Chapter 22 The Thoracic Outlet Syndrome: First Rib Subluxation Syndrome
Thoracic outlet syndrome, cervical ribs, interscalene triangle, trigger points, ischemic compression
After reading this chapter you should be able to answer the following questions:
| Question 1 | What are the anatomic boundaries of the thoracic outlet? |
| Question 2 | What are the contents of the thoracic outlet? |
| Question 3 | In which direction does the first rib commonly subluxate? |
| Question 4 | Which muscle group is frequently implicated in thoracic outlet syndrome? |
Significant confusion and controversy surround the thoracic outlet syndrome.1 Historically, anatomists refer to the superior aperture of the thorax as the thoracic inlet and to the diaphragm-covered inferior aperture as the thoracic outlet.2,3
Sir Ashley Cooper in 1821 first described the symptom complex of the thoracic outlet syndrome.4 Forty years later, Coote5 excised a cervical rib with successful obliteration of symptoms. Other earlier authors considered anatomic abnormalities of the cervical spine to be the primary cause of the vascular compression and resulting neurologic symptoms as thoracic outlet syndrome (TOS).6,7 By 1916 the presence of cervical ribs in 1% of the population had been established; however, only 10% of those were symptomatic.8
Further controversy and confusion stems from the fact that there are several subsets of syndromes. Adson and Coffey9 described the scalenus anticus syndrome and their diagnostic maneuver (Adson’s test) in 1927. Adson believed that intermittent vascular obstruction was pathognomonic of thoracic outlet syndrome.10 He surmised that arterial compression meant that the brachial plexus was also irritated. However, pulse obliteration can be found in 1% to 94% of completely normal subjects.11–13 The costoclavicular syndrome was described by Falconer and Weddell14 in 1943. Two years later, Wright13 identified the hyperabduction syndrome. It was Peet et al.15 who coined the broader term thoracic outlet compression syndromes (TOCS). Recently, Lee et al.16 and others17 proposed that subluxation of the first rib may irritate neurovascular structures at the cervicothoracic area and cause radicular symptoms in the arm, hand, and neck, commonly described as thoracic outlet syndrome.
Anatomic Features
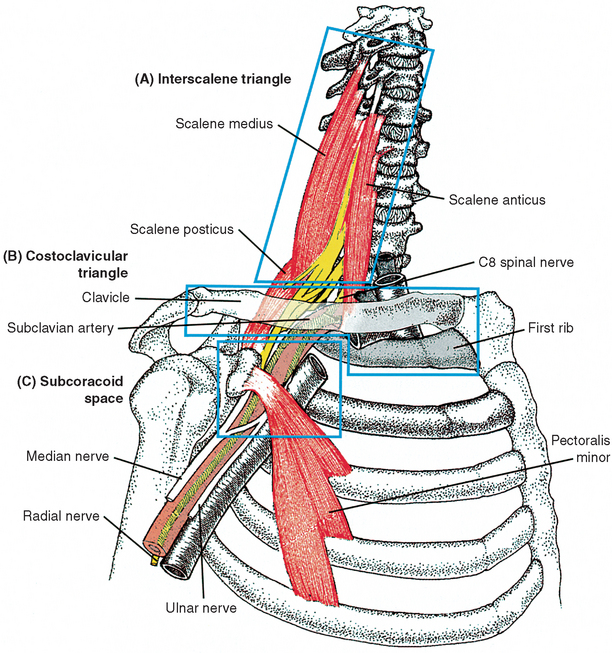
The “thoracic outlet” presents an opening bordered laterally by the first rib, medially by the vertebral column, and anteriorly by the claviculomanubrial complex. Contents of this thoracic outlet include the lower trunks of the brachial plexus and the subclavian artery (Figure 22-1). Anomalies in this region, including cervical ribs and fibrous bands, have been popularly linked to causation. The mere presence of an anatomic anomaly does not establish its causal relationship. Instead, the occurrence of neurovascular dysfunction at the thoracic outlet depends on the interplay of three conditions.18
Narrow Passages Traversed by the Neurovascular Bundle
Interscalene Triangle
The interscalene triangular space is bordered anteriorly by the scalene anticus muscle, posteriorly by the scalene medius muscle, and inferiorly by the medial border of the first rib. (See Figure 22-1, A.) This interscalene triangle transmits all trunks of the brachial plexus, but only the subclavian artery traverses this triangle, not the subclavian vein. The distance between the two scalenes at the base varies significantly.19 There are therefore occasions when both the artery and the nerve trunk are clamped within this tight fibrofascial triangle.20
Another anatomic variation is the slope of the first rib. If the slope is unusually steep, the artery would be firmly wedged between the rib and the tendon. This obliquity seems to be more marked in women21 and possibly in advancing age.
