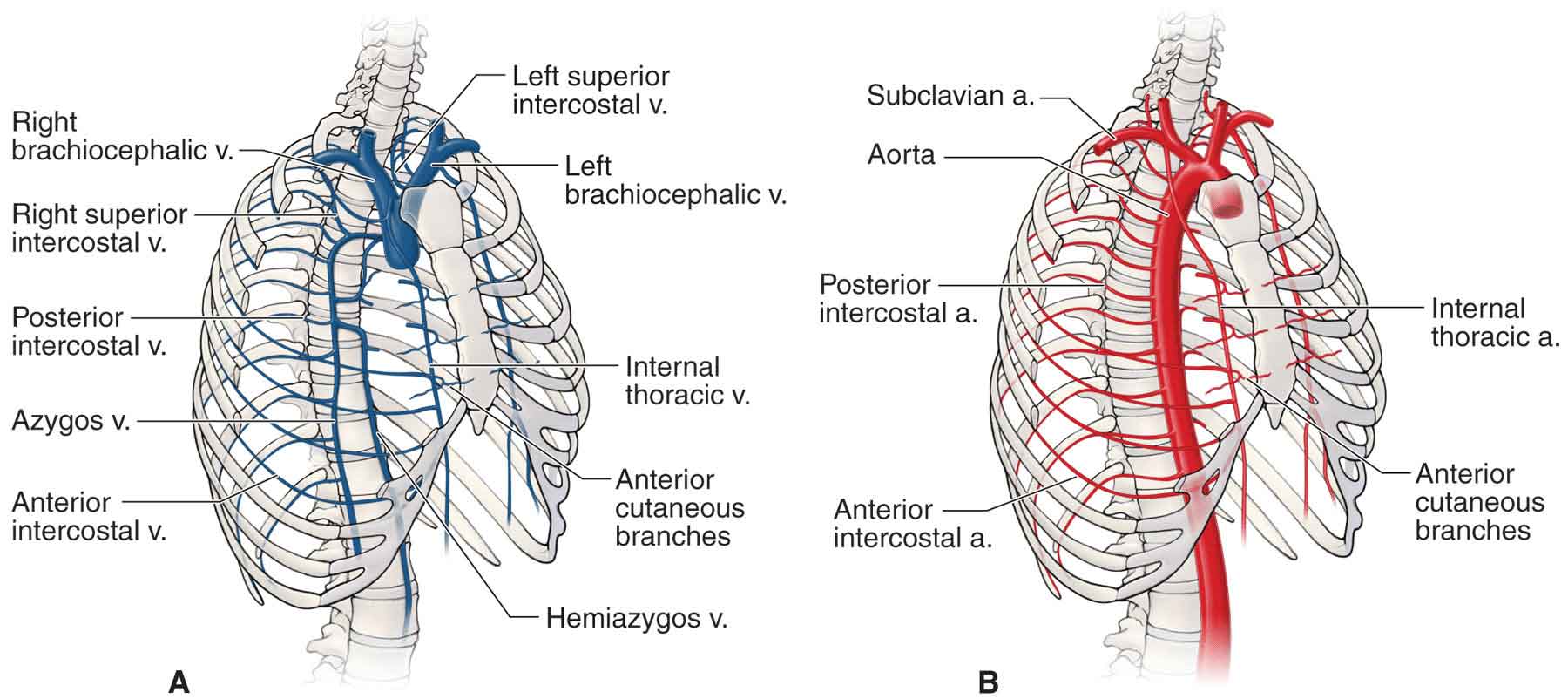
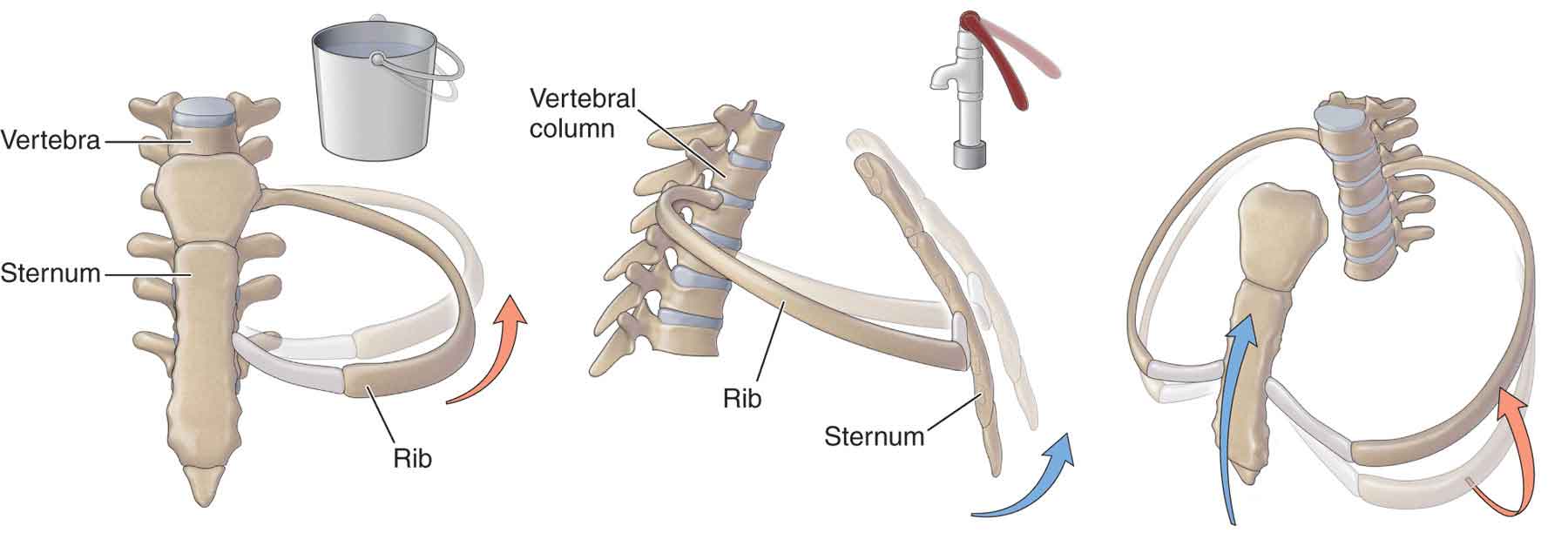
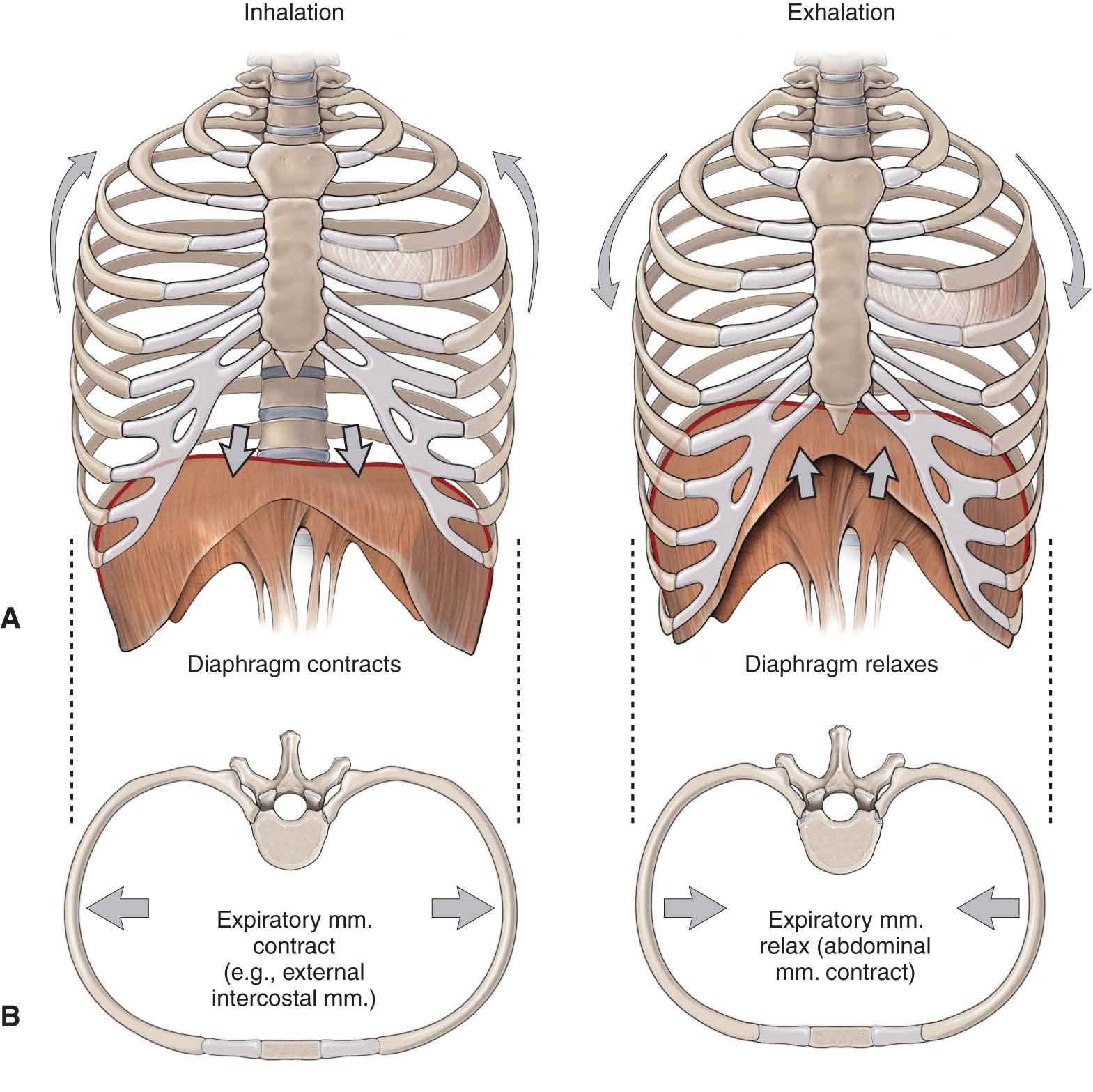
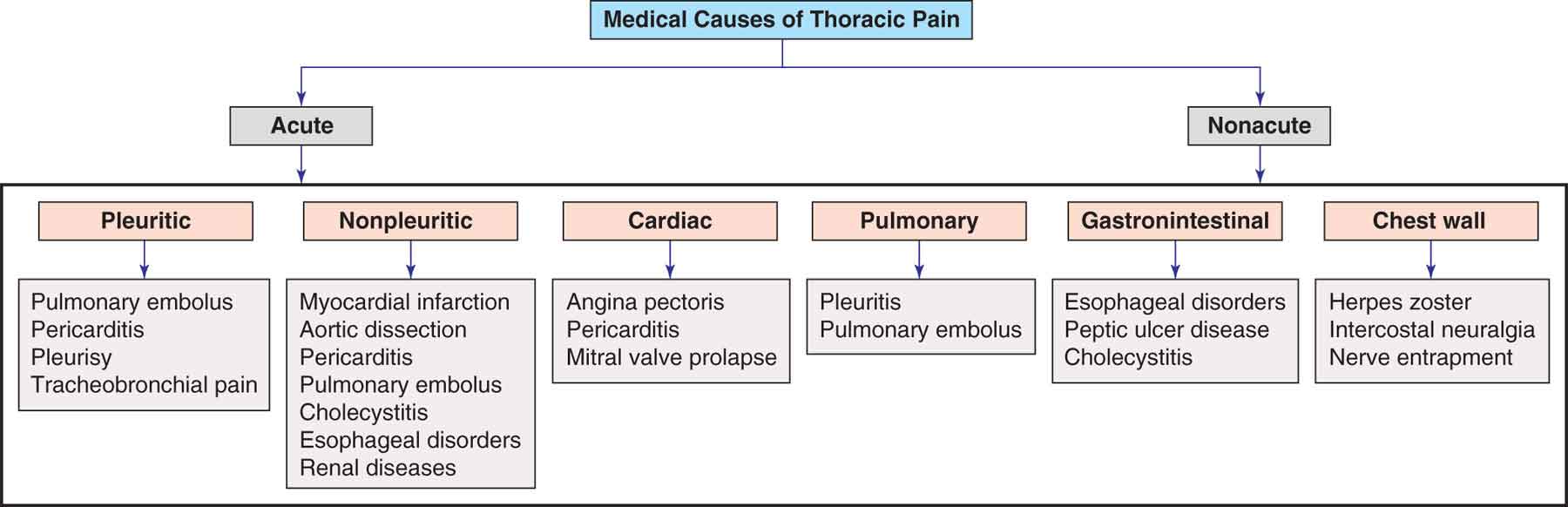
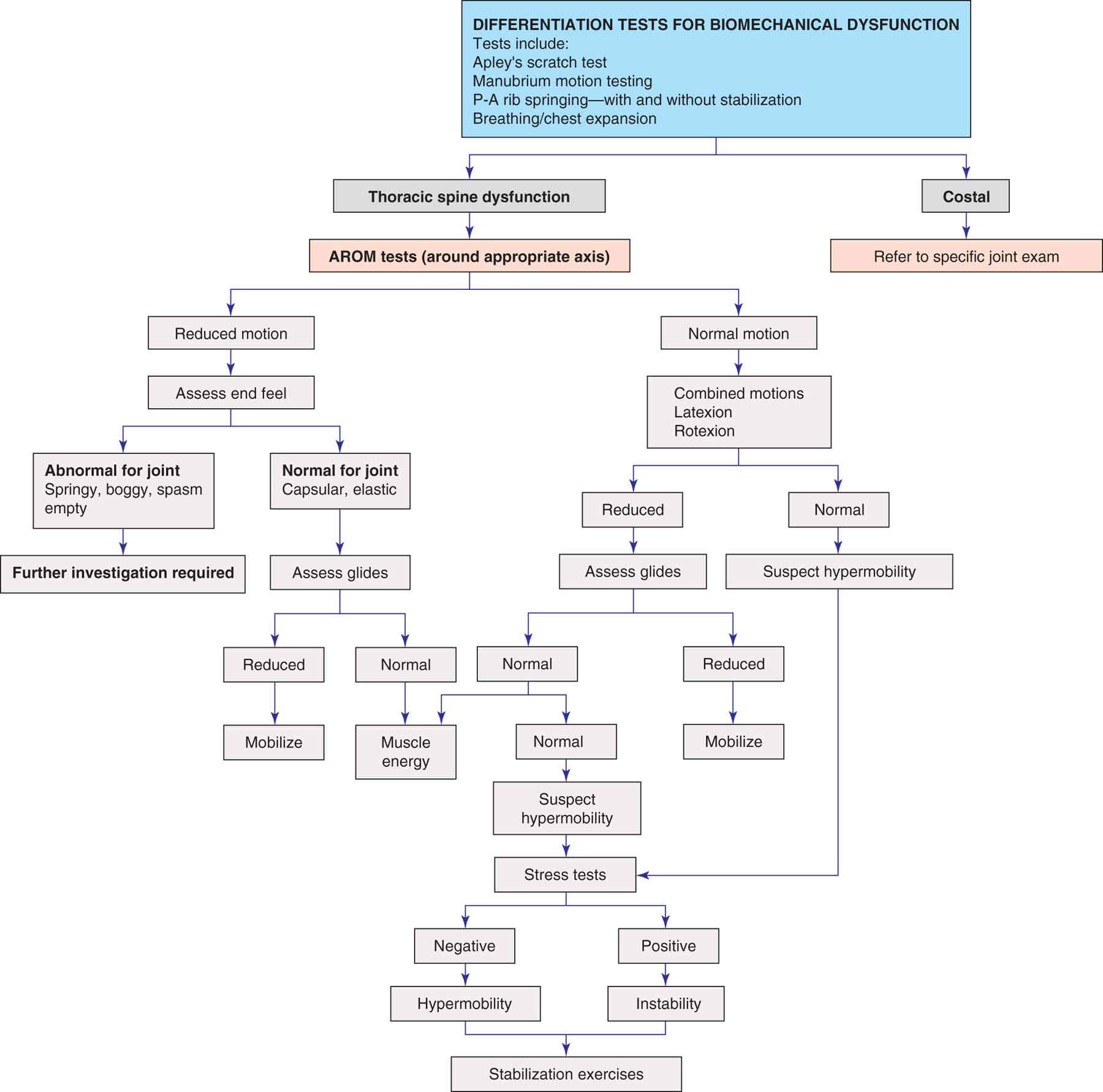
The thoracic spine serves as a transitional zone between the lumbosacral region and the cervical spine. Despite the fact that the thoracic spine has not enjoyed the same attention as other regions of the spine in terms of research, it can be a significant source of local and referred pain. The thoracic spine is the most rigid region of the spine and, in this area, protection of the thoracic viscera takes precedence over segmental spinal mobility. In addition, the thorax is an important region of load transfer between the upper body (the head, cervical spine, and upper extremities) and the lower body (the lumbopelvic region and lower extremities).1,2 As each thoracic vertebra is involved in at least six articulations, and as many as thirteen, establishing the specific cause of thoracic dysfunction may not always be possible. This task is made more difficult because of the inaccessibility of most of these joints.3 The thoracic spine (Fig. 27-1) forms a kyphotic curve between the lordotic curves of the cervical and lumbar spines. The curve begins at T1–2 and extends down to T12, with the T6–7 disk space as the apex.4 The thoracic kyphosis is a structural curve that is present from birth.5 Unlike the lumbar and cervical regions, which derive their curves from the corresponding differences in intervertebral disk (IVD) heights, the thoracic curve is maintained by the wedge-shaped vertebral bodies, which are about 2 mm higher posteriorly than anteriorly. The thoracic spine can be divided into five regions based on anatomical and biomechanical differences. FIGURE 27-1 The thoracic spine and rib cage. (Reproduced, with permission, from Chapter 2. Anterior Thoracic Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The thoracic vertebrae consist of the usual elements: the vertebral body (centrum), transverse processes, and spinous process (Fig. 27-1). The thoracic vertebral body (Fig. 27-1) is roughly as wide as it is long so that its anteroposterior and mediolateral dimensions are of equal length.8 The anterior surface of the body is convex from side to side, whereas the posterior surface is deeply concave.8 The first thoracic vertebra is atypical and has a large, nonbifid spinous process, the superior aspect of which tends to lie in the same transverse plane as the zygapophyseal joints of T1 and T2. On the anterior aspect of the transverse process, there is a deep and concave facet which articulates with the convex facet of the first rib to form the costotransverse joint. The height, end-plate cross-sectional area, and bone mass of the vertebral bodies increase cranially to caudally, particularly in the lower levels.9,10 Progressive wedging of the thoracic vertebral bodies occurs with increasing age in the majority of individuals, with disk space narrowing at multiple levels occurring from the third decade of life.11 The vertebral bodies of most of the thoracic spine differ from those of the cervical and lumbar vertebrae because of the presence of a demifacet on each of their lateral aspects for articulation with the ribs (the costovertebral joint; see later discussion). The IVDs of the thoracic spine have been poorly researched, although preliminary studies seem to indicate that the typical thoracic disk appears to have been adapted from a cervical design rather than from a lumbar design.12 The vertebral bodies of thoracic vertebrae 2–10 increase in size and change shape down the vertebral column and, importantly, each has two demifacets for the attachment of ribs.12 The IVDs of this region are narrower and flatter than those in the cervical and lumbar spine and contribute approximately one-sixth of the length of the thoracic column.13 Disk size in the thoracic region gradually increases from superior to inferior. The disk height to body height ratio is 1:5, compared to 2:5 in the cervical spine, and 1:3 in the lumbar spine,14,15 making it the smallest ratio in the spine and affording the least amount of motion.16 Motion is further restricted by the orientation of the lamella of the annulus fibrosus (AF),17 and the relatively small nucleus pulposus (NP), which is more centrally located within the AF, and has a lower capacity to swell.18 The roughly circular cross-section of the thoracic disk allows the force of torsion to be evenly distributed around its circumference, making it better able to withstand these kinds of forces.19 In the thoracic spine, the segmental nerve roots are mainly situated behind the inferior-posterior aspect of the upper vertebral body rather than behind the disk, which reduces the possibility of root compression in impairments of the thoracic disk.20 In a review of 280 patients, Arce and Dohrmann21 found that thoracic disk herniation constitutes 0.25–0.75% of all disk herniations. Because the intervertebral foramina are quite large at these levels, osseous contact with the nerve roots is seldom encountered in the thoracic spine,20 and, as the dermatomes in this region have a fair amount of overlap, they cannot be relied upon to determine the specific nerve root involved. In contrast to the cervical and lumbar regions, where the spinal canal is triangular/oval in cross-section and offers a large lateral excursion to the nerve roots, the midthoracic spinal canal is small and circular (Fig. 27-1), becoming triangular at the upper and lower levels. At the levels of T4–9, the canal is at its narrowest.20 The spinal canal is also restricted in its size by the pedicles, remaining within the confines of the vertebra and not diverging as they do in the cervical spine. This would tend to predispose the spinal cord to compression more than in the cervical spine, were it not for the smaller cord size and more oval shape of the thoracic canal. Despite this, central disk protrusions are more common in the thoracic region than in other regions of the spine, and, because the NP is small in the thorax, protrusions are invariably of the annular type, and nuclear protrusions are rare.20 Complicating matters is the fact that this is an area of poor vascular supply, receiving its blood from only one radicular artery. This renders the thoracic spinal cord extremely vulnerable to damage by extra dural masses or by an overzealous manipulation. The transverse processes of the thoracic spine are oriented posteriorly (i.e., they point backward) and are located directly between the inferior articulating process and the superior articulating process of the zygapophyseal joints of each level (Fig. 27-1). This anatomical feature makes the transverse processes useful as palpation points, when performing mobility testing in the midthorax. The transverse processes of the first 10 thoracic vertebrae differ from those of the cervical and lumbar spines because of the presence of a costal facet on the transverse process, which articulates with the corresponding rib to form the costotransverse joint (see later discussion). At the T11 and T12 levels, the costotransverse joint is absent because ribs 11 and 12 do not articulate with the transverse processes but rather with the vertebral body. Two short and thick laminae come together to form the spinous process (Fig. 27-1). The spinous processes of the thoracic region are long, slender, and triangular shaped in cross-section. Although all of the thoracic spinous processes point obliquely downward, the degree of obliquity varies. The first three spinous processes and the last three are almost horizontal, whereas those of the midthorax are long and steeply inclined. T7 has the greatest spinous process angulation. As elsewhere in the spine, the thoracic vertebrae are designed to endure and distribute the compressive forces produced by weight bearing, most of which is borne by the vertebral bodies. The compressive load at T1 is approximately 9% of body weight, increasing to 33% at T8 and 47% at T12.22,23 The thoracic vertebrae are classified as typical or atypical, with reference to their morphology. The typical thoracic vertebrae are found at T2–9, although T9 may be atypical in that its inferior costal facet is frequently absent. The atypical thoracic vertebrae are T1, T10, T11, and T12. The first vertebra (T1) resembles C7. The centrum of T1 demonstrates a larger transverse than the anteroposterior dimension of the vertebral body, being almost twice as wide as its length, and the spinous process is usually at least as long as that of C7. There are two ovoid facets on either side of the T1 vertebral body for articulation with the head of the first rib. The inferior aspect of the vertebral body of T1 is flat and contains a small facet at each posterolateral corner for articulation with the head of the second rib. Approximately 32 structures attach to the first rib and body of T1.22,23 Because of the ring-like structure of the ribs, and their attachments both anteriorly and posteriorly, the thoracic spine and ribs can be viewed as a cage-like structure forming a series of concentric rings. Any movement occurring at the various joints of each ring (costovertebral, costotransverse, sternocostal, and zygapophyseal joints) has the potential to influence motions at the other joints within the ring, or at the neighboring segments. The third vertebra is the smallest of the thoracic vertebra. The T9 vertebra may have no demifacets below, or it may have two demifacets on either side (in which case, the T10 vertebra will have demifacets only at the superior aspect). The T10 vertebra has one full rib facet located partly on the body of the vertebra and partly on the tubercle. It does not articulate with the 11th rib and so does not possess any inferior demifacets, and occasionally there is no facet for the rib at the costotransverse joint. The T11 and T12 segments form the thoracolumbar junction. The T11 vertebra has complete costal facets, but no facets on the transverse processes for the rib tubercle. The T12 vertebra only articulates with its own ribs and does not possess inferior demifacets. The common spinal ligaments are present at the thoracic vertebrae, and they perform much the same function as they do elsewhere in the spine. However, the anterior longitudinal ligament in this region is narrower but thicker compared with elsewhere in the spine,8 whereas the posterior longitudinal ligament is wider here at the level of the IVD, but narrower at the vertebral body than in the lumbar region.24 The zygapophyseal joints of the upper thoracic spine show some morphological features of the cervical region, and similarly the joints of the lower thoracic spine progressively approximate those of the upper lumbar region.25 The middle segments of the thoracic spine are designed for less mobility, as the thoracic cage articulations limit sagittal plane motion while accommodating axial displacements.25,26 The superior and inferior facets of the zygapophyseal joints arise from the upper and lower parts of the pedicle of the thoracic vertebra. The superior facet lies superiorly with the articular surface on the posterior aspect, whereas the inferior facet lies inferiorly with the articular surface on the anterior (ventral) aspect. The degree of superoinferior and mediolateral orientation is slight. The superior facet arises from near the lamina–pedicle junction and faces posteriorly, superiorly, and laterally. The inferior articulating facet arises from the laminae to face anteriorly, inferiorly, and medially, lying posterior to the superior facet of the vertebra below. The facet surfaces are concave anteriorly and convex posteriorly, bringing the axis of rotation through the centrum rather than through the spinous process, as in the lumbar vertebrae. This results in the biomechanical center of rotation coinciding with the actual center of rotation formed by body weight.29 The zygapophyseal joints function to restrain the amount of flexion and anterior translation of the vertebral segment and to facilitate rotation.22 They appear to have little influence on the range of side bending.22 The bony thoracic cage is formed by 12 pairs of ribs, the sternum, the clavicle, and the vertebrae of the thoracic spine (Fig. 27-1). The first rib is the shortest of the 12, and the broadest at its anterior end. The primary function of the rib cage is to protect the heart and lungs. All of the ribs of the cage are different from each other in size, width, and curvature, although they share some common characteristics. The rib length increases further inferiorly until the seventh rib, after which they become progressively shorter. Ribs 1–7 are named true ribs because their cartilage attaches directly to the sternum. The remaining ribs are false ribs, so named because their distal attachment is to the costochondral cartilage of their superior neighbor. Ribs 3–9 are typical ribs. The typical rib is characterized by a posterior end, which is composed of a head, neck, and tubercle. The head of the typical rib is characterized as two articular facets, a superior costal facet, and an inferior costal facet. The head of the typical rib projects upward in a very similar manner to that of the uncinate process in the cervical spine and, in fact, develops in much the same way during childhood, appearing to play a similar mechanical role.8 The head consists of a slightly enlarged posterior end, which is divided by a horizontal ridge. The ridge serves as an attachment for the intraarticular ligament. The intraarticular ligament, which travels between the head of the rib and the IVD, bisects the joint into superior and inferior portions. Each of these portions normally contains a demifacet for articulation with the synovial costovertebral joints. The tubercle of the typical rib lies on the outer surface, where the neck joins the shaft and is more prominent in the upper parts than in the lower. The articular portion of the tubercle presents an oval facet for articulation at the costotransverse joint (Fig. 27-1). The convex shaft of the rib is connected to the neck at the rib angle. The upper border of the shaft is round and blunt, whereas the inferior aspect is thin and sharp.8 The anterior end of the shaft has a small depression at the tip for articulation at the costochondral joint. The first, second, tenth, eleventh, and twelfth ribs are considered atypical since they only articulate with their own vertebra via one full facet, and the lower two do not articulate with the costochondrium anteriorly.8 The atypical first rib is small but massively built. Being the most curved and the most inferiorly orientated rib, it slopes sharply downward from its vertebral articulation to the manubrium. The head is small and rounded and articulates only with the T1 vertebra. The first costal cartilage is the shortest and this, together with the fibrous sternochondral joint (Fig. 27-1), contributes to the overall stability of the first ring of the rib cage. The first rib attaches to the manubrium just under the sternoclavicular joint, and the second rib articulates with the sternum at the manubriosternal junction. The atypical second rib is longer and is not as flat as the first rib. It attaches to the junction of the manubrium and the body of the sternum. The atypical 10th rib has only a single facet on its head, because of its lack of articulation with the vertebra above. The 11th and 12th ribs do not present tubercles and have only a single articular facet on their heads. The 11th and 12th ribs remain unattached anteriorly but end with a small piece of cartilage. The attachment of the ribs to the sternum is variable (Fig. 27-1). The upper five, six, or seven ribs have their own cartilaginous connection (see “Sternocostal Joint” section).8 The cartilage of the eighth rib ends by blending with the seventh. The same situation pertains for the ninth and the tenth ribs, thus giving rise to a common band of cartilage and connective tissue. The strong ligamentous attendance, and the presence of the two joints (costovertebral and costotransverse) at each level, severely limits the amount of movement permitted here to slight gliding and spinning motions, with morphology determining the function of each rib. The orientation of the ribs increases from being horizontal at the upper levels to being more downwardly oblique in the inferior levels of the thoracic spine (a point worth remembering when performing palpation). The thoracic vertebrae are connected to their adjacent vertebrae by the bilateral hyalinated, and synovial, costovertebral joints, and their surrounding ligaments (see Fig. 27-1). The costovertebral articulation also forms an intimate relationship between the head of the rib and the lateral side of the vertebral body (see Fig. 27-1). The 1st, 11th, and 12th ribs articulate fully with their own vertebrae via a single costal facet, without any contact with the IVD, while the remaining ribs articulate with both their own vertebra and the vertebra above, as well as to the IVD. This could potentially predispose the 1st, 11th, and 12th costovertebral joints to early arthritic changes, as a result of more mechanical stress compared to the 2nd to the 10th ribs.31 The radiate ligament connects the anterior aspect of the rib head to the bodies of two adjacent vertebrae and their intervening disk in a fanlike arrangement. Each of the three bands of the radiate ligament has different attachments. Oda et al.32 reported that the costovertebral joint and rib cage confer stability on the thoracic spine. They performed symmetrically applied resections of the posterior elements first, followed by resection of the bilateral costovertebral joints and then complete obliteration of the rib cage. Their conclusion was that the thoracic spine may become unstable when the posterior elements and the bilateral costovertebral joints are obliterated. In addition, there is an increase in the neutral zone and range of motion in both side bending and rotation, indicating that these joints provide a stabilizing influence during coupled motions.32 Feiertag et al.33 reported that rib head joint resection showed significant increases in thoracic spinal motion in the sagittal and coronal planes. As the ossification of the head of the rib is not developed at the superior costovertebral joint until about age 13, younger individuals, such as gymnasts, can demonstrate a vast amount of thoracic rotation and side bending. This is a synovial joint located between an articular facet on the posterior aspect of the rib tubercle and an articular facet on the anterior aspect of the transverse process, which is supported by a thin fibrous capsule (see Fig. 27-1). In the lower two thoracic vertebral segments, this articulation does not exist. The neck of the rib lies along the entire length of the posterior aspect of the transverse process. The short and deep costotransverse ligament runs posteriorly from the posterior aspect of the rib neck to the anterior aspect of its transverse process, filling the costotransverse foramen that is formed between the rib neck and its adjacent transverse process. The ligament has two divisions. Very little posteroanterior or anteromedial–posterolateral translation is available at this joint. Jiang et al.34 reported that the superior costotransverse ligaments are very important in maintaining the lateral stability of the spine. The sternum consists of three parts: the manubrium, the body, and the xiphoid process. The manubrium (Fig. 27-1) is broad and thick superiorly and narrower and thinner inferiorly, where it articulates with the body of the sternum. The articulation between the manubrium and the sternum is usually a symphysis, with the ends of the bones being lined with hyaline cartilage. This manubriosternal symphysis remains separate throughout life although ossification can occur. On either side of the suprasternal notch are articulating facets for the clavicles, and below these are the facets for the first rib. On the immediate inferolateral aspects of the manubrium are two more small facets for the cartilage of the second rib. The body of the sternum is made up of the fused elements of four sternal bodies, and the vestiges of these are marked by three horizontal ridges. The upper end of the body articulates with the manubrium at the sternal angle. A facet at the superior end of the body laterally provides a joint surface common with the manubrium for the second costal cartilage. On each lateral border of the sternum are four other notches that articulate with the costal cartilages of the third through sixth ribs. The third rib has the deepest fossa on the sternum, indicating that it may serve as the axis for rotation and side bending during arm elevation. T7 articulates with both the sternum and the xiphoid. The xiphisternum, or xiphoid process (see Fig. 27-1), is the smallest part of the sternum. It begins life in a cartilaginous state, but, in adulthood, the upper part ossifies. A study35 examining the effect of removal of the entire sternum from the intact thorax found that its removal produced an almost complete loss of the stiffening effect of the thorax. The first, sixth, and seventh costal cartilages are each linked to the sternum by a synchondrosis. The second to fifth ribs are each connected to the sternum through a synovial joint, whereby the cartilage of the corresponding rib articulates with a socket-like cavity in the sternum.36 In all of these joints, the periosteum of the sternum and the perichondrium of the costal cartilage are continuous. A thin fibrous capsule, present in the upper seven joints, attaches to the circumference of the articular surfaces, blending with the sternocostal ligaments. The surfaces of the joints are covered with fibrocartilage and are supported by capsular, radiate sternocostal, or xiphocostal and intraarticular ligaments. The joint is capable of about 2 degrees of motion from full inspiration to full expiration and allows the full excursion of the sternum in these activities. A large number of muscles arise from and insert on the thoracic spine and ribs (Fig. 27-2). The muscles of this region can be divided into those that are involved in spinal or extremity motion, and those that are involved in respiration (Tables 27-1 and 27-2). FIGURE 27-2 Muscles of the thoracic spine. (Reproduced, with permission, from Chapter 2. Anterior Thoracic Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) TABLE 27-1 Muscles of Forced Expiration Primary Accessory Abdominal muscles Internal intercostals (posterior) Transversus thoracis Transverse intercostals (intima) Latissimus dorsi Serratus posterior inferior Quadratus lumborum Iliocostalis lumborum Data from Kendall HO, Kendall FP, Boynton DA. Posture and Pain. Baltimore, MD: Williams and Wilkins; 1952. TABLE 27-2 Muscles of Inspiration Primary Accessory Diaphragm Scaleni Levator costarum Sternocleidomastoid External intercostals Trapezius Internal intercostals (anterior) Serratus anterior and posterior and superior and inferior Pectoralis major and minor Latissimus dorsi Subclavius Data from Kendall HO, Kendall FP, Boynton DA. Posture and Pain. Baltimore, MD: Williams and Wilkins; 1952. Spinal Muscles Iliocostalis Thoracis. The iliocostalis thoracis consists of several muscle straps that link the thoracic vertebrae and sacrum with the lower six or seven ribs. The muscle straps have a number of tendons, varying in different individuals, which insert in all angles in the lower six ribs. The function of the muscle is to extend the spine when working bilaterally and to sidebend the spine ipsilaterally when working alone. The iliocostalis consists of three subdivisions—iliocostalis lumborum, iliocostalis thoracis, and iliocostalis cervicis—which are a part of the external portion of the long erector spinae muscle group. The muscle receives its nerve supply by the posterior (dorsal) rami of the thoracic nerves. Longissimus Thoracis. The longissimus thoracis muscles originate with the intercostalis muscles from the transverse processes of the lower thoracic vertebrae. They insert into all of the ribs and into the ends of the transverse processes of the upper lumbar vertebrae. The function of the muscle is to extend the spine when working bilaterally and to side bend the spine ipsilaterally when working alone. The muscle is innervated by the posterior (dorsal) rami of the thoracic nerves. Spinalis Thoracis. The spinalis thoracis muscle (spinalis dorsi) originates from the spinous processes of the upper lumbar and two lower thoracic vertebrae. It inserts in the spinous processes of the middle and upper thoracic vertebrae. The function of the muscle is to extend the spine. The muscle is innervated by the posterior (dorsal) rami of the thoracic nerves. Semispinalis Thoracis. The semispinalis thoracis consists of long straps of muscle that stretch along and surround the vertebrae of the spine. The muscle can have between four and eight upper ends, which originate from the transverse processes of the T6–10. These straps of muscle insert in the spinous processes of the first four thoracic and fifth and seventh processes of C6–T4. The function of the muscle is to extend the spine when working bilaterally and to rotate the spine contralaterally when working alone. The semispinalis thoracis is innervated by the posterior (dorsal) rami of the thoracic nerves. Multifidus. The multifidus is a deep back muscle that runs along the entire spine and lies deep to the erector spinae muscles. It originates from the sacrum, sacroiliac ligament, mammillary processes of the lumbar vertebrae, transverse processes of the thoracic vertebrae, and the articular processes of the last four cervical vertebrae. The multifidus consists of numerous bundles of fibers that cross over two to five vertebrae at a time and insert into the entire length of the spinous process above. The function of the muscle is to extend the spine when working bilaterally and to rotate the spine minimally contralaterally when working alone. The thoracic multifidus is innervated by the posterior (dorsal) rami of the thoracic spinal nerves. Rotatores Thoracis (Longus and Brevis). The rotatores muscles are deep spinal muscles that lie beneath the multifidus muscles. The rotatores brevis muscle lies just deep to the rotatores longus muscle. The rotatores muscles are the best developed in the thoracic region. There are a total of 11 small, quadrilateral rotatores muscles on each side of the spine. Each muscle arises from the transverse process of the vertebra and extends inward to the vertebra above. The rotatores muscles help rotate the appropriate thoracic segment. They are innervated by posterior (dorsal) rami of the thoracic spinal nerves. Intertransversarii. The intratransversals are small muscles located between the transverse process of the vertebrae. In the thoracic region, they are single-bellied muscles and exist only from T10–11 to T12–L1. The function of the muscle is to sidebend the spine ipsilaterally. The muscle is innervated by the posterior (dorsal) rami of the thoracic spinal nerves. The other spinal muscles of the thoracic region act primarily on the cervical spine. These include the trapezius, levator scapulae, and anterior, posterior, and middle scalenes (see Chapter 25). Extremity Muscles. The muscles of the thoracic region that act primarily on the extremities include the pectoralis major, latissimus dorsi, and serratus anterior (see Chapter 16). The respiratory system is essentially a robust, multimuscle pump (Fig. 27-3). Connections to the respiratory mechanism have been found to exert a strong influence on such areas as the shoulder and pelvic girdles, as well as the head and neck. The primary task of the respiratory muscles is to displace the chest wall and, therefore, move gas in and out of the lungs to maintain arterial blood gas and pH homeostasis. The importance of normal respiratory muscle function can be appreciated by considering that respiratory muscle failure caused by fatigue, injury, or disease could result in an inability to maintain blood gas and pH levels within an acceptable range, which could have lethal consequences. Restoration of the respiratory mechanism is, thus, an essential element of thoracic intervention. FIGURE 27-3 Components of the respiratory system. (Reproduced, with permission, from Chapter 3. Lungs. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The actions of various respiratory muscles, which are broadly classified as inspiratory or expiratory, based on their mechanical actions, are highly redundant and provide several means by which air can be effectively displaced under a host of physiologic and pathophysiologic conditions.37,38 At rest, movement of air into and out of the lungs is the result of the recruitment of several muscles,39–41 and the expiratory phase of breathing at rest is also associated with active muscle participation.41 In a resting man, the tidal volume is the result of the coordinated recruitment of the diaphragm, the parasternal intercostal, and the scalene muscles (Tables 27-1 and 27-2).43,44 Although some have argued that the performance of the respiratory muscles does not limit exercise tolerance in normal healthy adults,45,46 heavy or prolonged exercise has been shown to impair respiratory muscle performance in humans.47,48 Thus, an interest in the adaptability of respiratory muscles to endurance-type exercise has grown significantly during the last decade. The primary muscles of respiration include the diaphragm, the sternocostal, and the intercostals. The secondary muscles of respiration are the anterior/medial scalenes, serratus posterior, pectoralis major and minor, and, with the head fixed, the sternocleidomastoid.8 Anatomically, the diaphragm muscle may be divided into sternal, costal, and lumbar parts. Functionally and metabolically, the diaphragm can be classified as two muscles.49,50 Thus, the muscle is attached around the thoracoabdominal junction circumferentially. From these attachments, the fibers arch toward each other centrally to form a large tendon. Contraction of the diaphragm pulls the large, central tendon inferiorly, producing diaphragmatic inspiration (see later discussion). The diaphragm has a phrenic C3–4 motor innervation and sensory supply by the lower six intercostal nerves. Between the ribs are the intercostal spaces, which are deeper both in front and between the upper ribs. Between the ribs lie the internal and external intercostal muscles, with the neurovascular bundle lying beneath each rib. The intercostal muscles, together with the sternalis (or sternocostalis or transversalis thoracis), phylogenically form from the hypomeric muscles. These muscles correspond to their abdominal counterparts, with the sternalis being homologous to the rectus abdominis, and the intercostals homologous to the external oblique.8 External Intercostals. The external intercostal muscles (Fig. 27-2), of which there are 11, are laid in a direction that is superoposterior to inferoanterior (run inferiorly and medially in the front of the thorax and inferiorly and laterally in the back). Because of the oblique course of the fibers, and the fact that leverage is greatest on the lower of the two ribs, the muscle pulls the lower rib toward the upper rib, which results in inspiration. The external intercostals attach to the lower border of one rib and the upper border of the rib below, extending from the tubercle to the costal cartilage. Posteriorly, the muscle is continuous with the posterior fibers of the superior costotransverse ligament. The action of the external intercostals is believed to be entirely inspiratory,43 although the muscles also counteract the force of the diaphragm, preventing the collapse of the ribs.40 Innervation of this muscle is supplied by the adjacent intercostal nerve. Internal Intercostals. The internal intercostals (see Fig. 27-2), which also number 11, have their fibers in an inferoposterior to a superoanterior direction. The internal intercostals are found deep to the external intercostals and run obliquely, and perpendicular, to the externals. The posterior fibers pull the upper rib down, but only during enforced expiration.40,43 The internal intercostals extend from the posterior rib angles to the sternum, where they end posteriorly. They are continuous with the internal membrane, which then becomes continuous with the anterior part of the superior costotransverse ligament. Innervation of this muscle group is supplied by the adjacent intercostal nerve. Transverse Intercostals (Intima). The deepest of the intercostals, the transverse intercostals are attached to the internal aspects of two contiguous ribs. They become progressively more significant and developed, further down the thorax. This muscle is used during forced expiration.40,43 Transversus Thoracis. The transversus thoracis is a triangular-shaped sheet muscle, which originates from the posterior (dorsal) surface of the sternum and covers the inner surfaces of both the sternum and the second to eighth sternal costal cartilages. The apex of the muscle points cranially, with muscle slips running inferolaterally and eventually inserting on the sternal ribs quite close to the costochondral junctions. Morphologically, the transversus thoracis is similar to the anterior (ventral) part of the transversus abdominis. Its function is to draw the costal cartilages down. The muscle is innervated by the adjacent intercostal nerves. These consist of 12 strong short muscles that turn obliquely (inferolaterally), parallel with the external intercostals, from the tip of the transverse process to the angle of the rib, extending from C7 to T11 transverse processes. These muscles, which are innervated by the lateral branch of the posterior (dorsal) ramus of the thoracic nerve, function to raise the rib, but their importance in respiration is argued. The levator costae may also be segmentally involved in rotation and side bending of the thoracic vertebra. The serratus posterior superior runs from the lower part of the ligamentum nuchae, the spinous processes of C7 and T1–3, and their supraspinous ligaments, to the inferior border of the second through fifth ribs, lateral to the rib angle. The muscle receives its nerve supply from the second through fifth intercostal nerves. Its function is unclear, but it is thought to elevate the ribs.8 This muscle arises from the spines and supraspinous ligaments of the two lower thoracic and the two or three upper lumbar vertebrae. It attaches to the inferior border of the lower four ribs, lateral to the rib angle. The muscle receives its nerve supply from the anterior (ventral) rami of the 9th through 12th thoracic nerves. Its function is unclear, but it is thought to pull the ribs downward and backward. The blood supply to this region is provided mainly by the posterior (dorsal) branches of the posterior intercostal arteries (Fig. 27-4) while the venous drainage occurs through the anterior and posterior venous plexuses. The spinal cord region between T4 and T9 is poorly vascularized.51 FIGURE 27-4 Vasculature of the thoracic region. (Reproduced, with permission, from Chapter 2. Anterior Thoracic Wall. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The spinal canal in this region is narrow, with only a small epidural space between the cord and its osseous environment.51 Innervation of the thoracic spinal canal is by the sinuvertebral nerve, which arises from the nerve root and reenters the epidural space. The thoracic spinal cord is unusually susceptible to injury because it occupies a greater percentage of the total cross-sectional area of its surrounding spinal canal than do the cervical or lumbar sections of the spinal cord, and the thoracic cord is tightly packed in the canal and easily injured by displaced fragments of bone or disk material.52 Furthermore, the blood supply of the midthoracic spinal cord is tenuous, and seemingly trivial injuries can disrupt the blood supply to a substantial portion of the thoracic cord and result in devastating neurologic deficits.53 In the thoracic region, there is great variability in the topography of the nerves and the structures that they serve.54 Typically, the spinal root arises from the lateral end of the spinal nerve but, in 25% of cases, the spinal root is made up of two parts that arise from the superior border of the spinal nerve.55 The thoracic spinal nerves are segmented into posterior (dorsal) primary and anterior (ventral) primary divisions (see Chapter 3). As elsewhere, the dermatomes of this region are considered to represent the cutaneous region innervated by one spinal nerve through both of its rami.56 The peripheral nerves, which travel through the thoracic spine and chest wall, include the posterior (dorsal) scapular, thoracodorsal, and long thoracic nerves (see Chapter 3). Knowledge of the regional biomechanics of the thoracic spine and rib cage assists the clinician in the interpretation of active movement and motion palpation examination in relation to the patient’s symptoms.57 The thoracic spinal segments possess the potential for a distinctive array of movements. Most of the understanding with regard to the biomechanics of the thoracic spine is based largely on the ex vivo studies of White,21 and Panjabi et al.,1,58 and a variety of ‘clinical models.28,59 In addition, although normative ranges of spinal motion have been reported for the lumbar spine, no such reliable data exists for the thoracic region.60 It is widely recognized that the mechanical behavior of the spine is influenced by load.61 Axial load has been shown to increase motion segment stiffness and decrease mobility. In addition, due to the modifying influence of the cage-like structure of the ribs, which provide a significant degree of stability,34 and the kyphotic shape of the curve, the biomechanics of the thoracic spine is considerably different from those of the lumbar and cervical regions. The increased stability/reduced mobility of the thoracic segments has been reported to produce three primary effects.23,62 Other biomechanical studies have investigated the stabilizing effects of the individual components of the thoracic spine.32,66 Flexion of the thoracic spine in weight bearing is initiated by the abdominal muscles and, in the absence of resistance, is continued by gravity, with the spinal erector muscles eccentrically controlling the descent. Flexion may also occur during bilateral scapular protraction. There are about 4–5 degrees of flexion available at the upper thoracic levels, 6–8 degrees in the middle layers, and 9–15 degrees in the lower levels,22 giving an overall total range for thoracic flexion of 20–45 degrees.67 End-range flexion is resisted by the posterior half of annulus and by the impaction of the zygapophyseal joints. According to Lee,28 flexion of the cervicothoracic region consists of an anterior rotation of the head of the rib and a superoanterior glide of the zygapophyseal joints, whereas extension and arm elevation in this region consists of a posterior sagittal rotation and posterior translation of the superior vertebra. This latter action pushes the superior aspect of the head of the rib posteriorly at the costovertebral joint, producing a posterior rotation of the rib (the anterior aspect travels superiorly, while the posterior aspect travels inferiorly).28 In the remainder of the thorax, flexion results from the superior facets (i.e., the inferior articular processes of the superior vertebra of the segment) gliding superiorly and anteriorly (Table 27-3).28 This motion at the zygapophyseal joint is accompanied by an anterior translation of the superior vertebra, and a slight distraction of the centrum. It seems likely that the anterior vertebral translation produces a similar motion in the ribs, with a superior glide occurring at the costotransverse joint. During this motion, the anterior aspects of the ribs approximate each other, while the posterior aspects separate. TABLE 27-3 Biomechanics of the Thorax Motions Z Joint Rib Motion Costotransverse Joint Vertebromanubrial (T1–2) Flexion Superoanterior glide Anterior rotation NA Extension Inferoposterior glide Posterior rotation NA Latexion Ipsilateral coupling NA NA Rotexion Ipsilateral coupling NA NA Inspiration NA Elevation NA Expiration NA Depression NA Vertebrosternal (T3–7) Flexion Superoanterior glide Varies (very mobile) anteroposterior rotation Superior–inferior glide (varies) Extension Posteroinferior glide Varies (very mobile) anteroposterior rotation Superior–inferior glide (varies) Latexion Ipsilateral side bend and contralateral rotation Ipsilateral—anterior rotation Contralateral—posterior rotation Ipsilateral—superior glide Contralateral—inferior glide Rotexion Ipsilateral side bend and ipsilateral rotation Ipsilateral—posterior rotation Contralateral—anterior rotation Ipsilateral—inferior glide Contralateral—superior glide Inspiration NA Posterior rotation bilaterally Inferior glide Expiration NA Anterior rotation bilaterally Superior glide Vertebrochonral (T8–10) Flexion Superoanterior glide Anterior rotation SMP glide Extension Inferoposterior glide Posterior rotation ILA glide Latexion Varies NA Apex in line with trochanter Ipsilateral—SMP Contralateral—ILA If not, the reverse occurs Rotexion Ipsilateral—inferior glide Contralateral—superior glide NA Ipsilateral—ILA, then anteromedial Contralateral—SMP, then posterolateral glide Inspiration NA NA ILA glide Expiration NA NA SMP glide NA, not applicable; SMP, superior medial posterior; ILA, inferior lateral anterior. Studies have shown that the thoracic zygapophyseal facets play an important role in stabilization of the thoracic spine during flexion loading.58,68 Extension of the thoracic spine is produced principally by the lumbar extensors and results in an inferior glide of the superior facet of the zygapophyseal joint (see Table 27-3). One to two degrees of extension is available at each thoracic segment, giving an overall average of 15–20 degrees of thoracic extension for the entire thoracic spine. Extension of the thoracic spine is restrained by the relative stiffness of the anterior IVD; the anterior longitudinal ligament; bony contact of the posterior elements, including the inferior facet onto the lamina below; and the spinous processes.23,58 Given the location of the axis of rotation of extension, which is close to the moving segment, more translation than rotation occurs during extension.69 The joint motions occurring with extension are essentially the opposite of those of flexion. The translation of the vertebra occurs in a posterior direction, with an accompanying slight compression of the centra. The posterior translation that occurs with extension is controlled by the posteriorly directed lamellae of the annulus, and by the capsule of the zygapophyseal joint. The transitional region between the thoracic and lumbar spines can produce an inflexion point that may serve to reduce the bending forces in the sagittal plane.6 However, stiffness in this area also may result in the thoracic spine pivoting over the thoracolumbar region, thereby increasing the risk of compression fracture (see Chapter 5).70 In addition to those motions occurring at the zygapophyseal joints and the vertebral body during thoracic extension, the motion also occurs at the rib articulations. The ribs rotate posteriorly, with the posterior aspects approximating and the anterior aspects separating, and an inferior glide occurs at the costotransverse joint.28 Side bending of the thoracic spine is initiated by the ipsilateral abdominals and erector muscles and then continued by gravity. A total of 25–45 degrees of side bending is available in the thoracic spine, at an average of about 3–4 degrees to each side per segment, with the lower segments averaging slightly more, at 7–9 degrees, each.22,74 At the zygapophyseal joints, the primary motion involves the ipsilateral superior facet gliding inferiorly, and the contralateral gliding superiorly (see Table 27-3). In effect, the ipsilateral zygapophyseal joint extends while the contralateral flexes. Side bending is restrained by the compression of the IVD and approximation of the ribs. Side bending in the upper thoracic spine is associated with ipsilateral rotation and ipsilateral translation.75 According to Lee,28 the coupling that occurs in the rest of the thoracic spine depends on which of the two coupling motions initiates the movement. If side bending initiates the movement, it is called latexion, and the biomechanics consist of side bending, contralateral rotation, and ipsilateral translation. The mechanism of this coupling, or actually tripling, is not certain, and one must guard against strong conclusions. The postulated mechanism is as follows: with side bending, a contralateral convex curve is produced. This causes the ribs on the convex side of the curve to separate and those on the concave side to approximate.28 Trunk side bending is essentially halted, by soft-tissue tension or rib approximation, or both, and the ribs become fixed. Further side bending is modified by the fixed ribs.28 The ipsilateral articular facet of the transverse process glides inferiorly on its rib, resulting in a relative anterior rotation of the neck of the rib, while the contralateral transverse process glides superiorly, producing a posterior rotation of the rib neck.28 The effect of these bilateral rib rotations is to force the superior vertebra into rotation away from the direction of side bending. The axis of rotation for the thoracic spine varies according to the vertebral level.76 The axis of rotation lies within the vertebral body in the midthoracic joints, but anterior to the vertebral body in the upper and lower joints.76 Almost pure rotation can occur in the midthoracic region, whereas, in the upper and lower segments, rotation can be associated with side bending to either side (see Table 27-3). Axial rotation (rotexion) is produced either by the abdominal muscles and other trunk rotators or by the unilateral elevation of the arm. Pure axial rotation (twisting) can only occur at two points in the spine: at the thoracolumbar and cervicothoracic junctions. A total of 35–50 degrees of rotation is available in the thoracic spine.22,74 Segmental axial rotation in the thoracic spine averages 7 degrees in the upper thoracic area, approximately 5 degrees in the middle thoracic spine, and 2–3 degrees in the last two or three segments.22,67,77 Torsional stiffness is enhanced in the thoracolumbar region by the mortise-type morphology of the zygapophyseal joints and the near sagittal alignment of the upper lumbar articulations.23,27,64,70,78 According to MacConnail and Basmajian,29 thoracic segmental rotation is coupled with contralateral side bending and contralateral translation. However, this finding deviates from what is generally observed clinically, where the coupling of rotation and side bending that occurs seems to depend on the segmental level and the integrity of the joint. The ribs function as levers, with the fulcrum represented by the rib angle, the effort arm represented by the neck, and the load arm represented by the shaft. Because of the relatively small size of the rib neck, a small movement at the rib neck will produce a large degree of movement in the shaft. The shapes of the articular facets of the upper six ribs would suggest that the upward and downward gliding movements that occur would produce spinning of the neck of the rib. In fact, the main movement in the upper six ribs during respiration and other movements is one of the rotations of the neck of the rib, with only small amounts of superior and inferior motion. In the seventh through tenth ribs, the principal movement is upward, backward, and medially during inspiration, with the reverse occurring during expiration.28 Because the anterior end of the ribs is lower than the posterior, when the ribs elevate, they rise upward, while the rib neck drops down. In the upper ribs, this results in an anterior elevation (pump handle) and in the middle and lower ribs (excluding the free ribs), a lateral elevation (bucket handle), with the former movement increasing the anteroposterior diameter of the thoracic cavity and the latter increasing the transverse diameter (Fig. 27-5). FIGURE 27-5 Bucket and pump handle rib motions. (Reproduced, with permission, from Chapter 3. Lungs. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) Both kinds of rib motion are produced by the action of the diaphragm. The seventh through tenth ribs act to increase the abdominal cavity free space to afford space for the descending diaphragm. As the ends of these ribs are elevated, they push up on each other, lifting each successive rib upward and finally lifting the sternum. The two lower ribs are depressed by the quadratus lumborum to provide a stable base of action for the diaphragm. Quiet respiration involves very little zygapophyseal joint motion. During inspiration, the diaphragm descends and pulls the central tendon inferiorly through the fixed 12th ribs and L1–3 (Fig. 27-6). When the maximum extensibility (distention) of the abdominal wall is reached, the central tendon becomes stationary. Further contraction of the diaphragm produces an elevation and posterior rotation of the lower six ribs, with torsion of the anterior costal cartilage, and an anterosuperior thrust of the sternum (and eventually the inferior aspect of the manubrium). FIGURE 27-6 Biomechanics of respiration. (Reproduced, with permission, from Chapter 3. Lungs. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) During inspiration in the normal population, because the second rib is longer than the first, the superior aspect of the manubrium is forced to tilt posteriorly as its inferior edge is moved anteriorly. As the top of the manubrium tilts back, the clavicle rolls anteriorly. Because the lower ribs are longer, the inferior sternum moves further anteriorly than the superior section during inspiration. The manubriosternal junction acts as the hinge for this motion. If this joint stiffens or ossifies, respiratory function will suffer. In addition, if the central tendon stiffens, inspiration will have to be accomplished, with the ribs moving laterally. Forced inspiration produces an increase in the activity level of the diaphragm, intercostals, scaleni, and quadratus lumborum. In addition, new activity occurs in the sternocleidomastoid, trapezius, both pectorals and serratus anterior. During inspiration, the ribs move with the sternum in an upward and forward direction, increasing the anteroposterior diameter of the chest while posteriorly rotating. The tubercles and costotransverse joints of28 Quiet expiration occurs passively (Fig. 27-6). During forced expiration, there is activity in a number of muscles (Table 27-1). During expiration, the ribs rotate anteriorly and the tubercles and costotransverse joints of28 It may be possible to detect a subluxation of the costotransverse joints by palpating the ipsilateral transverse process and rib during inspiration and thoracic side bending.28 For example, a superior subluxation of the right rib may produce the following: The findings for other rib dysfunctions are outlined in Table 27-4. TABLE 27-4 Rib Dysfunctions Dysfunction Rib Angle Intercostal Space Anterior Rib Thoracic Findings Anterior subluxation Less prominent Tender NA More prominent Posterior subluxation More prominent Tender NA Less prominent External rib torsion Prominent and tender superior border Wide above and narrow below ERS, ipsilateral at the level above NA Internal rib torsion Prominent and tender inferior border Narrow above and wide below FRS, contralateral at the level above NA ERS, extended, rotated, and side flexed; FRS, flexed, rotated, and side flexed; NA, not applicable. Data from Bookhout MR. Evaluation of the thoracic spine and rib cage. In: Flynn TW, ed. The Thoracic Spine and Rib Cage: Musculoskeletal Evaluation and Treatment. Boston, MA: Butterworth-Heinemann; 1996:147–167. Differential diagnosis of thoracic pain can be difficult. This is due to the complicated biomechanics and function of the region, the proximity to vital organs, and the many articulations. Bogduk79 has cited the following anatomical structures as possible causes of thoracic spine pain: posterior thoracic muscles, spinous processes, anterior and posterior longitudinal ligaments, vertebral bodies, zygapophyseal and costotransverse joints, inferior articular process, pars interarticularis, IVD, nerve root, joint meniscus, and dura mater. Pain arising from inflammation of the axial spine can mimic a variety of serious conditions, including cardiac/pulmonary pathology, renal colic, fracture, a tumor, or numerous visceral and retroperitoneal abnormalities, including abdominal aortic aneurysm.80 The thoracic spine is less commonly implicated in musculoskeletal pain syndromes than the lumbar and cervical spines, and when it does occur, there is some disagreement as to whether the ribs or the intervertebral joints are the major sources of the biomechanical dysfunction. Complicating matters is the fact that pain arising from the thoracic spinal joints has considerable overlap and can refer symptoms to distal regions (groin, pubis, and lower abdominal wall) (refer to Chapter 5). Apart from musculoskeletal lesions, the thoracic spine is also a common source of systemic pain, and the phenomenon of referred pain poses more diagnostic difficulties in the thoracic spine than in any other region of the vertebral column (Fig. 27-7).79 The algorithm outlined in Figure 27-8 can serve as a guide to the examination of the thoracic spine and ribs. FIGURE 27-7 Medical causes of thoracic symptoms. FIGURE 27-8 Thoracic spine examination algorithm. The history should include the chief complaints and a pain drawing. Referred chest pain patterns are outlined in Table 27-5. In addition to those questions listed under History in Chapter 4, the following questions should be asked by the clinician: TABLE 27-5 Chest Pain Patterns Origin of Pain Site of Referred Pain Type of Disorder Substernal or retrosternal Neck, jaw, back, left shoulder and arm, and abdomen Angina Substernal, anterior chest Neck, jaw, back, and bilateral arms Myocardial infarction Substernal or above the sternum Next, upper back, upper trapezius, supraclavicular area, left arm, and costal margin Pericarditis Anterior chest (thoracic aneurysm); abdomen (abdominal aneurysm) Posterior thoracic, chest, neck, shoulders, interscapular, or lumbar region Dissecting aortic aneurysm Variable Variable, depending on structures involved. Musculoskeletal Costochondritis (inflammation of the costal cartilage): sternum and rib margins. Abdominal oblique trigger points: pain referred up into the chest area. Upper rectus abdominis trigger points (left side), pectoralis, serratus anterior, and sternalis muscles: precordial pain Pectoralis trigger points: pain referred down medial bilateral arms along ulnar nerve distribution (fourth and fifth fingers) Precordium region (upper central abdomen and diaphragm) Sternum, axillary lines, and either side of vertebrae; lateral and anterior chest wall; occasionally to one or both arms Neurological Substernal, epigastric, and upper abdominal quadrants Around chest area, shoulders, and upper back region Gastrointestinal Within breast tissue; may be localized in pectoral and supraclavicular regions Chest area, axilla, mid-back, and neck and posterior shoulder girdle Breast pain Commonly substernal and anterior chest region No referred pain Anxiety Data from Donato EB. Physical examination procedures to screen for serious disorders of the head, neck, chest, and upper quarter. In: Wilmarth MA, ed. Medical Screening for the Physical Therapist. Orthopaedic Section Independent Study Course 14.1.1. La Crosse, WI: Orthopaedic Section, APTA, Inc., 2003:1–43; Goodman CC, Boissonnault WG. Pathology: Implications for the Physical Therapist. Philadelphia, PA: WB Saunders; 1998.
CHAPTER 27
The Thoracic Spine
OVERVIEW
ANATOMY
 Cervicothoracic: This region comprises the C7–T1 segment and the first rib.
Cervicothoracic: This region comprises the C7–T1 segment and the first rib.
 Vertebromanubrial: This region, which has a slight overlap with the cervicothoracic region, includes the first two thoracic vertebrae, ribs 1 and 2, and the manubrium.
Vertebromanubrial: This region, which has a slight overlap with the cervicothoracic region, includes the first two thoracic vertebrae, ribs 1 and 2, and the manubrium.
 Vertebrosternal: This region includes T3–7, the third to seventh ribs, and the sternum.
Vertebrosternal: This region includes T3–7, the third to seventh ribs, and the sternum.
 Vertebrochondral: This region includes T8–10, together with the 8th, 9th, and 10th ribs.
Vertebrochondral: This region includes T8–10, together with the 8th, 9th, and 10th ribs.
 Thoracolumbar. This region includes T11 and T12, and the 11th and 12th ribs. At the thoracolumbar junction, typically located between T11 and L1, the changes in curvature from one of kyphosis to one of lordosis vary quite widely according to posture, age, and previous compression fractures (see Chapter 5) and resulting deformity.6,7
Thoracolumbar. This region includes T11 and T12, and the 11th and 12th ribs. At the thoracolumbar junction, typically located between T11 and L1, the changes in curvature from one of kyphosis to one of lordosis vary quite widely according to posture, age, and previous compression fractures (see Chapter 5) and resulting deformity.6,7
Thoracic Vertebra
Vertebral Body
Intervertebral Disk
Transverse Processes
Spinous Processes
Ligaments
Zygapophyseal Joints
Ribs
Typical Ribs
Atypical Ribs
Attachment and Orientation of the Ribs
Costovertebral Joint
Costotransverse Joint
Sternum
Sternocostal Joint
Muscles
 Internal and external oblique
Internal and external oblique
 Rectus abdominis
Rectus abdominis
 Transversus abdominis
Transversus abdominis
Spinal and Extremity Muscles
Respiratory Muscles
Diaphragm
 The sternal fibers originate from two slips at the back of the xiphoid process.
The sternal fibers originate from two slips at the back of the xiphoid process.
 The costal fibers originate from the lower six ribs and their costal cartilages.
The costal fibers originate from the lower six ribs and their costal cartilages.
 The lumbar fibers originate from the crura of the lumbar vertebra, and the medial and lateral arcuate ligaments.
The lumbar fibers originate from the crura of the lumbar vertebra, and the medial and lateral arcuate ligaments.
Intercostals
Levator Costae
Serratus Posterior Superior
Serratus Posterior Inferior
Vascular Supply
Neurology
BIOMECHANICS
 The IVD can be regarded as the most important stabilizer in the thoracic functional unit mechanics.
The IVD can be regarded as the most important stabilizer in the thoracic functional unit mechanics.
 The rib head joints serve as stabilizing structures to the human thoracic spine under flexion–extension, side bending, and axial rotation loading, and resection after diskectomy increases range of motion by approximately 80% under all loading modes.
The rib head joints serve as stabilizing structures to the human thoracic spine under flexion–extension, side bending, and axial rotation loading, and resection after diskectomy increases range of motion by approximately 80% under all loading modes.
 The lateral portion of the facet joints plays an important role in providing spinal stability.
The lateral portion of the facet joints plays an important role in providing spinal stability.
 In the thoracic spine, total resection of the posterior ligamentous complex leads to an approximately 40% increase in the range of motion under flexion–extension, side bending, and axial rotation loading.
In the thoracic spine, total resection of the posterior ligamentous complex leads to an approximately 40% increase in the range of motion under flexion–extension, side bending, and axial rotation loading.
Flexion
Extension
Side Bending
Rotation
Respiration
Inspiration
 T1–7 glide inferiorly;
T1–7 glide inferiorly;
 T8–10 glide in an anterolateral and inferior direction; and
T8–10 glide in an anterolateral and inferior direction; and
 T11 and T12 remain stationary, except for slight caliper motion increasing the lateral dimension.
T11 and T12 remain stationary, except for slight caliper motion increasing the lateral dimension.
Expiration
 T1–7 glide superiorly;
T1–7 glide superiorly;
 T8–10 glide in a posteromedial and superior direction; and
T8–10 glide in a posteromedial and superior direction; and
 T11 and T12 remain stationary, except for slight caliper motion decreasing the lateral dimension.
T11 and T12 remain stationary, except for slight caliper motion decreasing the lateral dimension.
 A decreased inferior glide of the rib
A decreased inferior glide of the rib
 A decreased thoracic motion in the directions of left side bending and right rotation
A decreased thoracic motion in the directions of left side bending and right rotation
EXAMINATION
History
 Was there a mechanism of injury? Any information regarding the onset is important. For example, most rib injuries are commonly caused by direct trauma. If there was no mechanism of injury, a disease process such as scoliosis could be indicated. Costovertebral and costotransverse joint hypomobility and active trigger points are possible sources of upper thoracic pain.81
Was there a mechanism of injury? Any information regarding the onset is important. For example, most rib injuries are commonly caused by direct trauma. If there was no mechanism of injury, a disease process such as scoliosis could be indicated. Costovertebral and costotransverse joint hypomobility and active trigger points are possible sources of upper thoracic pain.81
 Do the symptoms occur with breathing? Symptoms reproduced with respiration could indicate a rib dysfunction or pleuritic pain. If the symptoms are aggravated on exertion, the clinician should focus on the relationship of specific movements or activities. Any information regarding the onset, as well as aggravating factors, is important, especially if the pain appears only during certain positions or movements, which would suggest a musculoskeletal lesion. Deep breathing or arm elevation tends to aggravate a rib dysfunction.
Do the symptoms occur with breathing? Symptoms reproduced with respiration could indicate a rib dysfunction or pleuritic pain. If the symptoms are aggravated on exertion, the clinician should focus on the relationship of specific movements or activities. Any information regarding the onset, as well as aggravating factors, is important, especially if the pain appears only during certain positions or movements, which would suggest a musculoskeletal lesion. Deep breathing or arm elevation tends to aggravate a rib dysfunction.
 Are the symptoms provoked or alleviated with movement or posture? This type of history indicates a musculoskeletal dysfunction. Chronic problems in this area tend to result from postural dysfunctions. The pain of a mechanical origin tends to worsen throughout the day but is relieved with rest.
Are the symptoms provoked or alleviated with movement or posture? This type of history indicates a musculoskeletal dysfunction. Chronic problems in this area tend to result from postural dysfunctions. The pain of a mechanical origin tends to worsen throughout the day but is relieved with rest.
 What activities tend to aggravate the symptoms? Pulling and pushing activities typically worsen thoracic symptoms. Aggravation of localized pain by coughing, sneezing, or deep inspiration tends to implicate the costovertebral joint.82
What activities tend to aggravate the symptoms? Pulling and pushing activities typically worsen thoracic symptoms. Aggravation of localized pain by coughing, sneezing, or deep inspiration tends to implicate the costovertebral joint.82
 Is the pain deep, superficial, aching, burning, or stabbing? The patient is asked to describe the quality of the pain. Thoracic nerve root pain is often sharp, stabbing, and severe, although it can also have a burning quality. Nerve pain usually is referred in a sloping band along an intercostal space.20 Vascular pain and visceral pain often are described as being poorly localized and achy. A sudden onset of pain related to trauma could indicate a fracture, muscle strain, or ligament sprain.
Is the pain deep, superficial, aching, burning, or stabbing? The patient is asked to describe the quality of the pain. Thoracic nerve root pain is often sharp, stabbing, and severe, although it can also have a burning quality. Nerve pain usually is referred in a sloping band along an intercostal space.20 Vascular pain and visceral pain often are described as being poorly localized and achy. A sudden onset of pain related to trauma could indicate a fracture, muscle strain, or ligament sprain.
