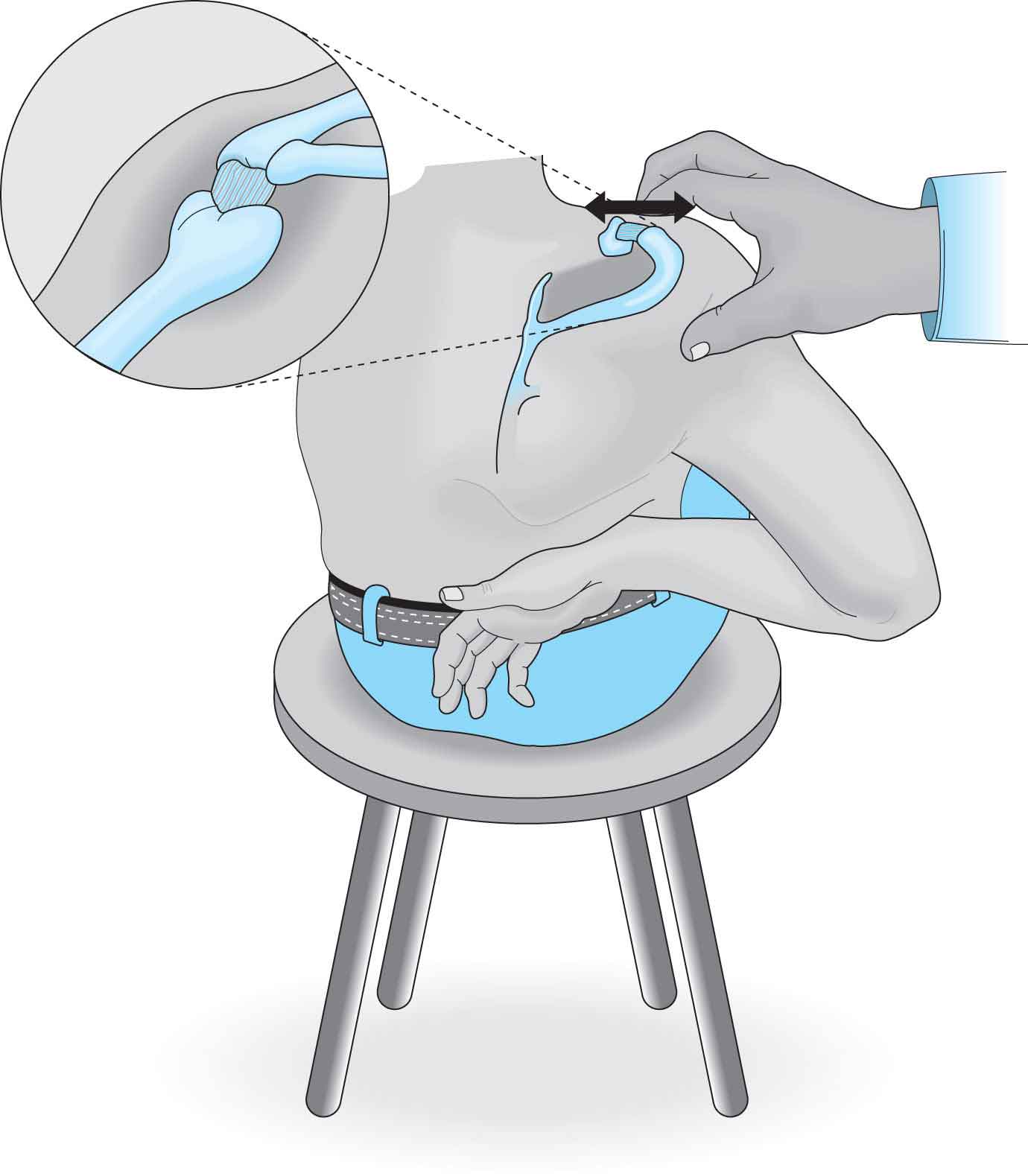
Touch has always been and continues to be a primary healing modality. The first written records of massage go back to Ancient China, and wall paintings in Egypt depict hands-on healing techniques that go back 15,000 years.1 From this early “laying on of hands” evolved many of the techniques used today. The techniques of MT fall under the umbrella of therapeutic touch. MT has become such an important component of the intervention for orthopaedic and neurologic disorders that it is considered by many as an area of specialization within physical therapy. Of the approaches commonly applied, the Cyriax,2 Mennell,3 and osteopathic techniques4,5 (Table 10-1) originated from physicians, whereas the Maitland,6,7 Kaltenborn,8 and McKenzie and May9 approaches (Table 10-2) were derived by physical therapists.10–12 TABLE 10-1 Manual Therapy Approach—Physician Generated Cyriax (Orthopaedic Medicine) Assertions Mennell Assertions Osteopathic Assertions Philosophy All pain has an anatomic source and, therefore, all treatment must reach that anatomic source If the diagnosis is correct, the treatment will be of benefit to the source Dysfunction indicates a serious pathologic process or joint disease Loss of normal joint movement or joint play can lead to dysfunction Joint manipulation can restore normal joint-play movements Neuromusculoskeletal system is connected with other systems; therefore, disease processes can be evident in musculoskeletal system An abnormality in structure (somatic dysfunction) can lead to abnormal function of related components Manipulative therapy can restore and maintain normal structure and function relationships Key concepts Diagnosis of soft-tissue lesions Categorization of referred pain Differentiation between contractile and noncontractile lesions Assessment of joint play Diagnosis of somatic dysfunction Examination focuses on presence of asymmetry, restriction of movement, and palpation of soft-tissue texture changes (i.e., palpation of skin, muscle, and other connective tissue for feeling of thickness, swelling, tightness, or temperature change) History Observation and history Age and occupation Symptoms (site and spread, onset and duration, and behavior) Medical considerations Inspection Present complaint Onset Nature of pain Localization of pain Loss of movement Past history Family history Medical systems review History Knowledge of physical trauma, past history of visceral, and soft-tissue problems Present complaint Establish relationship from patient’s history between time and mechanism to adaptation, and decompensation Physical examination Active movements Passive movements Resisted movements Neurologic examination Palpation Inspection Inspection Palpation Examination of voluntary movements Muscle examination Special tests (e.g., roentgenography) Examination of joint-play movements Postural analysis Regional screening functional units Pelvic girdle Foot Vertebral column Shoulder girdle Hand Interpretation of evaluation Identification of anatomic structure associated with lesion Joint dysfunction Determination of dysfunction: – Positional fault – Restriction fault Segmental or multisegmental Treatment strategies Injection Friction massage Manipulation Mobilization Physical therapy (e.g., exercise and modalities) Patient education Manipulation Mobilization Physical therapy (e. g., exercise and modalities) Patient education Manipulation Mobilization Muscle energy Myofascial techniques Counterstrain Exercise therapy Patient education Data from Di Fabio RP. Efficacy of manual therapy. Phys Ther. 1992;72:853–864. TABLE 10-2 Manual Therapy Approach—Physical Therapist Generated Maitland (Australian) Assertions Kaltenborn (Norwegian) Assertions McKenzie Assertions Philosophy Personal commitment to understand patient Consideration and application of theoretical (e.g., pathology and anatomy) and clinical thinking (e.g., signs and symptoms) Continual assessment and reassessment of data Biomechanical assessment of joint movements Pain, joint dysfunction, and soft-tissue changes are found in combination Predisposing factors of sitting posture, loss of extension range, and frequency of flexion contribute to spinal pain Patients should be involved in self-treatment Key concepts Examination, technique, and assessment are interrelated and interdependent Grades of movement (I–V) Strong emphasis on use of passive movement testing (testing accessory and physiologic joint movements) Differential assessment to prove or disprove clinical working hypothesis Application of principles from arthrokinematics (e.g., concave–convex rule and close- and open-packed positions) to determine existence of somatic dysfunction Grades of movement (I–III) During movements of spine, positional change to nucleus pulposus takes place Strong emphasis on use of active motions Flexed lifestyle leads to a more posterior position of nucleus Intervertebral disk is common source of back pain Evaluation framework Subjective examination (as defined by Maitland)14,15 Establish kind of disorder Area of symptoms Behavior of symptoms Irritability Nature Special questions Planning objective examination (as defined by Maitland)14,15 Physical examination Observation Functional tests Active movements Isometric tests Other structures in plan Passive movements (e.g., special tests, physiologic and accessory joint movements, and relevant adverse neural tissue tension tests) Palpation Neurologic examination Highlight main findings History (“five-by-five scheme”) Immediate case history (e.g., assess symptoms for localization, time, character, etc.) Previous history (e.g., assess for kind of treatment, relief of symptoms, presence of similar symptoms or related symptoms) Social background Medical history Family history Patient’s assessment of cause of complaint Physical examination Inspection Function (active and passive movements; testing with traction, compression, and gliding; and resisted tests) Palpation Neurologic tests Additional tests History Interrogation (e.g., where did pain begin, how, constant or intermittent, what makes it better or worse, previous episodes, and further questions) Posture (sitting and standing) Examination of movement (flexion, extension, and side gliding) Movements in relation to pain Repeated movements Test movements Other tests (e.g., neurologic and other joints) Evaluation Initial assessment relates examination findings Behavior of patient’s symptoms—pain or stiffness (somewhat analogous to McKenzie’s derangement and dysfunction syndrome, respectively) Diagnosis, although no specific structure designated Stage of disorder Stability of disorder Irritability of disorder Biomechanical assessment (i.e., restriction of joint mobility) and assessment of soft-tissue changes Diagnosis according to syndrome, as opposed to specific structure Postural syndrome (end range strain on normal tissues) Dysfunction syndrome (adaptive shortening of structure) Derangement syndrome (disturbance of normal anatomic relationship) Intervention strategies Based on continual assessment of subjective and objective findings Focus on treating pain or stiffness Mobilization Manipulation Adverse neural tissue mobilization Traction Exercise using movements that have positive influence on symptoms Patient education Mobilization Exercise (emphasis on proprioceptive neuromuscular facilitation) Traction/distraction Soft-tissue mobilization Manipulation Patient education Patient self-treatment using repeated active movements Exercise using movements that have positive influence on symptoms Mobilization or manipulation (if needed) Strong emphasis on patient education and self-treatment Data from Di Fabio RP. Efficacy of manual therapy. Phys Ther. 1992;72:853–864. Within these major philosophies, a number of subsets have also emerged, including myofascial release (MFR), positional release techniques, neurodynamic mobilization techniques (see Chapter 11), manually resisted exercise, proprioceptive neuromuscular facilitation (PNF), joint mobilization, and high-velocity thrust (manipulation) techniques. MT techniques have traditionally been used to produce a number of therapeutic alterations in pain and soft-tissue extensibility through the application of specific external forces to decrease pain and improve motion quality in an area with restriction.13 Some of these therapeutic alterations may be neurophysiologic and are therefore difficult to clinically assess. Unfortunately, the therapeutic efficacy of many MT techniques remains undetermined. Thus, many of these techniques have not been developed with the same scientific rigor as fields such as anatomy and physiology, and much of their use is based on clinical outcomes, rather than evidence-based proof. There are numerous concerns with determining the validity of studies addressing the efficacy of manual techniques: Although it is generally agreed that manual techniques are beneficial for specific impairments, such as a restricted joint glide and adaptively shortened connective tissue, there is less agreement on which technique is the most effective. The decision about which approach or technique to use has traditionally been based on the clinician’s belief, training, the level of expertise, and decision-making processes. This has led to widespread opinions on which tools to use to measure outcome; how to apply a particular technique in terms of patient setup, intensity, and duration; and how to gauge an individual’s response to a technique. Indeed, research studies seem to agree that the most efficacious approach is a combination of manual techniques with other interventions, such as progressive exercises, the use of therapeutic modalities, and patient education about proper body mechanics, positions, and postures.15–17 Regardless of which MT technique is used, all patients should undergo a full examination/evaluation before any technique is performed. Despite the varied approaches and rationales, there is general agreement concerning the criteria for the correct application of a manual technique. These include:19 TABLE 10-3 Indications for Selection of Manual Technique Based on Duration of Symptoms Acute Subacute Chronic Muscle energy Strongly indicated Strongly indicated Used to prepare tissue for joint manipulation and prevent recurrence of dysfunction Joint mobilization Grades I and II Grades II and III Grades III and IV Joint manipulation Rarely indicated Moderate-to-strong indication if muscle energy technique unsuccessful Strong indication if muscle energy technique ineffective Data from Ellis JJ, Johnson GS. Myofascial considerations in somatic dysfunction of the thorax. In: Flynn TW, ed. The Thoracic Spine and Rib Cage: Musculoskeletal Evaluation and Treatment. Boston, MA: Butterworth-Heinemann; 1996:211–262. TABLE 10-4 Appropriate Technique Based on Barrier to Motion and End-Feel Barrier End-Feel Technique Pain Empty None Pain Spasm None Pain Capsular Oscillations Joint adhesions Early capsular Passive articular motion stretch Muscle adhesions Early elastic Passive physiologic motion stretch Hypertonicity Facilitation Hold–relax Bone Bony None Reassessment is an integral part of any intervention. The clinician must be able to gauge how effective a technique has been so that necessary modifications can be made. Measurement procedures used by the clinician to determine the effectiveness of manual intervention must adequately reflect changes in pain level, impairments, and functional ability. Although measurements of range of motion (ROM), pain, and strength are valid and reliable,30–32 the functional measurement selected should be related to the particular functional limitation that the clinician is expecting to change with the intervention.33 MT is indicated in the following cases: Contraindications to MT include those that are absolute contraindications and those that are relative.34,35 Soft-tissue techniques can address multiple structures simultaneously to include, but are not limited to muscles, tendons, ligaments, fascia, and/or venous lymphatic structures.13 Increasing the length of tissue, breaking up fibrous scar tissue, breaking up adhesions, remodeling of collagen fibers, increasing circulation, and improving venous function and/or lymphatic function, decreasing pain, can all be included as goals for soft-tissue mobilization.13 Transverse friction massage (TFM) is a technique devised by Cyriax, whereby repeated cross-grain massage is applied to a muscle, tendon, tendon sheath, or ligament. TFM has long been used by physical therapists to increase the mobility and extensibility of individual musculoskeletal tissues, and to help prevent and treat inflammatory scar tissue.2,36–41 TFM is contraindicated for acute inflammation, hematomas, debilitated or open skin, and peripheral nerves, and in patients who have diminished sensation in the area. TFM is purported to have the following therapeutic effects: The application of the correct amount of tension to a healing structure is very important. The tissue undergoing TFM should, whenever possible, be positioned in a moderate but not painful stretch. The exception to this rule is when applying TFM to a muscle belly, which is usually positioned in its relaxed position.2,43 Lubricant is not typically used with the application of TFM. However, ultrasound can be applied to a tissue before TFM. Beginning with light pressure, and using a reinforced finger (i.e., middle finger over the index finger), or thumb, the clinician moves the skin over the site of the identified lesion back and forth, in a direction perpendicular to the normal orientation of its fibers (Fig. 10-1). It is important that the patient’s skin move with the clinician’s finger to prevent blistering. FIGURE 10-1 Transverse friction to the supraspinatus tendon. The tendon is brought into a more sagittal position just below the anterior acromion by placing the patient’s hand behind the back. The forefinger of the clinician is reinforced by the middle finger while applying the massage perpendicular to the tendon fibers, in an anterior-posterior direction. The amplitude of the massage should be sufficient to cover all of the affected tissue, and the rate should be at two to three cycles per second, applied in a rhythmical manner. The duration of the friction massage is usually gauged by when desensitization occurs (normally within 3–5 minutes). Tissues that do not desensitize within 3–5 minutes should be treated using some other form of intervention. If the condition is chronic or in the remodeling stage of healing, then the frictions are continued for a further 5 minutes after the desensitization, in an effort to enhance the mechanical effect on the cross-links and adhesions. Following the application of TFM, the involved tissue is either passively stretched or actively exercised, taking care not to cause pain. Most conditions amenable to TFM should resolve in 6–10 sessions over 2–8 weeks. When possible, patients should be taught how to apply TFM on themselves so that treatments can be continued at home. Tissues that do not show signs of improvement after three treatment sessions should be treated using some other form of intervention. MFR is a series of techniques designed to release restrictions in the myofascial tissue and is used for the treatment of soft-tissue dysfunction. The development of a holistic and comprehensive approach to the evaluation and treatment of the myofascial system of the body is credited to John Barnes, who was strongly influenced by the teachings of Mennell44 and Upledger and Vredevoogd.45 According to myofascial theory, the collagen provides strength to the fascia, the elastin gives it its elastic properties, and the gel functions to absorb the compressive forces of movement. Three types of fascia are considered to exist (see Chapter 1):35,46 The theory of MFR is based on the principle that trauma or structural abnormalities may create inappropriate fascial strain, because of an inability of the deep fascia to absorb or distribute the forces.46 These strains to the deep fascia can result in a slow tightening of the fascia, causing the body to lose its physiologic adaptive capacity.46 Over time, the deep fascial restrictions begin to pull the body out of its three-dimensional alignment, causing biomechanically inefficient movement and posture.46 In addition, because of the association of the deep fascia at the cellular level, it is theorized that trauma to or malfunction of the fascia can lead to poor cellular efficiency, disease, and pain throughout the body.35,46 Three theoretical models for the manifestation of myofascial dysfunction are a contraction, contracture, and cohesion–congestion (Table 10-5). TABLE 10-5 Theoretical Models for the Manifestation of Myofascial Disorders Model Manifestation End-Feel Contraction Muscle hypertonicity or spasm Reactive, firm, and painful end-feel Contracture Inert or noncontractile tissues that have undergone fibrotic alteration Abrupt, firm, stiff, or hard end-feel Cohesion–congestion Fluidochemical changes in microcellular transport systems, resulting in impairment Boggy, stiff, or reactive end-feel lymphatic flow, vascular stasis, or ischemia Data from Ellis JJ, Johnson GS. Myofascial considerations in somatic dysfunction of the thorax. In: Flynn TW, ed. The Thoracic Spine and Rib Cage: Musculoskeletal Evaluation and Treatment. Boston, MA: Butterworth-Heinemann; 1996:211–262. Thus, the purpose of MFR techniques is to apply a gentle sustained pressure to the deep fascia, in order to release fascial restrictions, thereby restoring normal pain-free function.35 Clinicians use the elbow, knuckle, or fingertips creating localized hyperemia through deep friction. MFR relies entirely on the feedback received from the patient’s tissues, with the clinician interpreting and responding to the feedback. This feedback is based on the Upledger concept of the natural body rhythm, called the craniosacral rhythm.45 It is this rhythm that is theorized to guide the clinician as to the direction, force, and the duration of the technique. It is not unusual for a patient to experience muscle soreness following MFR techniques. This soreness is thought to result from postural and alignment changes or from the techniques themselves. The soft-tissue techniques used in MFR are purported to break up cross-restrictions of the collagen of the fascia. Three of the more commonly used techniques involve stroking maneuvers:35 It is important to remember that the claimed benefits and effectiveness of MFR techniques are largely anecdotal because at the time of writing there is no scientific experimental research to validate these claims. Soft-tissue mobilizations (STMs) are used in many of the manual techniques described within this chapter, including MFR, muscle energy (ME), and PNF. The techniques of STM are based on the concept that tissue restrictions occur at different layers, ranging from superficial to deep. The general principles behind STM are that the superficial layers are treated before deep layers, with the force used applied in the direction of the maximum restriction, and where the choice of technique is dependent on the extent of the restriction, amount of discomfort, and degree of irritability. Deep tissue massage is recommended to reduce spasm47 and promote pain reduction.48 Several well-recognized STM techniques are described next.49 This technique is applied to the center of the restricted tissue at the exact depth, direction, and angle of the maximal restriction. The sustained pressure technique can be modified by applying a force in either a clockwise or a counterclockwise direction while maintaining the sustained pressure. This spiral motion increases the tissue tension in one direction while easing it in the other. Sustained pressure can also be applied perpendicular or parallel to the restriction. Ischemic compression, a similar technique to sustained pressure, can be used on both active and inactive trigger points. It is believed that the ischemic compression deprives the trigger points of oxygen, rendering them inactive and breaking the cycle of pain–spasm–pain. Usually, the pressure is applied for 8–12 seconds. If the patient reports a lessening of local and referred pain, the clinician can repeat the treatment. However, if the pain does not lessen, the clinician may need to adjust the pressure or choose an alternative technique. Massage can be defined as the systematic, therapeutic, and functional stroking and kneading of the body.50 The French are credited with the introduction of massage, and many of the terms associated with massage still bear French names. Massage has long been a central part of the physical therapy curriculum. Studies have demonstrated that deep massage increases the circulation and skin temperature of the massaged area, as a result of dilation of the capillaries.51–54 A number of traditional massage techniques are used, including: Acupressure is based on the ancient arts of shiatsu and acupuncture, involving manual pressure over the acupuncture points of the body, to improve the flow of the body’s energy, known as Qi. This energy is thought to circulate throughout the body along a series of channels, called meridians. Traditional Eastern medicine is based on the concept that all disorders are reflected at specific points, either on the skin surface or just beneath it, along these channels. By careful manipulation of these points, the clinician can theoretically strengthen, disperse, or calm the Qi, enabling it to flow smoothly.57 Modern acupressurists use traditional meridian acupuncture points; nonmeridian or extrameridian acupuncture points, which are fixed points not necessarily associated with meridians; and trigger points, which have no fixed locations and are found by eliciting tenderness at the site of most pain.58 When acupressure is applied successfully, the patient is supposed to experience a sensation known as teh chi, defined as a subjective feeling of fullness, numbness, tingling, and warmth with some local soreness and a feeling of distention around the acupuncture point.58 Western scientific research has proposed a number of mechanisms for the effect of acupressure on relieving pain, as follows: The origin of ME techniques is credited to Fred Mitchell, Sr.68 ME techniques combine the precision of passive mobilization, with the effectiveness, safety, and specificity of reeducation therapies and therapeutic exercise.69 ME techniques, which involve positioning a restricted muscle–joint complex at its restricted barrier, can be used to mobilize joints, strengthen weakened muscles, and stretch adaptively shortened muscles and fascia. Optimal success with these techniques is more likely in the acute or subacute stages of healing before prolonged joint changes have had the opportunity to occur. According to the teachings of ME, muscles function as flexors, extensors, rotators, and side benders of joints, as well as being restrictors or barriers to movement. In other words, muscles both produce and control motion. Although it is obvious that muscles produce motion, it is easy to forget that they also resist motion. This resistance to motion is related to muscle tone, a complex neurophysiologic state governed by both cortical and spinal reflexes and by the afferent activity from the articular and muscle systems. Afferent input from types I and II mechanoreceptors located in the superficial and deep aspects of the joint capsule is projected to the motor neurons (see Chapter 3). Exaggerated spindle responses are provoked by any motions that attempt to lengthen the muscle, creating an increase in resistance to those motions. Stretching or lengthening of the muscle also stimulates the Golgi tendon organs, which have an inhibitory influence on muscle tension, leading to muscle relaxation. In addition, it has been demonstrated that cutaneous stimulation of certain areas of the body can produce inhibition or excitation of specific motor neuron pools.71 It is theorized that the neuromuscular system is “scarred” by pain and impairment, producing asymmetry in the musculoskeletal system and resulting in a disruption of the harmony and rhythm of the body, referred to as somatic dysfunction.69 Somatic dysfunctions can be described or named in one of three ways:25 In the presence of a somatic dysfunction, there is usually an asymmetric pattern of motion, with restriction in one direction and increased freedom in the opposite direction.25 The triad of ART (asymmetry, range of motion restriction or barrier, and tissue texture)27 helps to describe the characteristics of somatic dysfunction. Primary somatic dysfunctions, which may result from trauma, are reversible, as long as they are treated correctly and do not become chronic in terms of abnormal fibrosis or adhesions. Secondary somatic dysfunctions result from the consequences of visceral pathology, or from the adaptations made by somatic structures in response to forces or stresses imposed on them. The consequence of a somatic dysfunction can be a change in the length of the tissues that surround a joint. Some of these tissues adaptively shorten, whereas others adaptively lengthen. These changes in length are theorized to produce changes in the neurophysiologic makeup of the muscle, affecting tension development, as well as changes in the angle of pull. There is some commonality between ME and several procedures used in orthopaedic MT, such as PNF.72 Greenman27 summarizes the requirements for the correct application of ME techniques to be control, balance, and localization. The intent of ME is to treat somatic dysfunctions by restoring the muscles around a joint to their normal neurophysiologic state, through either stretching or strengthening the agonist and antagonist. Somatic dysfunctions include those in which the motion barrier is encountered before the physiologic barrier is reached.69 The type of motion barrier is determined by the end-feel (see Chapter 4). A normal end-feel would indicate normal range, whereas an abnormal end-feel would suggest abnormal range, either hypomobile or hypermobile, with the latter characterized by a loss of end-feel resiliency and an abrupt approach to the anatomic barrier. All ME techniques are classed as direct techniques because they engage the barrier.26 Indirect techniques form the basis for the strain–counterstrain (positional release) techniques,73 and the functional techniques,74–76 both of which are discussed later. The position of the clinician during the performance of the technique must allow easy access to the structures involved while maintaining proper body mechanics. In each of the recognized methods of ME, the setup is identical. The clinician positions the bone or joint so that the muscle group to be used is at its resting length. The patient is then given specific instructions about the direction in which to move, the intensity of the contraction, and the duration of the contraction.72,77–79 The amounts of force and counterforce are governed by the length and strength of the muscle group involved, as well as by the patient’s symptoms.77 The clinician’s force can match the effort of the patient, thus producing an isometric contraction and allowing no movement to occur, or it may overcome the patient’s effort, thus moving the area or joint in the direction opposite to that in which the patient is attempting to move it, thereby incorporating an eccentric or isolytic contraction.72 There appears to be no consensus as to whether to use the relaxation of the agonist or the antagonist to gain motion.27,70,80–82 Strain–counterstrain is a passive positional technique used in the treatment of musculoskeletal pain and related somatic dysfunction. According to strain–counterstrain theory, myofascial tender points (Fig. 10-2) are located and then monitored during which a position of comfort, or ease, is established to evoke a therapeutic effect.73,83,84 It is worth noting that to date no experimental studies have been published to confirm the existence of these tender points or the effectiveness of strain–counterstrain. FIGURE 10-2 Strain–counterstrain tender points of the body. AC, anterior cervical; PC, posterior cervical; LH, lateral hamstring; MH, medial hamstring; GX, gastrocnemius; LA, lateral ankle; LC, lateral calcaneal; NA, navicular; LT, lateral trochanter; SP, spinous process; TP, transverse process; PS, paraspinal; LE, lateral epicondyle; ME, medial epicondyle; LM, lateral meniscus; MM, medial meniscus; PAT, patella; TAL, talus; MA, medial ankle; DC, posterior (dorsal) cuboid; DM, posterior (dorsal) metatarsal; IS, interspinal; PSIS, posterior superior iliac spine; PLT, posterolateral trochanteric; PMT, posteromedial trochanteric. A possible neurophysiologic explanation of how and why these techniques work was first suggested by Korr,85 who postulated that an injured joint and its related tissues behaved differently from those of an uninjured joint in that the γ motor neuron activity in the former became increased. Bailey86 later refined the theory by suggesting that an inappropriate high “gainset” of the muscle spindle (see Chapter 3) resulted in changes characteristic of somatic dysfunction.87 Thus, the techniques of strain–counterstrain appear to serve to effect the muscle spindle–γ loop, by allowing the extrafusal muscle fibers to lengthen to their normal relaxed state, thereby decreasing spindle output and interrupting the pain–spasm cycle.87–89 Strain–counterstrain is also thought to improve blood flow to the area through a circulatory flushing of previously ischemic tissues.88,90
CHAPTER 10
Manual Techniques
OVERVIEW
 The selection of a particular technique is typically made on an ad hoc basis.
The selection of a particular technique is typically made on an ad hoc basis.
 The strong placebo effect associated with the laying on of hands. Complicating the measurement of outcome and the effectiveness of an MT is the placebo effect (a response resulting from the suggestion that something is beneficial, even though it may be inert). Although MT is not alone in its use of the placebo effect, it is increasingly important that clinicians determine the specific effects of everything they do.14
The strong placebo effect associated with the laying on of hands. Complicating the measurement of outcome and the effectiveness of an MT is the placebo effect (a response resulting from the suggestion that something is beneficial, even though it may be inert). Although MT is not alone in its use of the placebo effect, it is increasingly important that clinicians determine the specific effects of everything they do.14
 Many musculoskeletal conditions are self-limiting so that patients may improve with time regardless of the intervention.
Many musculoskeletal conditions are self-limiting so that patients may improve with time regardless of the intervention.
 The difficulty of blinding clinicians and subjects to the intervention the subjects are receiving.
The difficulty of blinding clinicians and subjects to the intervention the subjects are receiving.
 Clear-cut definitions as to when one technique is more efficacious than another are lacking.
Clear-cut definitions as to when one technique is more efficacious than another are lacking.
 Overreliance on MT techniques to improve a patient’s status is a passive approach in an era when patient independence is stressed.
Overreliance on MT techniques to improve a patient’s status is a passive approach in an era when patient independence is stressed.
CORRECT APPLICATION OF MANUAL TECHNIQUES
 Knowledge of the relative shapes of the joint surfaces (concave or convex). The concave–convex pattern of arthrokinematics, based on arthrology studies by Maitland,7 Kaltenborn,8,20 and MacConaill and Basmajian,21 have been taught in physical therapy schools in the United States for about 30 years.22 These patterns describe the roll and slide relationships that naturally occur between two moving articular surfaces, which depends on whether the convex or concave articular surface of the joint is considered the moving segment. For example, if the moving articular surface is convex relative to the other surface, the joint glide occurs in the direction opposite to the osteokinematic movement (angular motion). If, on the other hand, the moving articular surface is concave, the joint glide occurs in the same direction as the osteokinematic movement. It is important to remember that the concave–convex rule was not intended to establish the direction of the manual glide applied to the joint, but merely to describe the arthrokinematic pattern that minimizes the inherent migration of the center of the convex member in the direction of the roll.22 For example, a number of kinematic studies of the glenohumeral joint appear to conflict with the expected arthrokinematic for concave–convex surface movement by maintaining that the humeral head actually remains nearly stationary or, in fact, translates superiorly when performing 90–120 degrees of shoulder abduction.23,24 However, the net superior translation of the humeral head is only a few millimeters and is offset by a concurrent inferior slide of the humeral head.22
Knowledge of the relative shapes of the joint surfaces (concave or convex). The concave–convex pattern of arthrokinematics, based on arthrology studies by Maitland,7 Kaltenborn,8,20 and MacConaill and Basmajian,21 have been taught in physical therapy schools in the United States for about 30 years.22 These patterns describe the roll and slide relationships that naturally occur between two moving articular surfaces, which depends on whether the convex or concave articular surface of the joint is considered the moving segment. For example, if the moving articular surface is convex relative to the other surface, the joint glide occurs in the direction opposite to the osteokinematic movement (angular motion). If, on the other hand, the moving articular surface is concave, the joint glide occurs in the same direction as the osteokinematic movement. It is important to remember that the concave–convex rule was not intended to establish the direction of the manual glide applied to the joint, but merely to describe the arthrokinematic pattern that minimizes the inherent migration of the center of the convex member in the direction of the roll.22 For example, a number of kinematic studies of the glenohumeral joint appear to conflict with the expected arthrokinematic for concave–convex surface movement by maintaining that the humeral head actually remains nearly stationary or, in fact, translates superiorly when performing 90–120 degrees of shoulder abduction.23,24 However, the net superior translation of the humeral head is only a few millimeters and is offset by a concurrent inferior slide of the humeral head.22
 Duration, type, and irritability of symptoms6,7 (Table 10-3). This information can provide the clinician with some general guidelines for determining the intensity of the application of a selected technique (see “Indications for MT” later in this chapter).
Duration, type, and irritability of symptoms6,7 (Table 10-3). This information can provide the clinician with some general guidelines for determining the intensity of the application of a selected technique (see “Indications for MT” later in this chapter).
 Patient and clinician position. Correct positioning of the patient is essential both to help the patient relax and to ensure safe body mechanics from the clinician. When patients feel relaxed, their muscle activity is decreased, reducing the amount of resistance encountered during the technique. If appropriate, thermotherapy can be used prior to the treatment to warm the tissues around the joint, improve circulation, and relax the muscles.
Patient and clinician position. Correct positioning of the patient is essential both to help the patient relax and to ensure safe body mechanics from the clinician. When patients feel relaxed, their muscle activity is decreased, reducing the amount of resistance encountered during the technique. If appropriate, thermotherapy can be used prior to the treatment to warm the tissues around the joint, improve circulation, and relax the muscles.
 Position of structure to be treated. The position of the structure to be treated must be appropriate for the stage of healing, the technique to be applied, and the skill of the clinician. It is recommended that the resting position of the joint be used when the patient has an acute condition, or the clinician is inexperienced. The resting position, in this case, refers to the position that the injured joint adopts, rather than the classic resting (open-packed) position for a normal joint. Other positions for starting the mobilization may be used by a skilled clinician in patients with nonacute conditions. As the treatment progresses, the joint is positioned at or near the end of the available range prior to the application of the mobilization force so as to place the restricting tissue in its most stretched position.
Position of structure to be treated. The position of the structure to be treated must be appropriate for the stage of healing, the technique to be applied, and the skill of the clinician. It is recommended that the resting position of the joint be used when the patient has an acute condition, or the clinician is inexperienced. The resting position, in this case, refers to the position that the injured joint adopts, rather than the classic resting (open-packed) position for a normal joint. Other positions for starting the mobilization may be used by a skilled clinician in patients with nonacute conditions. As the treatment progresses, the joint is positioned at or near the end of the available range prior to the application of the mobilization force so as to place the restricting tissue in its most stretched position.
 Hand placement. Accurate hand placement is essential for efficient stabilization and for the accurate transmission of force. The hand should conform to the area being treated so that the forces are spread over a larger area. This larger contact surface is more comfortable for the patient. Typically, the proximal bone is stabilized using the clinician’s hands, a belt, or an assistant, and the distal bone is moved.
Hand placement. Accurate hand placement is essential for efficient stabilization and for the accurate transmission of force. The hand should conform to the area being treated so that the forces are spread over a larger area. This larger contact surface is more comfortable for the patient. Typically, the proximal bone is stabilized using the clinician’s hands, a belt, or an assistant, and the distal bone is moved.
 Specificity. Specificity refers to the exactness of the procedure and is based on its intent. Whenever possible, the forces imparted by a technique should occur at the point where they are needed. The clinician should check one joint at a time, one movement at a time.
Specificity. Specificity refers to the exactness of the procedure and is based on its intent. Whenever possible, the forces imparted by a technique should occur at the point where they are needed. The clinician should check one joint at a time, one movement at a time.
 Direction and type of force. The treatment force is applied as close to the opposing joint surface as possible. This necessitates that the clinician be able to identify anatomical landmarks as guides. Distraction techniques are perpendicular to the treatment plane, whereas gliding techniques are applied parallel to the treatment plane. When possible the clinician should work with the force of gravity rather than against it. The direction of the force can be either direct, which is toward the motion barrier or restriction,25 or indirect, which is away from the motion barrier or restriction.26,27 Although the rationale for a direct technique is easy to understand, the rationale for using an indirect technique is more confusing. A good analogy is a stuck drawer that cannot be opened. Often the movement that eventually frees the drawer is an inward motion, followed by a pull.19
Direction and type of force. The treatment force is applied as close to the opposing joint surface as possible. This necessitates that the clinician be able to identify anatomical landmarks as guides. Distraction techniques are perpendicular to the treatment plane, whereas gliding techniques are applied parallel to the treatment plane. When possible the clinician should work with the force of gravity rather than against it. The direction of the force can be either direct, which is toward the motion barrier or restriction,25 or indirect, which is away from the motion barrier or restriction.26,27 Although the rationale for a direct technique is easy to understand, the rationale for using an indirect technique is more confusing. A good analogy is a stuck drawer that cannot be opened. Often the movement that eventually frees the drawer is an inward motion, followed by a pull.19
 The amount of force. The amount of force used depends on the intent of the manual procedure and a number of other factors, including but not limited to
The amount of force. The amount of force used depends on the intent of the manual procedure and a number of other factors, including but not limited to
 the age, sex, and general health status of the patient;
the age, sex, and general health status of the patient;
 the barrier to motion and end-feel (stage of healing) (Table 10-4); and
the barrier to motion and end-feel (stage of healing) (Table 10-4); and
 the type and severity of the movement disorder.
the type and severity of the movement disorder.
 Reinforcement of any gains made. It has been demonstrated that movement gained by a specific manual technique performed in isolation will be lost within 48 hours, if the motions gained are not reinforced.28 Thus, the motions gained by a manual technique must be reinforced by both the mechanical and the neurophysiologic benefits of active movement, self-stretching, automobilization, and functional activities using the new range.29 These active movements must be as precise as possible to the involved segment or myofascial structure.
Reinforcement of any gains made. It has been demonstrated that movement gained by a specific manual technique performed in isolation will be lost within 48 hours, if the motions gained are not reinforced.28 Thus, the motions gained by a manual technique must be reinforced by both the mechanical and the neurophysiologic benefits of active movement, self-stretching, automobilization, and functional activities using the new range.29 These active movements must be as precise as possible to the involved segment or myofascial structure.
INDICATIONS FOR MT
 Mild musculoskeletal pain
Mild musculoskeletal pain
 A nonirritable musculoskeletal condition demonstrated by pain that is provoked by motion, but that disappears very quickly
A nonirritable musculoskeletal condition demonstrated by pain that is provoked by motion, but that disappears very quickly
 Intermittent musculoskeletal pain
Intermittent musculoskeletal pain
 Pain reported by the patient that is relieved by rest
Pain reported by the patient that is relieved by rest
 Pain reported by the patient that is relieved or provoked by particular motions or positions
Pain reported by the patient that is relieved or provoked by particular motions or positions
 Pain that is altered by changes related to sitting or standing posture
Pain that is altered by changes related to sitting or standing posture
CONTRAINDICATIONS TO MT
Absolute
 Systemic or localized infection (e.g., osteomyelitis), febrile state
Systemic or localized infection (e.g., osteomyelitis), febrile state
 Acute circulatory condition
Acute circulatory condition
 Malignancy
Malignancy
 An open wound at the treatment site, or sutures over the treatment site
An open wound at the treatment site, or sutures over the treatment site
 Recent fracture
Recent fracture
 Hematoma
Hematoma
 Hypersensitivity of the skin
Hypersensitivity of the skin
 Inappropriate end-feel (spasm, empty, and bony), or evidence of joint ankylosis, or joint hypermobility
Inappropriate end-feel (spasm, empty, and bony), or evidence of joint ankylosis, or joint hypermobility
 Advanced diabetes
Advanced diabetes
 Rheumatoid arthritis (in a state of an exacerbation)
Rheumatoid arthritis (in a state of an exacerbation)
 Cellulitis
Cellulitis
 Constant, severe pain, including pain at rest or that disturbs sleep, indicating that the condition is likely to be very irritable or in the acute stage of healing
Constant, severe pain, including pain at rest or that disturbs sleep, indicating that the condition is likely to be very irritable or in the acute stage of healing
 Extensive radiation of pain
Extensive radiation of pain
 Any condition that has not been fully evaluated
Any condition that has not been fully evaluated
Relative
 Joint effusion or inflammation
Joint effusion or inflammation
 Rheumatoid arthritis (not in a state of an exacerbation)
Rheumatoid arthritis (not in a state of an exacerbation)
 Presence of neurologic signs
Presence of neurologic signs
 Osteoporosis
Osteoporosis
 Pregnancy, if a technique is to be applied to the spine
Pregnancy, if a technique is to be applied to the spine
 Dizziness
Dizziness
 Steroid or anticoagulant therapy
Steroid or anticoagulant therapy
SOFT-TISSUE TECHNIQUES
Transverse Friction Massage
 Traumatic hyperemia.2 According to Cyriax, longitudinal friction to an area increases the flow of blood and lymph, which, in turn, removes the chemical irritant by-products of inflammation. In addition, the increased blood flow reduces venous congestion, thereby decreasing edema and hydrostatic pressure on pain-sensitive structures.
Traumatic hyperemia.2 According to Cyriax, longitudinal friction to an area increases the flow of blood and lymph, which, in turn, removes the chemical irritant by-products of inflammation. In addition, the increased blood flow reduces venous congestion, thereby decreasing edema and hydrostatic pressure on pain-sensitive structures.
 Pain relief. The application of TFM stimulates type I and II mechanoreceptors, producing presynaptic anesthesia. This presynaptic anesthesia is based on the gate theory of pain control (see Chapters 3 and 8). However, if the frictions are too vigorous in the acute stage, the stimulation of nociceptors will override the effect of the mechanoreceptors, causing the pain to increase. Occasionally, the patient may feel an exacerbation of symptoms following the first two or three sessions of the massage, especially in the case of a chronically inflamed bursa.42 In these cases, it is important to forewarn the patient.
Pain relief. The application of TFM stimulates type I and II mechanoreceptors, producing presynaptic anesthesia. This presynaptic anesthesia is based on the gate theory of pain control (see Chapters 3 and 8). However, if the frictions are too vigorous in the acute stage, the stimulation of nociceptors will override the effect of the mechanoreceptors, causing the pain to increase. Occasionally, the patient may feel an exacerbation of symptoms following the first two or three sessions of the massage, especially in the case of a chronically inflamed bursa.42 In these cases, it is important to forewarn the patient.
 Decreasing scar tissue. The transverse nature of the friction assists with the orientation of the collagen in the appropriate lines of stress and also helps produce hypertrophy of the new collagen. Given the stages of healing for soft tissue (see Chapter 2), light TFM should only be applied in the early stages of a subacute lesion, so as not to damage the granulation tissue. These gentle movements theoretically serve to minimize cross-linking and so enhance the extensibility of the new tissue. Following a ligament sprain, Cyriax recommends immediate use of gentle TFM to prevent adhesion formation between the tissue and its neighbors, by moving the ligamentous tissue over the underlying bone.2
Decreasing scar tissue. The transverse nature of the friction assists with the orientation of the collagen in the appropriate lines of stress and also helps produce hypertrophy of the new collagen. Given the stages of healing for soft tissue (see Chapter 2), light TFM should only be applied in the early stages of a subacute lesion, so as not to damage the granulation tissue. These gentle movements theoretically serve to minimize cross-linking and so enhance the extensibility of the new tissue. Following a ligament sprain, Cyriax recommends immediate use of gentle TFM to prevent adhesion formation between the tissue and its neighbors, by moving the ligamentous tissue over the underlying bone.2
Myofascial Release
Myofascial Stroking
 J stroke. This technique is used to increase skin mobility. Counterpressure is applied with the heel of the hand, while a stroke in the shape of the letter J is applied in the direction of the restriction, with two or three fingers, which creates some torque at the end of the stroke.
J stroke. This technique is used to increase skin mobility. Counterpressure is applied with the heel of the hand, while a stroke in the shape of the letter J is applied in the direction of the restriction, with two or three fingers, which creates some torque at the end of the stroke.
 Vertical stroke. The purpose of vertical stroking is to open up the length of vertically oriented fascia. As in the J stroke, counterpressure is applied with one hand, while the stroking is performed with the other.
Vertical stroke. The purpose of vertical stroking is to open up the length of vertically oriented fascia. As in the J stroke, counterpressure is applied with one hand, while the stroking is performed with the other.
 Transverse stroke. As its name suggests, the transverse stroke is applied in a transverse direction to the body. Force is applied downward into the muscle with the fingertips of both hands, and the force is applied slowly and perpendicular to the muscle fibers.
Transverse stroke. As its name suggests, the transverse stroke is applied in a transverse direction to the body. Force is applied downward into the muscle with the fingertips of both hands, and the force is applied slowly and perpendicular to the muscle fibers.
 Cross-hands technique. The cross-hands technique is used for the release of deep fascial tissues. The clinician places crossed hands over the site of restriction. The elastic component of the fascia is then stretched until the barrier is met. At this point, the clinician maintains a consistent, gentle pressure at the barrier for approximately 90–120 seconds. Once the release is felt, the clinician reduces the pressure.
Cross-hands technique. The cross-hands technique is used for the release of deep fascial tissues. The clinician places crossed hands over the site of restriction. The elastic component of the fascia is then stretched until the barrier is met. At this point, the clinician maintains a consistent, gentle pressure at the barrier for approximately 90–120 seconds. Once the release is felt, the clinician reduces the pressure.
Soft-Tissue Mobilization
Sustained Pressure
Ischemic Compression
General Massage
 Effleurage. This is a general stroking technique applied to the muscles and soft tissues in a centripetal direction (from distal to proximal), to enhance relaxation and increase venous and lymphatic drainage. The clinician applies a firm contact with the patient using the palms of the hand and, at the end of the stroke, lifts the hands from the patient’s skin and replaces them at the starting position.55 Oil or cream can be used to aid the stroking.
Effleurage. This is a general stroking technique applied to the muscles and soft tissues in a centripetal direction (from distal to proximal), to enhance relaxation and increase venous and lymphatic drainage. The clinician applies a firm contact with the patient using the palms of the hand and, at the end of the stroke, lifts the hands from the patient’s skin and replaces them at the starting position.55 Oil or cream can be used to aid the stroking.
 Stroking. Stroking techniques are applied superficially along the whole length of a surface. These techniques are typically applied previous to the deeper techniques of massage to enhance relaxation.54
Stroking. Stroking techniques are applied superficially along the whole length of a surface. These techniques are typically applied previous to the deeper techniques of massage to enhance relaxation.54
 Petrissage. This term is used to describe a group of techniques that involve the compression of soft-tissue structures and include kneading, wringing, rolling, and picking-up techniques, to release areas of muscle fibrosis and to “milk” the muscles of waste products that collect from trauma or abnormal inactivity.56
Petrissage. This term is used to describe a group of techniques that involve the compression of soft-tissue structures and include kneading, wringing, rolling, and picking-up techniques, to release areas of muscle fibrosis and to “milk” the muscles of waste products that collect from trauma or abnormal inactivity.56
 Strumming. The technique of perpendicular strumming involves the application of repeated, rhythmic deformations of a muscle belly in a strumming fashion.
Strumming. The technique of perpendicular strumming involves the application of repeated, rhythmic deformations of a muscle belly in a strumming fashion.
Acupressure
 The gate control theory of pain (see Chapter 3).
The gate control theory of pain (see Chapter 3).
 Diffuse noxious inhibitory control. This theory implies that noxious stimulation of heterotopic body areas modulates the pain sensation originating in areas where a subject feels pain.58
Diffuse noxious inhibitory control. This theory implies that noxious stimulation of heterotopic body areas modulates the pain sensation originating in areas where a subject feels pain.58
 Stimulation of the production of endorphins, serotonin, and acetylcholine in the central nervous system, which enhances analgesia.59–67
Stimulation of the production of endorphins, serotonin, and acetylcholine in the central nervous system, which enhances analgesia.59–67
Muscle Energy
 The technique, which involves a controlled effort in a controlled direction, commences from a controlled position. Eccentric, concentric, and isometric contractions, at varying levels of effort, are used in ME, within a range of movement controlled by the clinician.
The technique, which involves a controlled effort in a controlled direction, commences from a controlled position. Eccentric, concentric, and isometric contractions, at varying levels of effort, are used in ME, within a range of movement controlled by the clinician.
 The clinician balances the degree of force used, depending on the intention.
The clinician balances the degree of force used, depending on the intention.
 The force used is localized as much as possible to the joint in question. The localization of force is more important than the intensity of the force.
The force used is localized as much as possible to the joint in question. The localization of force is more important than the intensity of the force.
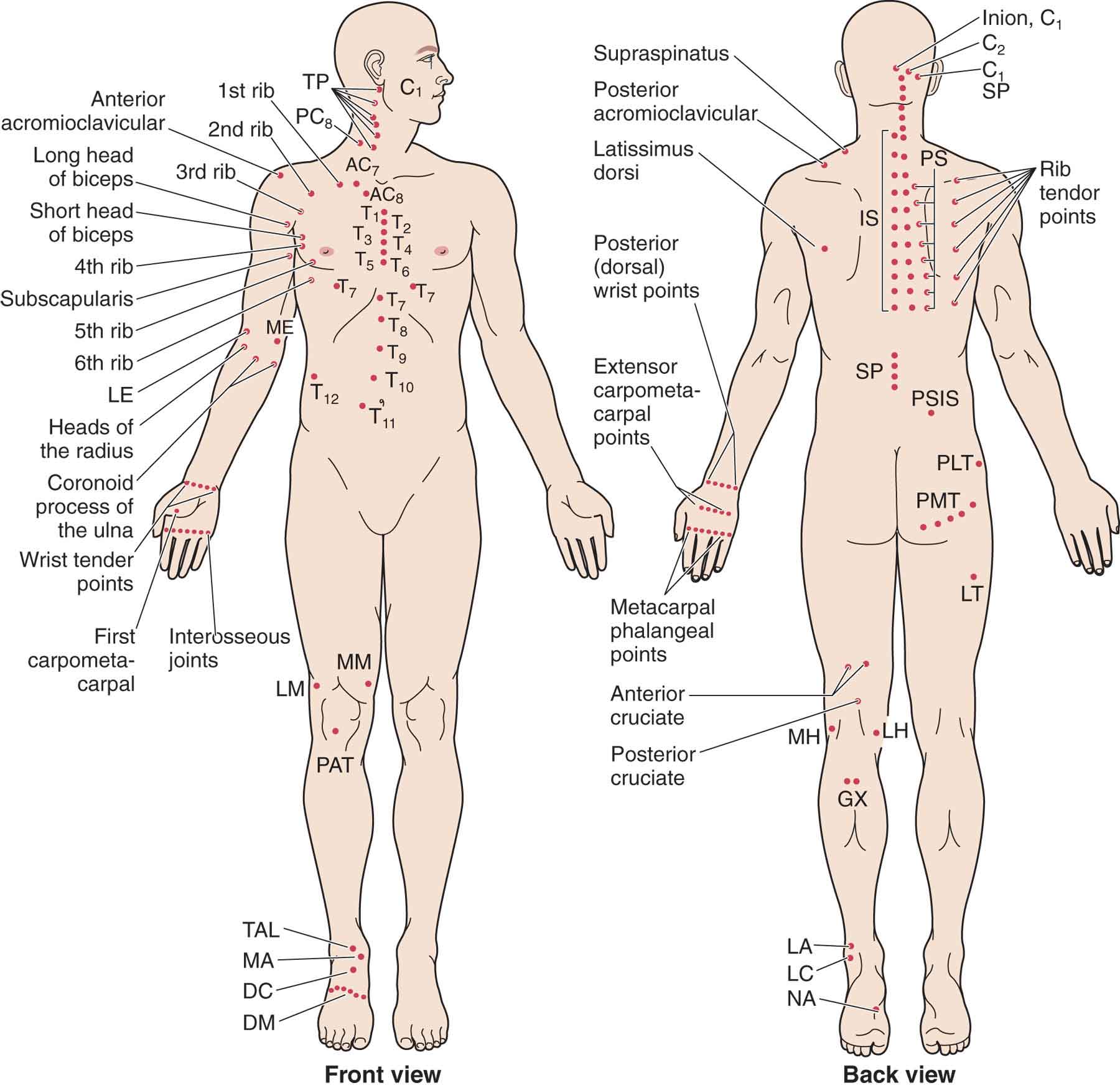
Strain–Counterstrain (Positional Release)
Manual Techniques