Costoclavicular Triangle
The neurovascular bundle immediately enters a second triangular space bounded anteriorly by the middle third of the clavicle, posteromedially by the anterior border of the first rib, and posterolaterally by the upper border of the scapula and the subscapularis muscle. (See Figure 22-1, B.) Both the upper and lower borders of this triangle are mobile; hence they are subject to physiologic narrowing, depending on the position of the arm and activities of the shoulder musculature.
Subcoracoid Space
The last narrow strait is provided by the insertion of the pectoralis minor tendon into the coracoid process. (See Figure 22-1, C.) During shoulder abduction, contraction of the pectoralis minor tendon may significantly narrow the subcoracoid space over the neurovascular structures.22–24
Physiologic Factors Compromising the Narrow Passages
Developmental Factors
In the upright position the space created between the clavicle and the first rib is chiefly determined by the inclination of the clavicle at the acromioclavicular joint. Aging leads to progressive acromioclavicular descent, which is more marked in women.20,24,25 This may explain the reason why women are four times more prone to develop TOS than are men.22,23,26
Anthropomorphic Factors
Acromioclavicular descent is also prominent in individuals with an asthenic physique, because the poorly developed shoulder muscles allow the scapula to rotate anteriorly and laterally. This is further aggravated by a long slender neck, wherein the cervical roots are even farther away from the costoclavicular passage, subjecting them to more exaggerated tension and angulation.27–29
Postural and Dynamic Factors
Certain body postures and arm positions may consistently produce symptoms. The most notable is hyperabduction and external rotation of the arm, such as sleeping with the arm behind the pillow. Occupations such as painting and automobile repair require the arm to be overhead for prolonged period. The anatomic mechanisms responsible for the symptoms in hyperabduction are costoclavicular compression and bowing of the axillary artery at the subcoracoid space.13,30,31 Abduction of the arm beyond 90 degrees requires external rotation of the scapula, which brings the clavicle upward and backward at the sternoclavicular joint, closing the costoclavicular space.13,23 Hyperabduction to 180 degrees is always accompanied by external rotation of the humerus, which tenses the costocoracoid ligament and the pectoralis minor, accentuating compression of the subclavian vein.23,32
Other symptom-producing factors may include wearing a heavy bag with a shoulder strap or carrying a heavy briefcase consistently with the same arm. In both situations the clavicle is brought directly or indirectly against the neurovascular bundle.33 Water skiers, whose arms are strenuously pulled forward and downward with the body tilted backward, compress the costoclavicular space as the neurovascular bundle is dragged against the first rib and the scalene anticus tendon. Hikers carrying bulky backpacks with cross-shoulder belts suffer lower plexopathy (back palsy)34 by the same mechanism, as do soldiers standing at attention for a prolonged period with shoulders drawn backward and chest thrust forward. These positions not only depress the clavicle but also elevate the first rib, thereby closing the costoclavicular passage.23
Another insidious compressive mechanism is deep inspiration, especially when forced or labored as in patients with emphysema. The first rib moves upward and forward during deep inspiration by as much as 34 mm and 22 mm, respectively, in men and by as much as 28 mm and 14 mm, respectively, in women.35 More importantly, this is repeated approximately 33,000 times each day. In patients with emphysema, the increased functional residual lung capacity keeps the first rib in an elevated position. Added to this are the repeated strained cervical movements during forced breathing, mediated to the first rib by the scalenes. The scalenes therefore hypertrophy and can potentially narrow the interscalene passage. In emphysema patients the neurovascular bundle is repeatedly subjected to stretch, compression, and friction.20,36
Structural Anomalies Compromising the Narrow Passages Further
Anomalous Ribs
The association of cervical rib with TOS is well documented. Its incidence in routine nonsymptomatic patients is 0.002% to 0.5%.9,37,38 Approximately 10% of those with cervical ribs experience symptoms. Familial occurrences with other congenital anomalies have been reported.20,39 It is more common on the left side, although bilateral cervical ribs were found in 50% of surgical candidates.24 It is believed that cervical ribs develop in intrauterine life more often with prefixed than with postfixed brachial plexus20 because of the lesser resistance encountered by the small first thoracic nerve root in a prefixed plexus.40 Rayan41 reports numbness and tingling in the forearms of a 14-year-old girl and a 12-year-old boy brought on by athletic activities at school and caused by a cervical rib articulating with the first rib on the symptomatic side. He believes that a cervical rib more than 5.5-cm long tends to lift up and kink the subclavian artery and stretch the seventh cervical nerve root. However, it is generally considered that abnormal fibrous bands extending from the tip of an incomplete cervical rib to the first rib are the most common causes of true TOS.1,11,20,22 Furthermore, these fibrous bands are clinically treacherous because they are invisible on x-ray films and may exist without concomitant rib anomalies.
Anomalous Muscle Insertions
Excessive and sustained scaleni muscle contraction has been thought to cause neurovascular symptoms,11,42,43 presumably by strangling the subclavian artery and neurovascular bundle. It is now believed that such muscular actions alone are unable to produce the symptoms without some form of anomalous muscle insertions.24,44 These anomalous muscle insertions may be a fused scalenus anticus and medius insertion that occupies an extended area over the middle third of the first rib,24 a split tendinous insertion of the scalenus medius muscle,33 or even a hypertrophied scalenus minimus muscle.20
Other Anomalies
A number of unusual causes have been reported in the literature as contributing to neurovascular compression in the costoclavicular compartment: fracture of the clavicle with subsequent pseudarthrosis,45 malunion of a clavicular fracture,46 unreduced dislocation of the clavicle,47 and other rare causative factors such as osteochondroma of the clavicle and first rib.26
Biomechanical Considerations
Functional Cause
Because chiropractors are intimately interested in symptom-causing functional disturbances of various kinds rather than anatomic or pathologic causes, it is not unusual that we see and recognize patients with symptoms of neurovascular compression syndromes related to functional disturbances at the cervicothoracic junction. One of the major anatomic structures that may be involved in patients presenting with brachialgia, paresthesias, and pain along the ulnar nerve distribution is the first rib. Lindgren and Leino48 reported on 22 cases of thoracic outlet syndrome-diagnosed patients who presented with a hypomobile first rib on the symptomatic side. They further reported on five additional TOS patients a year later49 in whom the hypomobile or subluxated first rib was confirmed by cineradiographic study. These same authors also believe that normal mobility of the first rib is necessary for normal function at the cervicothoracic area and normal function at the thoracic outlet.50
Lewit51 stated that there are different types of impingement syndromes. When the canal is through a solid bone or a single groove covered by soft tissues, surgical decompression is often necessary. However, when a canal is formed by bones linked by joints capable of movement, for example, the thoracic outlet, impairment of joint mobility must be taken into consideration in pathogenesis of an entrapment syndrome. Under such conditions impaired function is the first change. If this functional loss lasts for a period, the increased strain on corresponding soft tissues, muscles, and ligaments may cause thickening of the ligament and in the end damage the nerve. This pathophysiologic mechanism is commonly shared in manual medicine (Figure 22-2).52–56 If the offending structure is found to be a cause of functional disability as in joint dysfunction, treatment must be directed toward restoring that lost function. Lewit51 calls this “dynamic nerve compression” or nerve compression due to impaired function. Successful treatment can be achieved by manipulation.
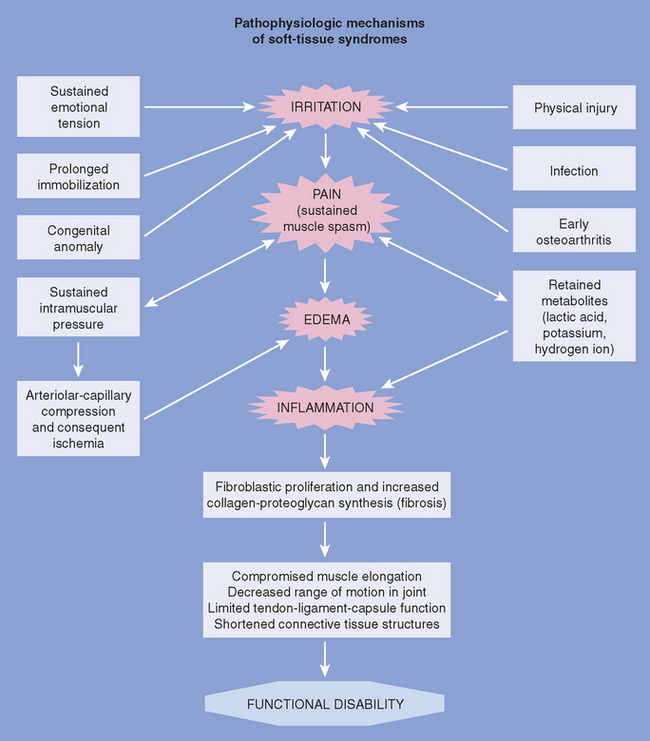
Figure 22-2 The pathophysiologic mechanism of functional disability.
(Modified from Bland JH. J Musculoskel Med 1986;3(11):23-41.)
Traumatic and Occupational Causes
Hargberg and Wegman57 and others58,59 evaluated the association and impact of occupational exposure and disorders of the shoulder and neck area. They found that certain tasks that are repetitive in nature or involve sustained handling of materials in primarily one direction such as is typical of assembly line workers (particularly sustained static contractions of the cervicothoracic muscles required to perform tasks at shoulder level) are clearly associated with shoulder-neck disorders.
Other commonly missed causative factors of TOS are adhesions and scarring associated with posttraumatic thoracic outlet syndrome. Dellon60 and others61 believe that rear end collisions cause a stretch type of injury to the brachial plexus with subsequent scarring that causes entrapment of the brachial plexus proximal to the first rib; hence such conditions are often missed in commonly used transaxillary first rib resections.
Clinical Features
From our discussion thus far, it is obvious that the clinical presentation is dependent on the underlying anatomic or functional disturbances with which patients present. In our experience, patients present with moderate symptoms with progressive deterioration, especially when symptoms are dominantly vascular. The opposite is true with neurologic dominance of symptoms. Presentations are commonly significant, especially to the patient, because they include numbness and weakness but improve gradually with conservative care (Box 22-1).
BOX 22-1 Symptoms of Thoracic Outlet Syndrome
Modified from Liebenson CS. J Manipulative Physiol Ther 1988;11:493-99.
The literature appears to selectively differentiate symptoms into (1) primarily vascular causes and vascular symptoms such as swelling, cyanosis, pallor, coolness, and ischemia; and (2) primarily neurologic causes such as numbness, tingling, and paresthesia. This may have prompted a number of authors to give subclassifications to various causative factors involved. Each of these syndromes had obvious pathognomonic diagnostic tests. Adson’s maneuver was specific for the scalenus anticus syndrome in which neurovascular compression occurred exclusively in the interscalene triangle. As a consequence, scalenectomy became the treatment of choice. Falconer and Weddell14 coined the term costoclavicular syndrome for those patients with positive exaggerated military maneuver, which is thought to narrow the costoclavicular space. Later Wright advocated the diagnostic category of hyperabduction syndrome for patients who became symptomatic with hyperabduction of the symptomatic arm.
Sensory Signs and Symptoms
The most common presenting symptoms of TOS are numbness and tingling. Sanders and Pearce62 found that 90% of TOS patients had paresthesia in the hand, 80% had arm pain, 86% had neck pain, and 69% had occipital headache. In their review of the TOS literature, Pang and Wessel18 noted that neurologic disturbances are caused by involvement of the C8 and T1 fibers in the lower trunk of the brachial plexus and that sensory disturbances usually appear in advance of motor signs.
The pain is usually described as a dull, constant, heavy ache, and its distribution does not respect the C8-T1 dermatomal pattern. It is often diffuse in the supraclavicular and shoulder area and spreads down the arm. Paresthesia, however, is frequently segmental and mostly felt in the inner aspect of the arm and forearm, the ulnar half of the hand, and the fourth and fifth digits, including the hypothenar eminence. Constant numbness and tingling in the ulnar digits are almost pathognomonic and certainly disturbing to the patient, but occasionally a burning sensation and sharp localized pain may be experienced.1 In some patients the pain is atypical, localized to the anterior chest wall, and may simulate angina pectoris (pseudoangina).36
Sensory symptoms are often precipitated by trauma to the shoulder girdle, a bout of heavy lifting or simply carrying heavy objects, or the habitual use of a heavy shoulder bag over the same shoulder. The pain is often aggravated by the use of the arm or arms because these symptoms are often bilateral.63 Pain is worse by the end of the day, particularly in occupations involving the use of the arms overhead. Many patients are awakened during the night by arm pain and paresthesia, especially if the affected arm is raised above the pillow. Ribbe et al.64 found that the most reliable symptoms were: (1) history of aggravation of symptoms with arm elevation, (2) history of C8-T1 paresthesia, (3) tenderness over the brachial plexus supraclavicularly, and (4) positive abduction and external rotation (AER) of the arm test. They found that three of these four tests were positive in 94% of thoracic outlet syndrome patients. This is considered the “TOS index.”
Arm positions that remove traction on the brachial plexus bring relief of symptoms. Patients often find relief in sitting with elevation of the shoulder by resting the affected elbow on the arm of the chair or supporting the elbow with the opposite hand. This maneuver is effective for any brachial plexus compression syndrome, not only for TOS.
With time, objective signs of sensory denervation appear, including diminished sensation to pinprick and light touch sensation over the C8-T1 dermatome. Initially this hypesthesia is patchy over the ulnar digits, but with time it becomes evenly distributed over the entire ulnar side of the hand.65 When this is correlated with digital tenderness over the scalene anticus and supraclavicular portion of the brachial plexus, three of the four items of the “TOS index” are satisfied and the diagnosis of TOS is certain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree