Neurodynamics is the study of the mechanics and physiology of the nervous system. The nervous system is an electrical, chemical, and mechanical structure with continuity between its two subdivisions: the central and peripheral nervous systems (see Chapter 3). In addition to permitting inter- and intraneural communication throughout the entire network, the nervous system is capable of withstanding mechanical stress as a result of its unique mechanical characteristics. Nervous tissue, a form of connective tissue, is viscoelastic. This viscoelasticity allows for the transfer of mechanical stress throughout the nervous system during trunk or limb movements. This adaptation results from changes in the length of the spinal cord during movement and the capacity of the peripheral nerves to adapt to different positions. The peripheral nerves adapt through a process of passive movement relative to the surrounding tissue via a gliding apparatus around the nerve trunk.1,2 Three mechanisms appear to play an important role in this adaptability:2 The efficiency of this mechanism partially depends on the capacity of the loose connective tissue around the nerve (adventitia, conjunctiva nervorum, perineurium) to allow any traction forces to be distributed over the whole length of the nerve. If this distribution of forces is compromised, an unfavorable rise in traction forces can occur at certain segments, depending on the anatomic site (see next section).3 The role that tension on the neural tissue plays in pain and dysfunction has been studied for over a century. During this time, a number of specific tests have been designed to examine the neurological structures for the presence of adaptive shortening and inflammation.3–6 The more common of these neurodynamic mobility tests are described in this chapter. Once detected, any lack of neural mobility that appears to be contributing to a patient’s signs and/or symptoms can be addressed using a number of neural mobilization techniques. Neurodynamic mobilizations, which use specific combinations of active or passive movements that aim to reduce mechanosensitivity and restore symptom-free function, have been advocated for certain nerve-related dysfunctions.7,8 Until recently, the proposed effects of neural mobilization were based on theory rather than research evidence.9–11 Most of the studies have examined the influence of neural mobilization exercises on nerve mechanics in cadavers and subsequently in vivo.12 The spinal dura (see Chapter 3) forms a loose sheath around the spinal cord from the foramen magnum to the level of the second sacral tubercle. From there it continues as the filum terminale to the end at the coccyx. Laterally, the dura surrounds the exiting spinal nerve roots at the level of the intervertebral foramen. There are three areas called tension sites, in which the dura is tethered to the bony canal, providing stability to the spinal cord. These tension sites are found at the segmental levels of C6, T6, and L4; the elbow; the shoulder; and the knee have similar sites.3,4,13 As a result of these sites of tension, the neurologic tissues move in different directions, depending on where the stress is applied, and in which order it is applied.3 It has been suggested that the nervous system is loaded differently depending on the sequence of joint movement. This suggestion has been questioned in a study by Boyd et al.14 which found that varying the movement sequence did not substantially impact excursion and strain in the end position of one of the most common neurodynamic tests—the straight-leg raise (SLR). Theoretically, during movement, neural tissue takes its lead from the movement of joints and muscles, with the physical loading of the nerve dependent on the location of the nerve in relation to the joint axis.3 Various studies have demonstrated excursion of the nerve complex during movements of the extremity.12,15–18 Under normal circumstances, the tension sites are not adversely affected by the motion of the extremities. Despite their apparent mobility, nerves, and their microcirculation are vulnerable to tension, friction, and compressive forces at multiple sites along their routes.19 If the dura becomes adherent, excessive stress may be produced in the areas of adhesion, increasing the length of the dura beyond its normal limit of tension (Table 11-1).3 Theoretically, increased dural tension may be felt throughout the neuromeningeal system and, potentially, it may affect the range of motion available to the trunk and to an extremity. Pathomechanically, a decrease in the mobility of a nerve along its entire length may make the nerve more vulnerable to additional injuries during repetitive movements.3,19,20 One study12 examined the difference in median nerve excursion between different types of nerve gliding exercises (including sliders and tensioners). Sliders utilize combinations of joint movements to encourage peripheral nerve excursion by increasing elongation at one end of the nerve bed, thereby creating tension on the nerve from that end, while simultaneously releasing tension from the other end of the nerve.11 In contrast, tensioners utilize combinations of joint movements that elongate the nerve bed from both ends in an attempt to stretch the normal connective tissues. Of the two, it was determined that sliders produce greater amounts of nerve excursion compared to tensioners.12 TABLE 11-1 Sites of Peripheral Nerve and Nerve Root Vulnerability Site Description Tunnels Hard-sided tunnels, such as the carpal tunnel, increase the probability of spatial compromise of the nerve. Within a tunnel, the contained nervous system always has the potential to rub on the tunnel structure, creating friction, and any trauma or alteration to the tunnel structure can mechanically or chemically compromise the neural structures Branches It is more difficult for the nerve to move away from forces at those points where a nerve branches (e.g., radial nerve at the elbow) Hard interfaces A nerve is more readily compressed if it lies on a bone or passes through fascia (e.g., radial nerve in the spiral groove of the humerus) Proximity to the surface Superficial nerves, such as the sensory radial nerve in the forearm, are more vulnerable to external compression Adherence to interfacing structures Some areas of nerve are more firmly adherent to interfacing tissues than others (e.g., the common fibular (peroneal) nerve at the head of the fibula) Data from Butler DS, Tomberlin JP. Peripheral nerve: structure, function, and physiology. In: Magee D, Zachazewski JE, Quillen WS, eds. Scientific Foundations and Principles of Practice in Musculoskeletal Rehabilitation. St. Louis, MO: WB Saunders, 2007:175–189.
CHAPTER 11
Neurodynamic Mobility and Mobilizations
OVERVIEW
 Elongation of the nerve against elastic forces. In normal daily movement, nerves may slide up to 2 cm in relation to surrounding tissues and contend with a strain of 10%.3
Elongation of the nerve against elastic forces. In normal daily movement, nerves may slide up to 2 cm in relation to surrounding tissues and contend with a strain of 10%.3
 Longitudinal movement of the nerve trunk.
Longitudinal movement of the nerve trunk.
 An increase and decrease of tissue relaxation at the level of the nerve trunk.
An increase and decrease of tissue relaxation at the level of the nerve trunk.
PROPOSED MECHANISMS FOR NEURODYNAMIC DYSFUNCTION
A number of mechanisms (excluding diseases such as diabetes mellitus, hypothyroidism, immune deficiency syndromes, rheumatoid arthritis, and alcoholism) are hypothesized to contribute to an injury of the peripheral nerve trunk. These include the following:23
 Posture. Sustained postures that produce changes in the natural curves of the spine can result in a shortening of the distance traveled by the peripheral nerve trunk and eventual adaptive shortening of these structures. Correction of this posture, after sufficient time has elapsed for it to have taken place, may produce a stretching of the neural tissues.
Posture. Sustained postures that produce changes in the natural curves of the spine can result in a shortening of the distance traveled by the peripheral nerve trunk and eventual adaptive shortening of these structures. Correction of this posture, after sufficient time has elapsed for it to have taken place, may produce a stretching of the neural tissues.
 Direct trauma. Orthopaedic injuries account for some of the injuries to peripheral nerves. For example, the radial nerve is injured through orthopaedic trauma more than any other major nerve.24 Nerve injuries can occur as the result of a direct blow to the nerve or secondary to damage of an adjacent structure such as a fracture,25,26 joint dislocation,27 or tendon rupture.28 Other causes of direct nerve trauma have included injections,29 joint manipulations,30 and surgical procedures.31 A neurological injury is one of the most serious complications of fracture and dislocation, both in the short and long term. For example, the prevalence of injury to the sciatic nerve after acetabular fracture or fracture–dislocation of the hip has been reported to be between 10% and 25%.32
Direct trauma. Orthopaedic injuries account for some of the injuries to peripheral nerves. For example, the radial nerve is injured through orthopaedic trauma more than any other major nerve.24 Nerve injuries can occur as the result of a direct blow to the nerve or secondary to damage of an adjacent structure such as a fracture,25,26 joint dislocation,27 or tendon rupture.28 Other causes of direct nerve trauma have included injections,29 joint manipulations,30 and surgical procedures.31 A neurological injury is one of the most serious complications of fracture and dislocation, both in the short and long term. For example, the prevalence of injury to the sciatic nerve after acetabular fracture or fracture–dislocation of the hip has been reported to be between 10% and 25%.32
 Extremes of motion. Given the course of many of the peripheral nerve trunks, it is not difficult to envision movements of the extremities that could place a traction force on these trunks. Indeed, those very same movements are exploited in some of the neurodynamic mobility tests.
Extremes of motion. Given the course of many of the peripheral nerve trunks, it is not difficult to envision movements of the extremities that could place a traction force on these trunks. Indeed, those very same movements are exploited in some of the neurodynamic mobility tests.
 Electrical injury. In a 17-year review of burn unit admissions, permanent nerve injuries were found in 22% of electrocuted patients.33 The upper limb was most commonly involved with the median and ulnar nerves most commonly injured.33 Postneurologic symptoms in such cases can vary from neuropathy to complex regional pain syndrome (CRPS).
Electrical injury. In a 17-year review of burn unit admissions, permanent nerve injuries were found in 22% of electrocuted patients.33 The upper limb was most commonly involved with the median and ulnar nerves most commonly injured.33 Postneurologic symptoms in such cases can vary from neuropathy to complex regional pain syndrome (CRPS).
 Compression. Compression to a nerve can occur during muscle contraction and as a result of tight fascia, osteochondroma, ganglia, lipomas and other benign neoplasms, and bony protuberances.
Compression. Compression to a nerve can occur during muscle contraction and as a result of tight fascia, osteochondroma, ganglia, lipomas and other benign neoplasms, and bony protuberances.
The underlying mechanisms associated with clinical improvements following neural mobilization remain unclear.9
Double-Crush Injuries
The double-crush syndrome (DCS) is a general term referring to the coexistence of dual neuropathies along the course of a peripheral nerve. The concept was proposed by Upton and McComas in 197334 who suggested that proximal compression of a nerve may decrease the ability of the nerve to withstand a more distal compression.35
From the pathophysiological viewpoint, impairment of neural excursion, loss of elasticity, underlying abnormality of the connective tissue as well as direct pressure on the nerve may lead to disruption of axons, impairment of axonal transport, endoneural edema, or ischemic changes in nerves.35 For example, according to this theory, a cervical radiculopathy, manifesting as little more than neck pain and stiffness, could precipitate a distal focal entrapment neuropathy.34 The term double-crush syndrome is used to describe this mechanism of nerve injury: the serial compromise of axonal transport along the same nerve fiber causing a subclinical lesion at the distal site to become symptomatic.
At least eight etiologic mechanisms have been proposed to explain the relationship between the proximal and distal nerve fiber lesions:34,36–39
- A proximal nerve lesion renders the distal nerve segment more vulnerable to compression because of serial constraints of axoplasmic flow.
- The peripheral nerves possess an underlying susceptibility to pressure.
- Interruption of lymphatic and venous drainage at the proximal nerve lesion site renders the distal nerve segment more vulnerable.
- Endoneurial edema at one lesion site compromises neural circulation, rendering nerve fibers at the other site more vulnerable.
- A connective tissue abnormality common to both sites along the nerve fibers.
- Tethering of the nerve at one site causes injurious shear forces at the other site.
- Entrapment of the nerve at one site can cause a decrease in the function of the muscle pump, which creates a slight, generalized edema of the limb. This increases tissue pressure in certain anatomic passages, which causes an additional entrapment nerve lesion.
- The initial nerve lesion discharges a metabolite that travels through the intraneural circulation, increasing the vulnerability of other segments of the nerve.
Since its introduction, the double-crush hypothesis has been invoked to explain a great number of coexisting proximal and distal nerve impairments. In fact, it has been expanded in various ways (i.e., to triple-crush, quadruple-crush, and multiple-crush syndromes, as well as the reversed DCS).37,40,41 Despite its acceptance, there are some clinical situations where the double-crush hypothesis has anatomic and pathophysiologic restrictions that render it inapplicable.42 For the DCS to occur, there must be anatomic continuity of nerve fibers between the two (or more) lesions sites. If this is lacking, then a sequential impairment of axoplasmic flow obviously cannot occur. Consequently, two focal nerve disorders along the same neural pathway (e.g., cervical root lesions and carpal tunnel syndrome) do not automatically fulfil this anatomic criterion of DCS unless the same axons are compromised at both sites.42
Although, experimental studies of the double-crush hypothesis have shown that successive lesions along a peripheral nerve can summate,38,43,44 studies that have attempted to demonstrate the existence of DCS have as yet proved inconclusive.45–47
A neurophysiological examination is critical in distinguishing between a single or a double lesion as well as determining the comparative severity of the two lesions.35
NEURODYNAMIC MOBILITY EXAMINATIONS
Both Elvey48 and Butler20 have been credited with the initial development of the examination techniques for neurodynamic mobility. Elvey48 developed what he named the brachioplexus tension test, which was later called the upper limb tension test (ULTT). Similar tests, such as the SLR and prone knee flexion tests, have since been designed for the lower extremity. The slump test, popularized by Maitland,49, is considered to be a general test of neurodynamic mobility. The tension tests are designed to apply a controlled sequential and progressive mechanical and compressive stress to the dura and other neurologic tissues, both centrally and peripherally, thereby assessing the contribution of the spinal nerve roots and peripheral nerves to extremity pain. The tests place tensile stresses on the dura of spinal nerve roots and peripheral nerves using a longitudinal traction force of the nerve until the patient’s symptoms are reproduced.3
The examination of neural adhesions is by no means an exact science, but the principles are based on sound anatomic theory. Knowledge of the course of each of the peripheral nerves is thus essential in order to put a sequential and adequate tension through each of them (see Chapter 3).
