Chapter Three The theory of clinical reasoning in combined movement therapy
Introduction
This chapter introduces and discusses the clinical reasoning processes required to make the best decisions when assessing and managing patients with spinal pain syndromes. There is an increasing amount of attention given towards clinical reasoning in physiotherapy and manual therapy literature, which is an indication of the importance these processes can have on the progression of practice. The practical basis for considering clinical reasoning is simple: some clinicians get more people better, and quicker, than other clinicians. We call these people experts. These experts display characteristically different methods of assessing and managing patients than clinicians who do not have such high levels of success (Case et al, 2000; Doody & McAteer, 2003; James 2001; Jensen et al, 2000, 2007; King & Bithell, 1998; Resnik & Hart, 2003; Robertson, 1996; Roskell & Cross, 2001). The cognitive differences recognized in clinical practice are supported by decades of work in the psychology of expertise (Chase & Simon, 1973; Craik & Lockart, 1972; DeGroot, 1965; DeGroot & Gobet, 1996; Gobet & Simon, 1998, 2000; Gobet & Wood, 1999; Neisser, 1998). It would therefore be advantageous for all of us to try and behave like experts. Expertise is not simply proficiency in the physical application of technical skills. Of course, this excellence in technique is of vital importance in treating patients with a combined movement approach, but it is equally important to know precisely when, how, and with which patients to apply these techniques. This knowing, or cognitive level of the clinical process can be what we mean when we say ‘clinical reasoning’. Thus, it is the balance of thought and technique that produce excellence in practice:
Clinical reasoning has been defined as the cognitive process that incorporates thinking skills and knowledge (facts, procedures, concepts, principles and patterns) used to make clinical decisions and judgements through the evaluation, diagnosis and management of a patient problem (Jones, 1994). Models and definitions largely based on descriptions of clinical reasoning in medicine (Barrows & Feltovitch, 1987; Elstein et al, 1978; Feltovitch & Barrows, 1984; Groen & Patel, 1985) have been utilized and adapted to the physiotherapy process in a number of texts, e.g. Higgs & Jones (2000) and Jones (1994, 1995, 1997a, 1997b, 1997c). Additionally, alternative reasoning approaches to medicine-based modelling have been proposed from within the therapy professions, e.g. Bradnam (2002), Edwards et al (2006), Edwards et al (2004), Gifford (1998), Jette et al (2003), Ladyshewsky (2002), Rothstein et al (2003) and Steiner et al (2002). These authors, among many others authors, state quite convincingly that a meaningful appreciation of the cognitive processes underlying our decision-making is critical to the quality of our practice. This appreciation can, however, be difficult due to the complexity and unfamiliarity of the literature (Kempanien et al, 2003). With this in mind, this chapter attempts to discuss the complexities of clinical reasoning in a practical, meaningful and context-related way in relation to combined movement therapy (CMT).
Mechanic B scenario
• Diagnosis – a dirty fuel tank
• Outcome – you are advised to add injector cleaner to the full tank of fuel and drive fast at high revs to clean out the system, which you do. You then crash because the steering column was broken.
Mechanic B’s experience
Based on the above two accounts, we can consider the following questions:
• Is there a difference in experience between Mechanic A and Mechanic B?
• Is there a difference in knowledge of cars between Mechanic A and Mechanic B?
• Is there a difference in the way that each mechanic inquired about what had happened on the motorway?
• Is there a difference in the way in which each mechanic inspected your car?
• Is there a difference in the way each mechanic interpreted the information gained from the two points above?
• Is there a motivational difference between the two mechanics?
Their areas of inquiry are quite logical, and they may be the sort of questions you would instinctively want to ask – particularly if you had been unfortunate enough to have the experience of being assisted by Mechanic B! As well as being instinctive and logical, they also reflect a number of core principles of clinical reasoning. The similarity between the above scenario and clinical reasoning in manual therapy is not, however, due to chance – clinical reasoning is quite simply based in logic. It is made up of the sort of things that we naturally want to ask about when trying to work out what is happening in a given situation. Clinical reasoning has been meaningfully linked to, and often referred to as, ‘wise’ action (Butler, 2000). In the above scenario then, which mechanic displayed the wisest actions? The answer in this case is straightforward. It is now a matter of what constitutes this wise action and where this ‘wisdom’ comes from.
As stated already, the points above – asking about differences between the two mechanics – reflect an understanding of the underpinning principles of clinical reasoning. Higgs & Jones (2000) present a well-recognized and oft-quoted framework of clinical reasoning which we can use as a basis for considering how the clinical reasoning process can be harnessed in CMT. Figure 3.1 illustrates this framework.