Breig’s tissue-borrowing phenomenon offers a plausible explanation for the neurodynamic tests.50 Breig observed that tension produced in a lumbosacral nerve root resulted in the displacement of the neighboring dura, nerve roots, and lumbosacral plexus toward the site of tension. In effect, a borrowing of the resting slack in neighboring meningeal tissues occurs as neural structures are pulled toward the site of increased tension.51 This displacement of the nerve roots plexi results in a decrease in the available slack and potential mobility of the neural tissues throughout the region.51
Positive symptoms for the presence of neuropathic dysfunction include pain, paresthesia, and spasm.23 Unfortunately, these signs and symptoms are also associated with a host of musculoskeletal injuries. Asbury and Fields52 hypothesized that the type of pain that results from an injury to a peripheral nerve is characteristic and has two varieties:
- Dysesthetic pain. This type of pain is felt in the peripheral sensory distribution of a sensory or mixed nerve and results from nociceptive afferent fibers.
- Nerve trunk pain. This type of pain results from the nociceptors within the nerve sheaths and exhibits a pain distribution following the course of the nerve trunk.
However, relying on the reproduction of a type of pain (a subjective issue at the best of times) is not sufficient to make the diagnosis of neural tissue dysfunction.
Because the subject of neural provocation tests and the intervention of neurodynamic mobilization remain controversial, the clinician should ensure that the results of these tests are always used in conjunction with findings from a complete neuromusculoskeletal examination, including the following:3,23,53–55
 Observation. An injury to a peripheral nerve trunk may result in visible atrophy within its motor distribution.
Observation. An injury to a peripheral nerve trunk may result in visible atrophy within its motor distribution.
 Palpation. The clinician should carefully palpate along each of the nerve trunks in the region where they are superficial. Physical deformation of an irritated nerve should reproduce pain with palpation.
Palpation. The clinician should carefully palpate along each of the nerve trunks in the region where they are superficial. Physical deformation of an irritated nerve should reproduce pain with palpation.
 The range of motion. In areas of decreased neural mobility, both active and passive range of motion may be diminished in the same direction. However, a lesion to the musculotendinous unit would also reproduce pain with the same maneuver, particularly in muscles that cross two joints.
The range of motion. In areas of decreased neural mobility, both active and passive range of motion may be diminished in the same direction. However, a lesion to the musculotendinous unit would also reproduce pain with the same maneuver, particularly in muscles that cross two joints.
 Resistive testing. Resistive tests can be used to examine for the presence of weakness in the distribution of a peripheral nerve and to help differentiate between pain reproduced with active or passive range of motion that indicates damage to the musculotendinous unit, and pain that results from neural tension. For example, pain reproduced in the posterior thigh with the SLR may indicate a lesion of the hamstring muscle belly or a lesion to the sciatic nerve. If resisted knee flexion does not reproduce pain, the musculotendinous unit is unlikely to be at fault, leaving the sciatic nerve as the likely cause.
Resistive testing. Resistive tests can be used to examine for the presence of weakness in the distribution of a peripheral nerve and to help differentiate between pain reproduced with active or passive range of motion that indicates damage to the musculotendinous unit, and pain that results from neural tension. For example, pain reproduced in the posterior thigh with the SLR may indicate a lesion of the hamstring muscle belly or a lesion to the sciatic nerve. If resisted knee flexion does not reproduce pain, the musculotendinous unit is unlikely to be at fault, leaving the sciatic nerve as the likely cause.
The purpose of the physical examination is to determine which tissue is at fault. This is accomplished by isolating (where possible) each tissue that has the potential to produce those symptoms and selectively stressing that tissue. Part of the problem with this approach lies in the fact that a positive finding for many of the assessment techniques may just produce a sensitive movement, rather than a stretch of the dura.3 For example, when wrist extension is performed with the elbow in extension and the shoulder abducted, in addition to placing stress on the elbow and wrist joints, wrist flexors, and elbow flexors, the loading of the nervous system is continued proximally, at least up to the level of the axilla.56
Some of the so-called dural symptoms could also result from the imparted stretch on the dura during the various maneuvers, producing changes in the axoplasmic flow inside the nerves, provoking the firing of abnormal impulses, and decreasing the vascular supply to the nerve.57–59
SLUMP TEST
A neural tension test performed in a sitting position is necessary to simulate the extremes of spinal motion associated with symptom-provoking activities such as slouched sitting or entering and exiting a car.49,60,61
The slump test, introduced by Maitland,49 is a combination of other neuromeningeal tests, namely, the seated SLR, neck flexion, and lumbar slumping. In the slump test, the patient is seated in full flexion of the thoracic and lumbar regions of the spine.62 Sensitizing maneuvers are then systematically applied and released to the cervical spine and lower extremities while the clinician maintains the patient’s trunk position.51 The slump test assesses the excursion of neural tissues within the vertebral canal and intervertebral foramen61 and detects impairments to neural tissue mobility from a number of sources as identified by Macnab63 and Fahrni.64 Maitland asserted that the slump test enables the tester to detect adverse nerve root tension caused by spinal stenosis, extraforaminal lateral disk herniation, disk sequestration, nerve root adhesions, and vertebral impingement.60,61
Over the years, several studies50,65–67 have demonstrated the effects of the trunk and head position on neural structures within the vertebral canal and intervertebral foramen during slump testing. These studies reported that full spinal flexion or flexion of the cervical, thoracic, and lumbar regions of the spine results in a lengthening of the vertebral canal and transmits tension to the spinal cord, lumbosacral nerve root sleeves, and nerve roots.50,65–68 A more recent study by Davis et al.69 found the slump test had a high false-positive rate in asymptomatic individuals and recommended that the current criteria for determining a positive test should be examined using new range-of-motion cutoff scores. The study also recommended that the test should be considered positive only when peripheral symptoms are reproduced before 22 degrees of knee extension.69 A 2011 pilot study by Trainor and Pinnington70 indicated good inter-tester reliability and suggested that the slump knee bend test has the potential to be a useful clinical test for identifying patients with mid lumbar nerve root compression.
Depending on which text is read, there is a wide variety of progressive steps to the slump test, particularly when the lumbar kyphosis stage is introduced. Although the specific order of implementation remains controversial, it is important that the clinician consistently use the same sequence with each patient. For example, when the extension of the cervical spine is introduced, the dura and the nerve roots slacken. Extending the thoracic and lumbar spines increases the slack in the neural tissues.
Because the slump test is a combination of other tests, a choice as to its use needs to be made. Either the classic SLR test or its variations should be performed, or the slump test should be used.72

FIGURE 11-1 The femoral slump test.
As soon as symptoms are reproduced during these tests, the test should be terminated. It is worth remembering that during a dural tension test, the dura itself does not move. It is merely stressed; hence, the name for the tests. One such method of sequencing for the slump test is described next.
The patient is positioned sitting with the hands behind the back, the popliteal creases just off the edge of the bed and a slight arch in the back (Fig. 11-2), and the head flexed and then placed in neutral. This initial position is then followed by a slump of the lumbar and thoracic spine with a posterior pelvic tilt as the clinician maintains the patient’s neck in neutral (Fig. 11-3). This maneuver has the effect of tightening the entire dura including the thoracic dura. If the test is still negative, the patient is asked to flex the neck by first applying a chin tuck and placing the chin on the chest and then to straighten the knee as much as possible. Overpressure is then gently applied to the upper thoracic and the lower cervical spine and maintained throughout the examination (Fig. 11-4). The subject’s ankle is then passively dorsiflexed to the point of slight resistance, while the knee is slowly passively extended to full extension or to the point when the subject reports an onset of neural mediated symptoms (Fig. 11-5). If the patient is unable to straighten the knee because of a reproduction of symptoms, he or she is asked to actively extend the neck. Following the extension of the neck, if the patient cannot straighten the knee further, the test can be considered positive.
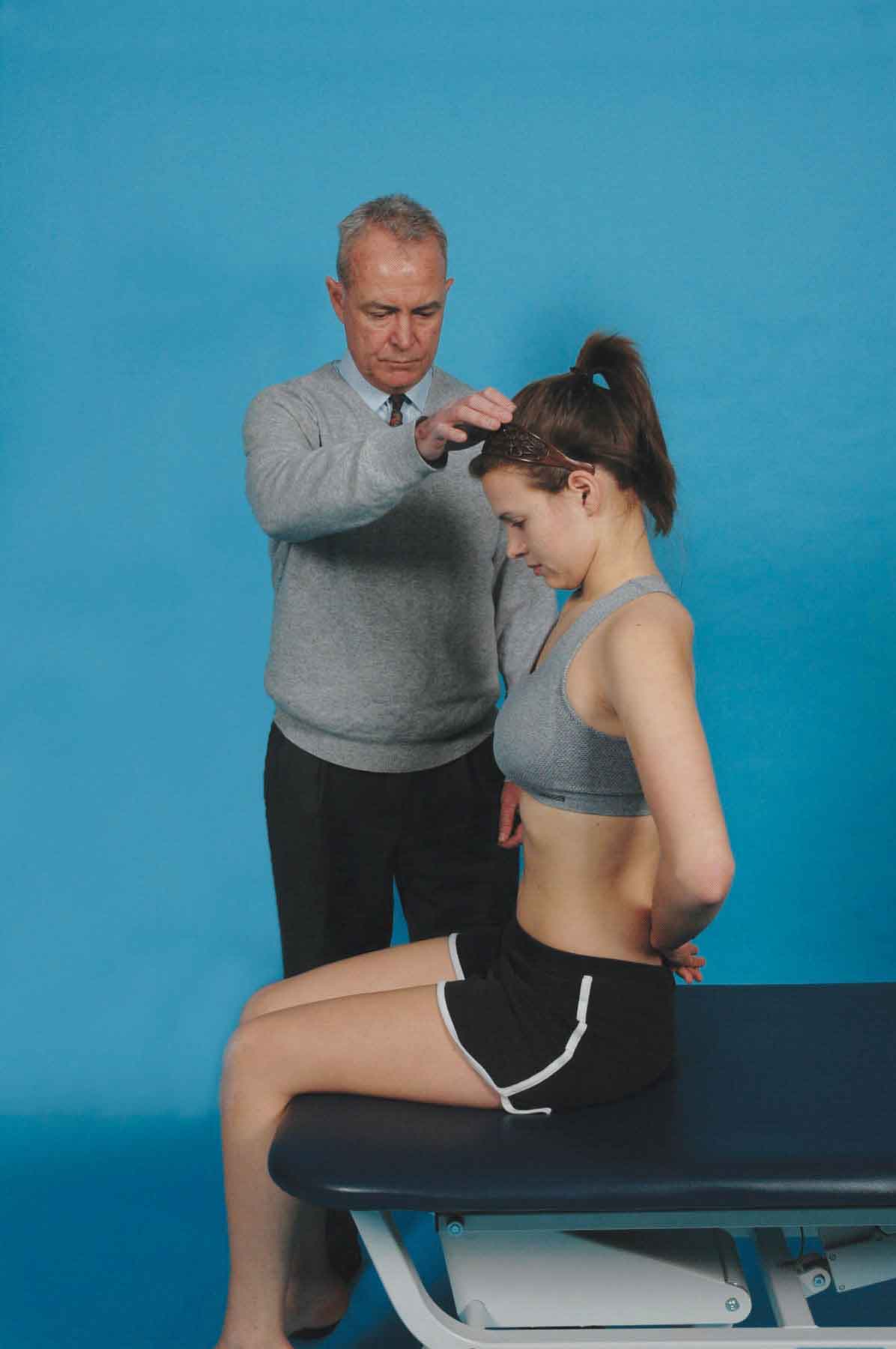
FIGURE 11-2 The slump test 1.
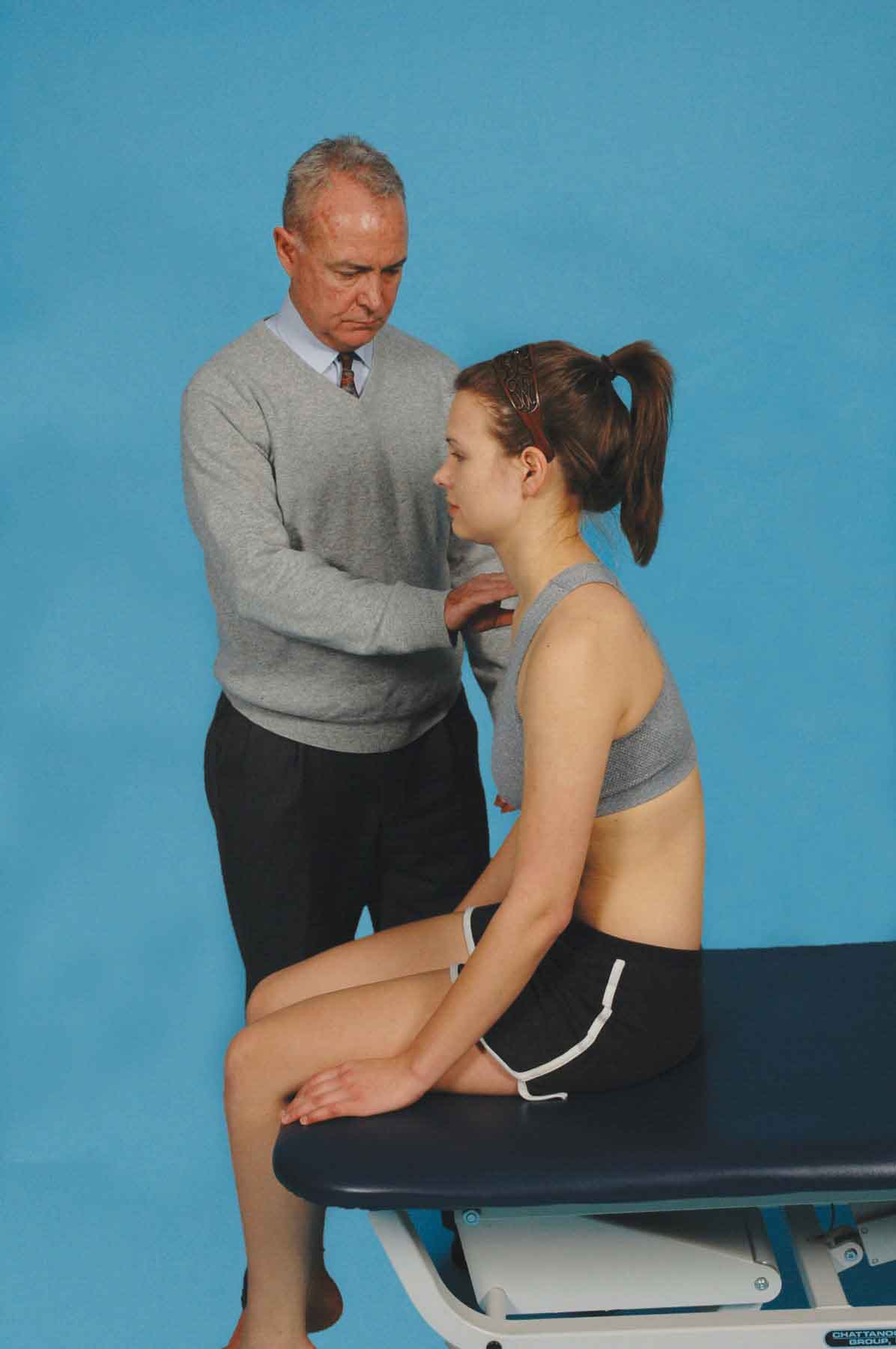
FIGURE 11-3 The slump test 2.

FIGURE 11-4 The slump test 3.

FIGURE 11-5 The slump test 4.
The test can also be performed in reverse because a positive response may occur in one direction but not the other.
LOWER EXTREMITY TENSION TESTS
Sciatica is defined as pain along the course of the sciatic nerve or its branches and is most commonly caused by a herniated disk or by lateral recess spinal stenosis.73 Characteristically, patients with sciatica report gluteal pain radiating down the posterior thigh and leg, paresthesia in the calf or foot, and varying degrees of motor weakness. Extraspinal entrapment of the sciatic nerve (i.e., along its course within the pelvis or the lower extremity), although infrequent, is difficult to diagnose because its symptoms are similar to those of the more frequent causes of sciatica.
Straight-Leg Raise
The SLR test is recognized as the first neural tissue tension test to appear in the literature. It was first described by Lasègue well over 100 years ago.74