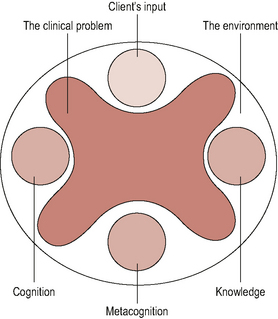
Figure 3.1 • Client-centred clinical reasoning. This framework represents the core components and the interactive thought process required for good reasoning. (Higgs & Jones, 2000)
Stages of reasoning in combined movement theory
• Early differential diagnosis (pattern recognition)
• Decision-making during the history-taking: what questions to ask and why (hypothetico-deductive reasoning)
• What do we know and how do we know it (the theory of knowledge)?
• Diagnostic testing (probability theory)
Stage 1: Pattern recognition
This is the first piece of information obtained. It may be written on your referral note for example. Research has demonstrated that expert practitioners begin the cognitive process of solving the problem from a very early stage of assessment and are able to recognize clinical patterns even at this early point (Barrows & Feltovitch, 1987; Jensen et al 2000; King & Bithell, 1998; Schon, 1991). The information above might not be much to go on, but it is arguably enough for the expert clinician to start to organize their thoughts and knowledge in order to make the next few minutes of the assessment more efficient and productive. Efficient organization of knowledge is a trait associated with expert practice (Rivett & Jones, 2004).
The brief information given above includes:
• Benign, neuromusculoskeletal (NMS)
• Cervicogenic headache and local somatic neck pain
• Possible structural causes, e.g. facet joint, peri-articular structures, local muscular causes, disc
• Inflammatory or degenerative disease
• Intracranial space occupying lesion (tumour)
• Intracranial vascular dysfunction (aneurysm, haemorrhage)
• Extracranial space-occupying lesion (tumour; arterial aneurysm)
• Non-neuromusculoskeletal tissue trauma (arterial dissection)
• Spinal cord/meningeal involvement
1. The patterns are now ‘set up’ in the clinician’s mind ready and waiting to be tested
2. The patterns may be prioritized, or at least the beginnings of the prioritization process may be in sight.
The second point relates to the clinician’s judgement of which of the above possibilities (patterns) are most likely and which are least likely to be the cause of the problem, given the information at hand. Detailed attention is given to this concept of probability later in the chapter, but for now, the clinician’s mind should be considering prioritization. In this case, the clinician might think: ‘I have experience of many male patients in this age group with unilateral pain such as this, and in my experience, most turn out to be treatable, benign NMS conditions, not many in this age group have had inflammatory or degenerative disease, and very rarely has this presentation been something serious’. Therefore, based on this clinician’s experience, the diagnosis is more likely to be a treatable NMS condition, and least likely (but not impossible) to be serious pathology or a red flag. The above is an example of how, at this stage, clinicians rely predominantly on their own experiences and observation to formulate potentially meaningful patterns (Elstein & Schwarz, 2000; Jones, 1999). Thus, the pattern recognition model of reasoning is reliant on experience (Simon, 1980). The value of this early recognition of patterns is predominantly the fact that it makes the process of ‘diagnosing’ quick and efficient. However, there are a few caveats with placing too much value and reliance on this model that should be considered before we proceed:
 Clinical relevance
Clinical relevance
Experience
Cognitive psychologists have suggested that it takes 10 years experience to become ‘expert’ in a discipline (Gobet & Wood, 1999). However, as others have pointed out (Rivett & Jones, 2004), simply gaining experience (as measured in time) is not enough. In order to display true proficiency, there must be other factors influencing the clinician’s development:
Using clinical experience and prior observation is prone to bias. This will be discussed in a psychological context below. However, on a very practical basis, it is important to consider that experiential observation can be influenced by biases of natural recovery, statistical regression, politeness of patients, placebo response and recall (Herbert, 2005).
Error
Some authors have highlighted the potential for error in the reasoning process (Rivett & Jones, 2004; Scott, 2000). The patterns that are recognized in this first stage will, in the majority of situations, later develop (generate) into testable hypotheses and it is this collection of hypotheses which will form the shape of the remaining assessment and examination process. Therefore, the whole diagnostic and decision-making procedure is reliant on the quality and accuracy of these early patterns. In respect of early pattern recognition, potential errors may take the form of developing the wrong initial concept of the problem; over-emphasis on favoured hypotheses, misinterpreting early information, making assumptions (this should be carefully considered as being very different to pattern recognition), considering too few (narrow range of) patterns (or hypotheses), making hypotheses too vague, and failing to detect early cues for serious pathology. There is equal potential for reasoning errors throughout the whole assessment procedure, but it is problems within the hypothesis generation stage that will misdirect the subsequent procedure. Hence utmost attention should be given to the potential for error at this stage.
The concept of error in pattern recognition is paradoxical: pattern recognition relies on experience yet it is that very experience which is the most likely cause of error in pattern recognition. Common errors, as stated above, include narrowness of hypotheses, misinterpreting information, and failure to recognize early signs of serious pathology. These errors are products of experience which have not been subject to the scrutiny of careful thought (cognition), reflection, critical analysis or self-monitoring (metacognition). In the absence of careful cognitive and metacognitive processing, external (to the clinician) experience may be internally (to the clinician) mis-interpreted. This is the psychological phenomenon of perception. The interpretation of any experience is subjective and specific to the individual. All external experiences are filtered through our own, personal schemata, which is itself developed by experiences. Thus, if we have psychological schemata which are built of aberrant/limited/biased interpretations of previous experiences, all future experiences are going to be interpreted within these skewed schemata. A good way of demonstrating this concept is with the use of an optical illusion (Fig. 3.2).
The image in Figure 3.2 has two interpretations: (1) an old woman and (2) a young girl. Now that you know this information, you should be able to see both interpretations (although some will still find this harder than others). However, if you did not know that there are two interpretations, you will probably only see one and be satisfied that this is a nice picture of either an old woman or a young girl. Each subsequent time you see the picture, you will automatically interpret the image you are familiar with, because your personal schemata has been ‘set up’ with this first experience. Additionally, each subsequent time that you see the image, your interpretation of whatever that early experience was will be reinforced. Therefore, you could coast through life believing that this picture has only a single interpretation and this belief would continue to get stronger and stronger, eventually becoming almost impossible to break away from. However, the critical reasoner would want to question their early experience of interpreting the picture. In this case, you could perhaps spend longer examining the image to see for yourself if there really was another interpretation. Or you could spend time thinking about whether there at least could be an alternative. Or you could challenge your own perception of the image and re-examine it. Or you could ask another viewer if they see the same thing as you. Better still, ask a number of other viewers to see what their interpretations are – the more viewers you ask, the more likely it would be that you would come across someone who has seen the alternative interpretation, thereby challenging your belief. These later activities are part of the cognitive/metacongnitive process associated with good reasoning and are more likely to reveal something closer to reality than just accepting the first interpretation. The continual inclusion of the reflective cognition/metacognition process is imperative in determining the quality of pattern recognition and hypothesis generation.
 Clinical relevance
Clinical relevance
Pattern recognition has been recognized for its many values, e.g. efficiency in dealing with a problem quickly without the need to clarify and re-check, efficiency in dealing with uncertainty, imprecise data, or limited premises (Albert et al, 1988). However, effective and efficient pattern recognition is reliant on the following three conditions being met:
If all three of these conditions are not in place, the process is prone to error (as discussed above) and the limitations of the logical basis of pattern recognition are exposed. The logical basis of pattern recognition is known as induction. Hence, pattern recognition is also referred to as ‘inductive reasoning’ (Higgs & Jones, 2000, p. 6). The basis of induction is one of making inferences about something from prior experience or observation(s) of a similar event. For example, I have switched my kettle on 200 times and it has never exploded, therefore I affirm that when I switch it on now (the 201st time), it will again not explode. This seems quite a reasonable assumption, and this logical process is largely what drives us to make all sorts of decisions and choices on a daily basis throughout our lives. However, there is a strong philosophical argument which challenges reliance on inductive reasoning and questions its logical basis. Consider the following inference:
Premise A: I have seen 20 patients this week whose headache was caused by upper cervical facet dysfunction.
Premise B: Upper cervical facet dysfunction causes headaches.
Conclusion: My next (21st) patient that I see with headache will have upper cervical facet dysfunction as the cause.
Consideration of the problems of induction is nothing new. The argument against inductivism was highlighted in the work of an eminent 20th century philosopher called Karl Popper. His claim was that adherence to an inductivist approach is erroneous and limited and that in order for a more accurate approximation to what is correct to be made, a deductive approach should be taken (Popper, 1980). Luckily, for us manual therapists, this has already been given some thought and forms the next stage in our reasoning process.
Stage 2: Hypothetico-deductive reasoning
Now that patterns have been recognized, the clinician has two choices:
1. Accept the most likely pattern as the diagnosis and begin treatment
2. Use these patterns to generate a number of hypotheses which can then be tested for their validity.
Option one would be an extreme form of expert practice and is totally reliant on the pattern recognition model. As stated above, this can be very quick and efficient. However, also as stated above, it will only work if certain conditions are met, and the model is prone to error and logical limitation. Therefore, for most people at most times, option two would be the most reasonable option. For the clinical reasoner, the rest of the history-taking is not a random, or even pre-structured, list of questions but a reasoned, hypothesis-driven process of inquiry. This process is referred to as a hypothetico-deductive model of reasoning, and is written about extensively in both general clinical reasoning (e.g. Barrows & Tamblyn, 1980; Elstein et al, 1978) and manual therapy specific clinical reasoning literature (e.g. Higgs & Jones, 1995; Jones, 1995; Rivett & Jones, 2004). The hypothetico-deductive model describes a process of data collection, hypothesis generation, interpretation and hypothesis testing. As stated earlier, in reality, a combination of various reasoning models will be operationalized, e.g. simply because we have now stated that the predominant process has evolved to a hypothetico-deductive structure does not mean that future patterns will not be recognized, and subsequently tested as hypotheses, and so on. However, for clarity, at this point we shall focus our attention on hypothetico-deductive reasoning.
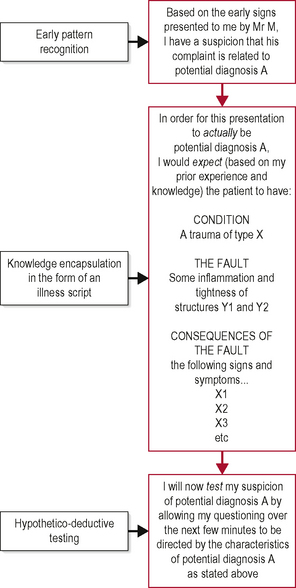
It was suggested above that superior, efficient organization of knowledge was a cognitive ability commonly attributed to the expert practitioner. This process can be clearly demonstrated at this stage of the assessment process. A natural cognitive link between the early recognition of patterns and the subsequent testing of those patterns is the organization, or encapsulation, of the clinician’s existing knowledge in the form of ‘packaged’ lists of characteristics/information regarding what actually constitutes each pattern. These packages of pattern-specific information have been referred to as ‘illness scripts’ (Feltovitch & Barrows, 1984). More recent work has identified this theoretical notion as an integral component of efficient reasoning (Boshuizen & Schmidt, 2000; Rivett & Jones, 2004; Sefton et al, 2000). Figure 3.3 demonstrates the temporal operationalization between the early recognition of patterns, the instantaneous formulation of illness scripts, and the subsequent guiding of hypothesis-driven questioning.
In the middle box representing the illness script in Figure 3.3, you will notice that the ‘script’ is separated into three distinct components, i.e. potential diagnosis A is conditional of (1) there being a specific type of trauma, (2) that specific tissues have been affected, and (3) that the manifestation of (1) and (2) are a specific set of signs and symptoms. Boshuizen and Schmidt (2000) refer to these three components as:
The enabling conditions are the conditions under which the problem/disease may occur, and considers such information as social history, hereditary conditioning, medical or environmental background, etc. The fault refers to the actual pathophysiological process taking place for this problem/disease. The consequences of the fault are therefore those clinically observable signs and symptoms considered to be associated with the specific problem/disease. For our case study we can construct examples of possible illness scripts which may be associated with the patterns recognized early on for our 38-year-old male with neck and head pain. Table 3.1 shows three patterns (for illustrative purposes, only three patterns have been used in this example – of course, it is probable that, in reality, there would be more than three potential diagnoses) and the associated illness scripts which could be potential diagnoses for this patient.
Table 3.1 Example of three patterns and associated illness scripts related to the case study of upper cervical neck pain and headache
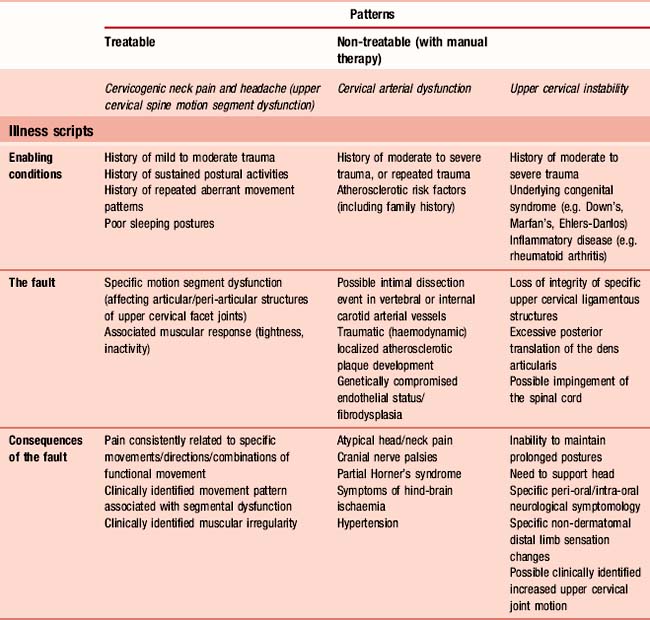
Premise A: all treatable cervicogenic headache and neck pain is differentially characterized by features X, Y and Z (as encapsulated in the specific illness script).
Premise B: Mr M has features X, Y, and Z.
Conclusion: Mr M has treatable cervicogenic headache and neck pain.
Stage 3: What do we know and how do we know it? Knowledge
Knowledge is a key component in the framework of clinical reasoning (see Fig. 3.1). As stated above, the validity of the deductive logical inference is dependent on the quality of knowledge which supports its premises. If our reasoning is reliant on our knowledge, we must consider the nature and quality of our knowledge, and question where it comes from.
• The type of knowledge (i.e. pain related to upper cervical evil spirits) is not valid
• The source of this knowledge (i.e. knowledge acquired from the shaman) is also not valid.
Table 3.1 suggests a number of characteristics (in the form of illness scripts) suggestive of each proposed hypothesis. We can now question the quality of this information and examine where this information comes from, i.e. how do we know that characteristics X, Y, Z equate to diagnosis A.
Types of knowledge
Types, or forms, of knowledge have been discussed and presented in a number of therapy-specific texts and publications, e.g. Higgs et al (2004), Higgs and Titchen (2000), Jones (1995), Resnik and Hart (2003), Resnik and Jensen (2003) and Swisher (2002). Classically, types of knowledge have been sub-divided into the categories which are shown in Figure 3.4.
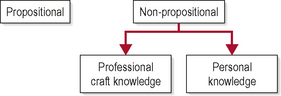
Figure 3.4 • Types of knowledge. Propositional know-that knowledge and non-propositional know-how knowledge.
The interested reader is referred to Higgs and Titchen (2000) and Higgs et al (2004) for detailed information regarding this classification. In summary, propositional knowledge is knowledge about propositions! Propositions are the assertion that something is the case, e.g. the sun is the centre of our universe. In manual therapy, propositional knowledge refers to theoretical or scientific knowledge derived through scientific study and accessed through publicly available information sources such as peer-reviewed journal articles and books. Thus propositional knowledge is know-that knowledge. Professional craft knowledge is that which relates to actual practice skills, information, and competencies required of clinicians and is acquired through experience and is often tacit or ‘sub-conscious’. Personal knowledge is similarly gained through social (clinical) experiences but refers to that reflective, more conscious component of practice which forms our individualized frames of references, values and beliefs. Professional craft knowledge could, for example, include the manual skill needed to assess upper cervical passive physiological movement dysfunction as learnt on a post-graduate course and practised over a period of time. Personal knowledge, however, would be that independent, unique appreciation of what ‘stiffness’ actually feels like, or where ‘resistance’ begins, etc. Professional and personal knowledge are forms of ‘non-propositional’ knowledge and are related to ability, i.e. I am able to accurately assess resistance on this regular combined movement pattern and am able to make judgement on the degree of stiffness. Thus, these types of knowledge are often referred to as know-how knowledge.
The importance of attempting to understand types of knowledge is to make a judgement, as inferred above, on the quality of that knowledge. An expert practitioner will not only have more knowledge, but will utilize different knowledge types (compared to a novice), in turn from a variety of logically valid sources (Boshuizen & Schmidt, 2000; Gobet, 1998; Gobet & Wood, 1999; Jensen et al, 2000; King & Bithell, 1998).
Sources of knowledge
Personal experience
As stated, non-propositional sources rely on experience. Earlier in the chapter, we considered the limitations of individual experience as the dominant basis for reasoning. Therefore, significant reliance on personal experience can be erroneous in the reasoning process and it has been demonstrated in study that experience alone is not enough to form the basis of expert practice (e.g. King & Bithell, 1998). However, there are strong arguments for continued attention towards the importance of non-propositional knowledge in clinical reasoning (Higgs et al, 2004; Higgs & Titchen, 2000). The mechanism for ensuring that perception of personal experience is not distorted and misinterpreted is to devise mechanisms of continual reflection of practice. This is, of course, the advantage that personal knowledge has over professional craft knowledge. Without this component of reflection, experience is arguably the simple collection of data which is then used to inform the next judgement and as such is prone to the logical limitations of inductive logic. Reflective practice, therefore, should be considered the backbone to the reasoning process, and the interested reader is directed to the work of Donald Schon (1991) for further detail regarding reflective practice.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree