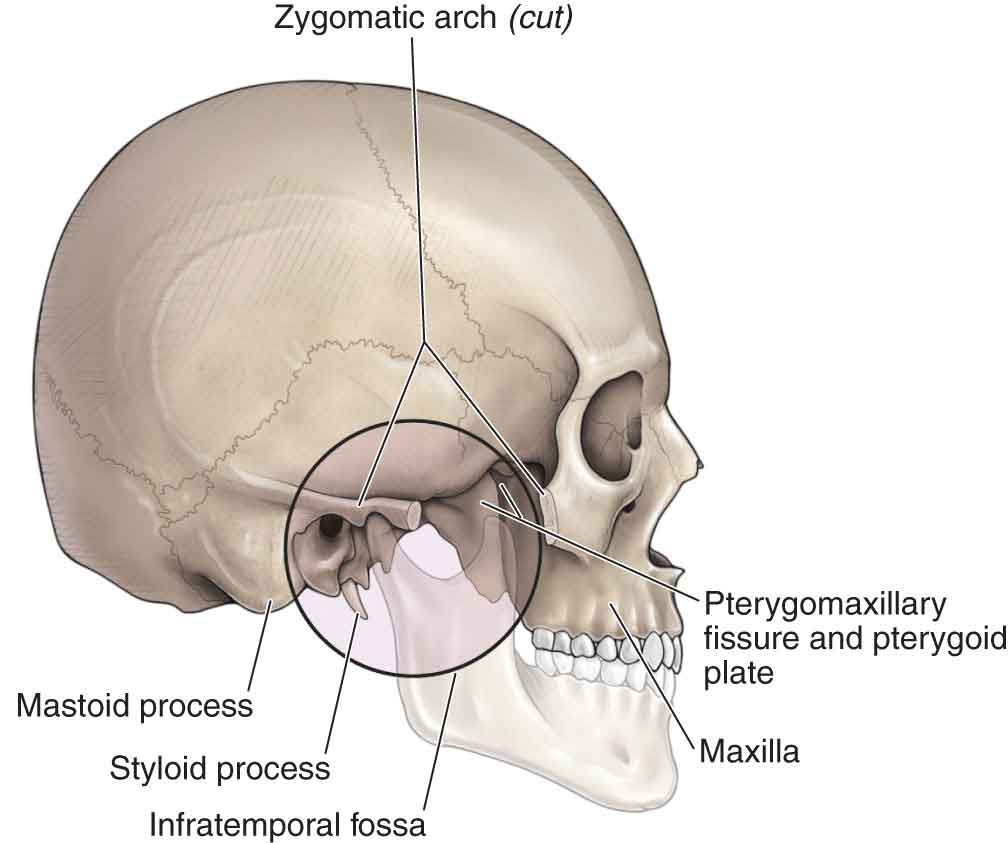
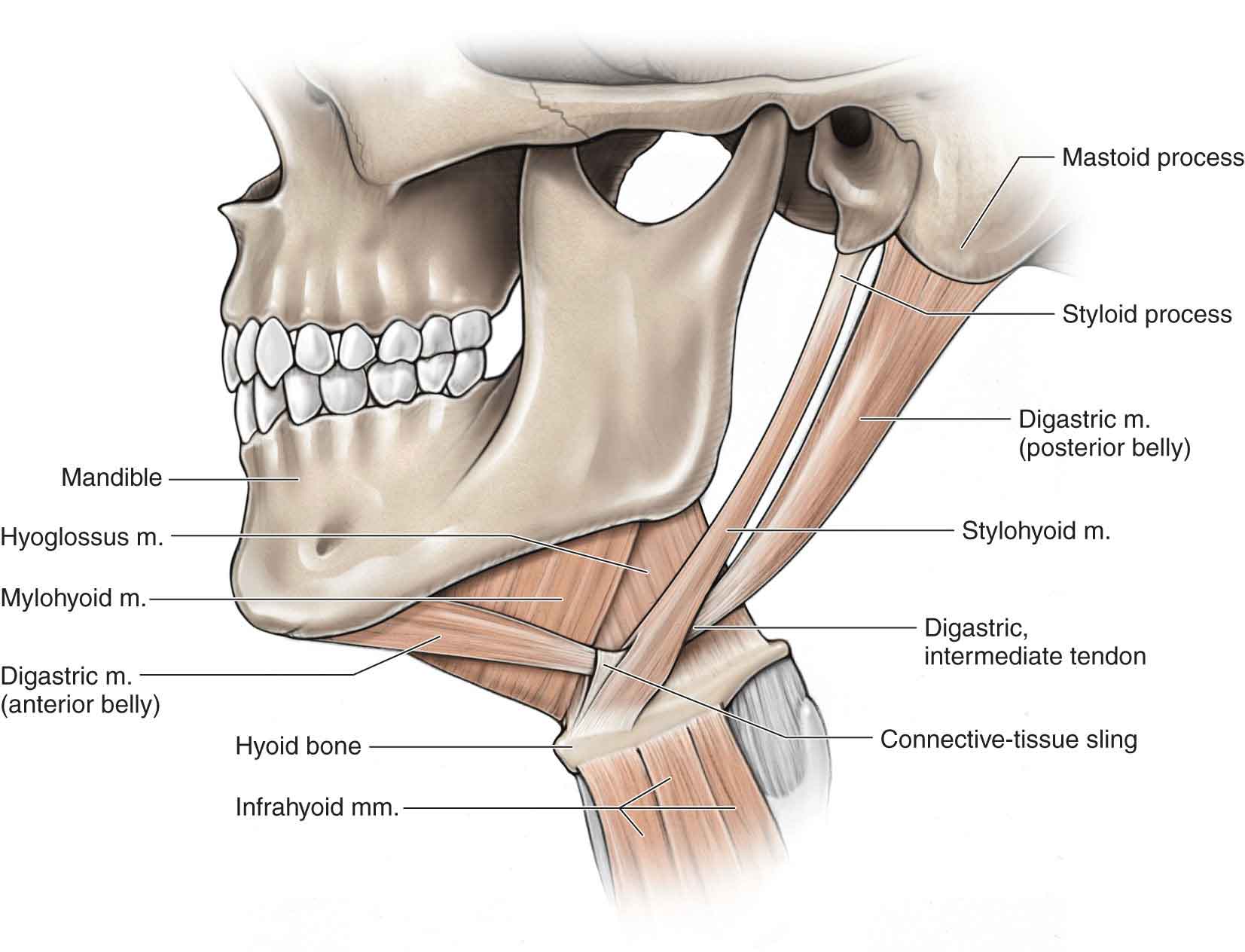
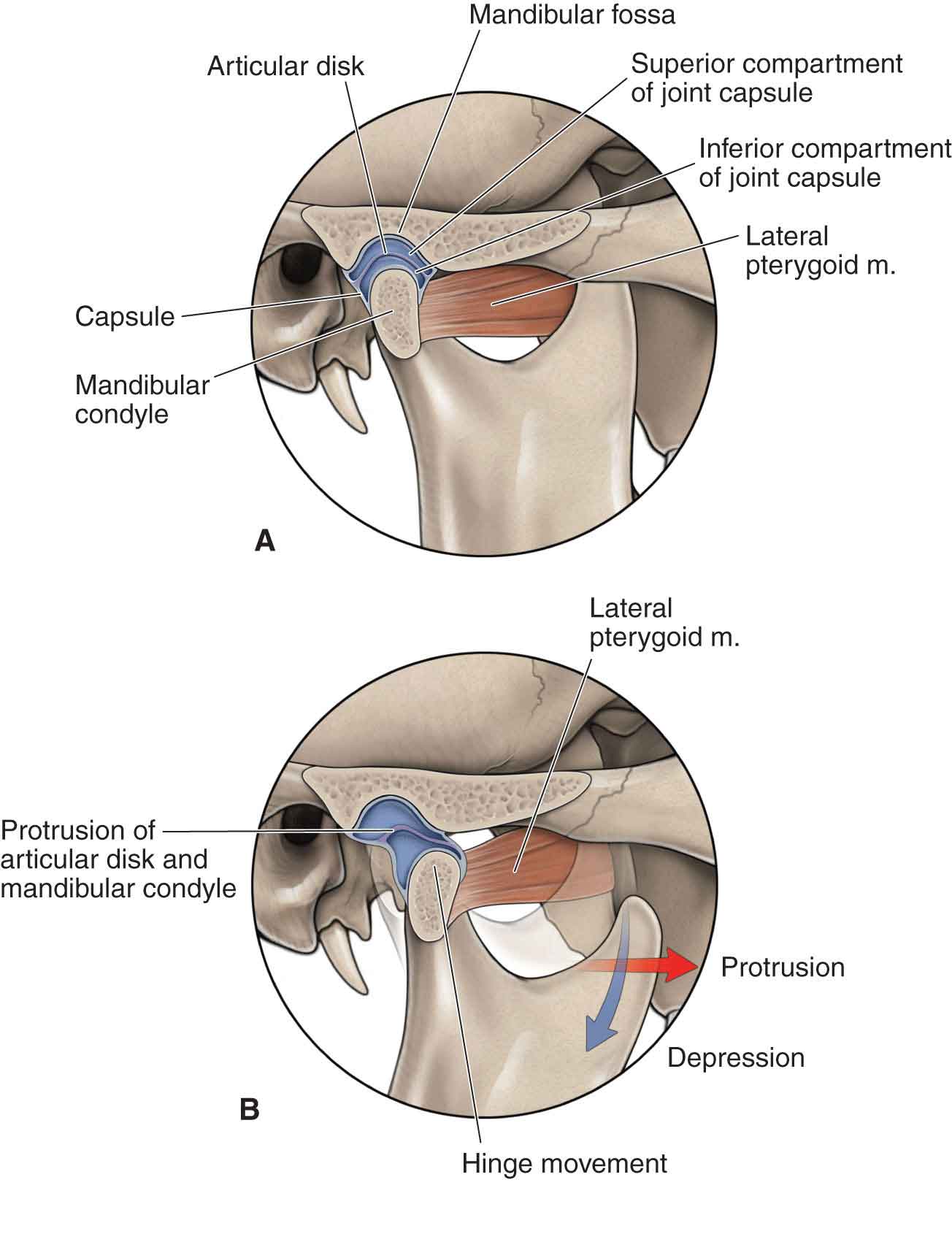
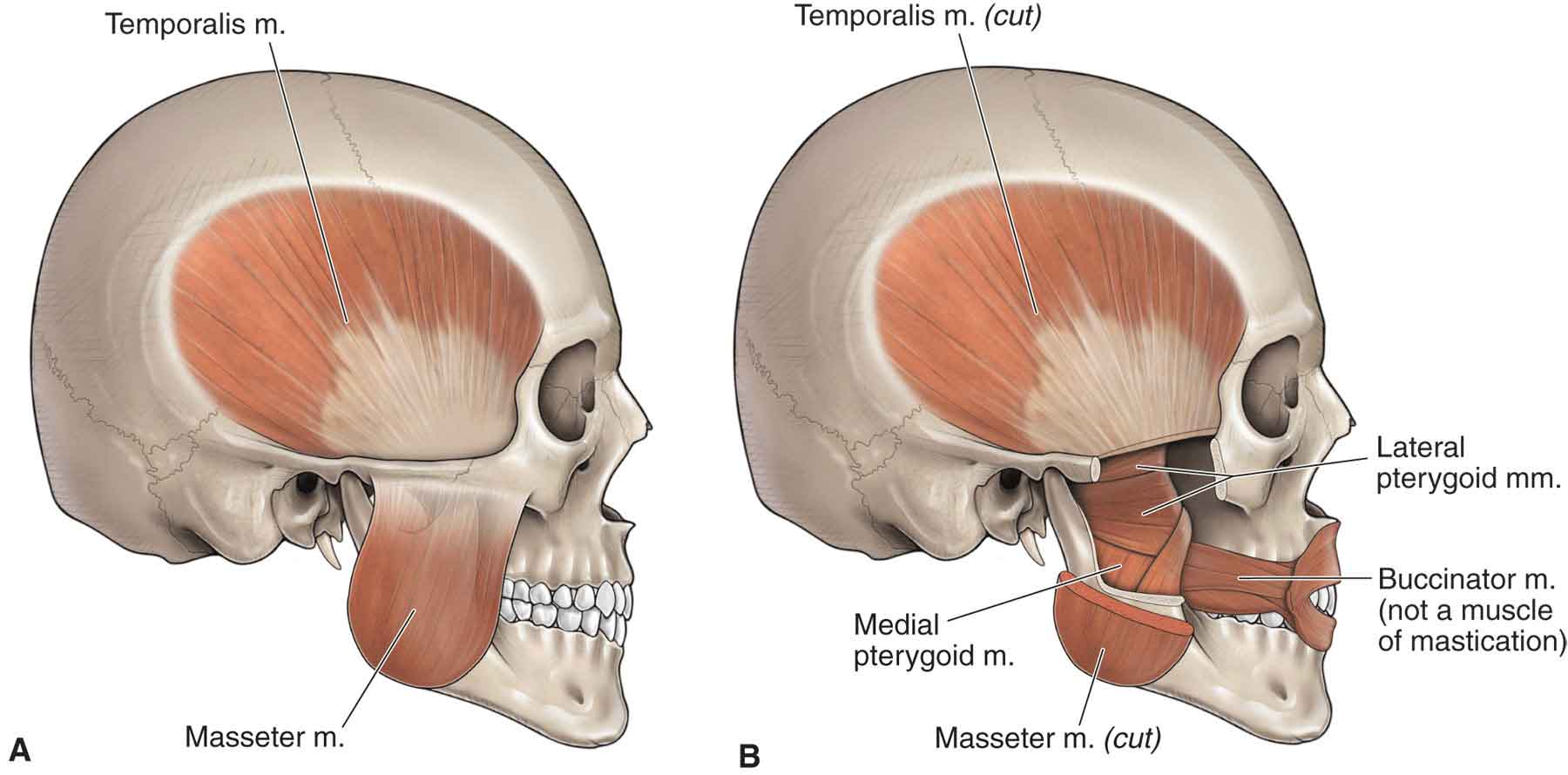
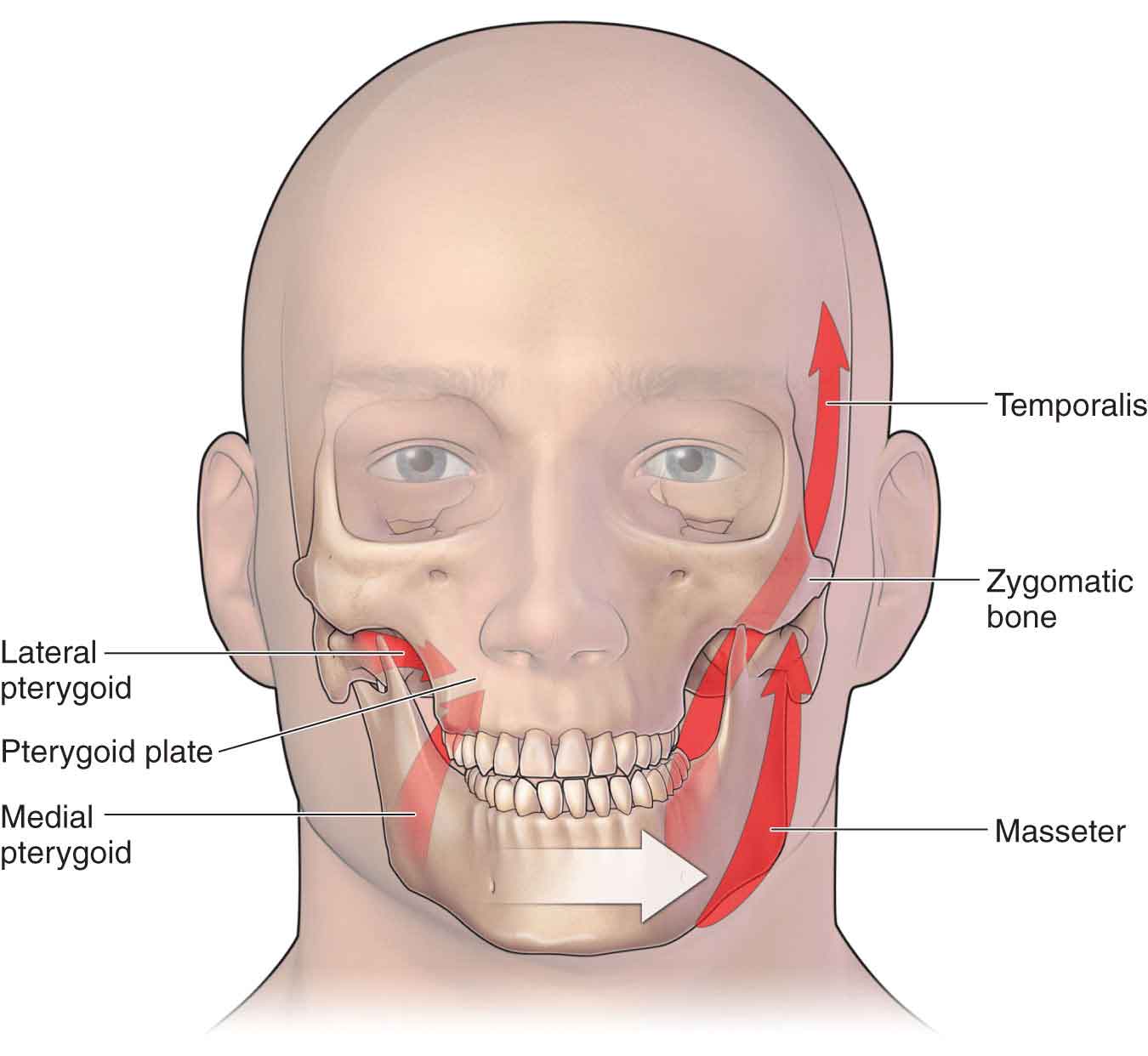
Approximately 50–75% of the general population has experienced unilateral temporomandibular joint dysfunction (TMD) on a minimum of one occasion and that at least 33% have reported a minimum of one continuing persistent symptom.1,2 TMD is a collective term used to describe a number of related disorders affecting the stomatognathic system and its related structures, all of which may have common symptoms. The term TMJ dysfunction as an overall descriptor of stomatognathic system dysfunction has been discontinued because it implies structural problems when none may exist, and does not include the many other factors that may be involved.3 Housed within the skull are the components of the stomatognathic system, which includes the TMJ, the masticatory systems, and the related organs and tissues such as the inner ear and salivary glands.4 An interrelationship exists between the stomatognathic system and the head and neck due to their proximity and shared embryological development. An understanding of this relationship is vital to understand the reasons for the myriad of symptoms that this region can exhibit. The embryologic structures from which the head, the face, and the neck originate are segmentally organized during development with the appearance and modification of six paired branchial or pharyngeal arches.4 These branchial arches contain the cranial nuclei of the trigeminal nerve (ophthalmic; maxillary and mandibular), the facial, the glossopharyngeal, and the laryngeal branch of the vagus nerve as well as the hypoglossal nerve. The first of these arches, the mandibular arch, consists of a large anterior (ventral) part (the mandibular process of Meckel’s cartilage) and a small posterior (dorsal) (maxillary) process. As development progresses, both processes disappear except for two small portions at the posterior (dorsal) ends, which persist. The first brachial arch forms The second pharyngeal arch (the hyoid arch) consists of Reichert’s cartilage. This arch is involved in the formation of The third pharyngeal arch is involved in the formation of the greater cornu of the hyoid and its body, the stylopharyngeal muscle, and the sensory apparatus of the posterior one-third of the tongue. The fourth pharyngeal arch combines with the sixth arch to form the thyroid, cricoid, and arytenoid cartilages of the larynx. The muscles derived from this arch are the pharyngeal constrictors (the cricothyroid) and the intrinsic muscles of the larynx. The pharyngeal constrictors are innervated by the superior laryngeal branch of the vagus nerve. The intrinsic muscles of the larynx are innervated by the recurrent laryngeal branch of the vagus nerve. In primitive creatures, and the human fetus, vibrations through the jaw are used as a basis for hearing. At around 8½ weeks, the small bones of the inner ear (the malleus, incus, and stapes) can be seen as distinct entities. The development of the malleus bone and the tensor tympani are intimately related to that of the lateral pterygoid muscle. Due to this embryological relationship, it is theorized that a spasm of the lateral pterygoid muscle can increase the tension within the tensor tympani (similar to that of a drum skin)4 resulting in increased sensitivity to pitch and vibration. Theoretically, this increased tension could produce sensorineural tinnitus, or ringing in the ears,4 a common associated symptom of a TMD, and an injury to the craniovertebral region. The diagnosis of TMD, like that of whiplash syndrome, remains controversial.5 This is due in part to a paucity of studies regarding the incidence, course, management, and prognosis of claimed TMDs.6,7 However, reports of TMD appear to be quite common. Although 50–75% of the general population has at least one sign of a TMD, only around one in four people with signs is actually aware of, or reports, any symptoms,8,9 and only about 5% of people with one or more signs of a TMD will actually seek an intervention.9–11 TMD tends to affect women more often than men,12 specifically women over the age of 55.13 After a technology assessment conference in 1996 about managing TMD, the National Institutes of Health (NIH) concluded that the natural history and etiology of TMD are not well understood and that most TMD symptoms are self-limiting, can recur, and may fluctuate over time.14 The most common TMD by far, comprising 90–95% of all TMD cases, is a condition with multiple musculoskeletal facial pain complaints and a variety of jaw impairments, without an identified structural cause.15 Due to the complex interplay between the sympathetic and trigeminal nervous systems and an increased understanding of the centralization of pain, TMD is best approached as a cluster of related disorders in the stomatognathic system that have many causes and common symptoms.16 There are likely three etiologic factors of TMD: (1) predisposing factors, (2) precipitating or triggering factors, and (3) perpetuating or sustaining factors17: Thus, the clinical course of TMD does not reflect a progressive disease but rather a complex disorder that is molded by many interacting factors, such as stress, anxiety, and depression, which serve to maintain the disease.16 Headaches, orofacial pain, earache, and neck pain are common complaints. A diagnosis of TMD must, therefore, include an examination of all of the following: Given the number of potential causes of jaw and face pain, a diagnosis of TMD can rarely be ascribed solely to the TMJ. Examples of appropriate diagnoses for TMD are more likely to include Nonsurgical interventions such as counseling, physical therapy, pharmacotherapy, and occlusal splint therapy continue to be the most effective way of managing more than 80% of patients with TMD.16 Although dentists are the primary professionals involved in the examination and intervention of TMD, physical therapists can play an important role in assisting the dentist in restoring function to the stomatognathic system. However, the procedures in physical therapy intervention are not well described in the literature in this area. The TMJ (Fig. 26-1) is a synovial, compound, modified ovoid bicondylar joint, which is formed between the articular eminence of the temporal bone, the intra-articular disk, and the head of the mandible. FIGURE 26-1 The temporomandibular joint. (Reproduced, with permission, from Chapter 21. Infratemporal Fossa. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The TMJ is unique in that, even though the joint is synovial, the articulating surfaces of the bones are covered not by hyaline cartilage but by fibrocartilage.19,20 Fibrocartilage has the same general properties found in hyaline cartilage but tends to be less distensible, owing to a greater proportion of dense collagen fibers (see Chapter 1). The development of fibrocartilage over the load-bearing surface of the TMJ indicates that the joint is designed to withstand large and repeated stresses and that this area of the joint surface has a greater capacity to repair itself than would hyaline cartilage.21 The area of load bearing is affected by the congruity of the contacting tooth surfaces (occlusion), head position, and the coordination of muscle function. The fibrocartilage is at its thinnest at the roof of the fossa, but load bearing here occurs only in the presence of dysfunction.22 The mandible works like a class-three lever (see Chapter 1), with its joint as the fulcrum. Although there is no agreement among the experts concerning force transmission through the joint, there does appear to be agreement that postural impairments of the cervical and upper thoracic spine can produce both pain and impairment of the TMJ.8 A number of bony components make up the masticatory system: the maxilla and the mandible, which support the teeth, and the temporal bone, which supports the mandible at its articulation with the skull. The sphenoid bone and the hyoid bone also could be included, because they provide important anatomic and functional links to the TMJ. The borders of the maxillae extend superiorly to form the floor of the nasal cavity as well as the floor of each orbit (Fig. 26-1). Inferiorly, the maxillary bones form the palate and the alveolar ridges, which support the teeth. The maxillae and mandible each contains 16 permanent teeth. The structure of each tooth reflects its function in mastication. The greater wings of the sphenoid bone form the boundaries of the anterior part of the middle cranial fossa. From these greater wings, the pterygoid laminae serve as the attachments for the medial and lateral pterygoid muscles. The U-shaped hyoid bone (Fig. 26-2), also known as the skeleton of the tongue, serves as the attachment for the infrahyoid muscles and for some of the extrinsic tongue muscles. The hyoid bone is involved with the mandible to provide reciprocal stabilization during swallowing and chewing. Theoretically, due to its muscle attachments, the position of the hyoid bone can be affected by cervical and shoulder positions, as occurs during forward head posture, which changes the length–tension relationships. FIGURE 26-2 The hyoid bone and related muscles. (Reproduced, with permission, from Chapter 25. Overview of the Neck. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The mandible, or jaw (Fig. 26-1), which supports the lower teeth, is the largest and the strongest bone in the face. It is suspended below the maxillae by muscles and ligaments that provide it with both mobility and stability. The medial surface of the mandible serves as the attachment for the medial pterygoid and the digastric muscles. The platysma, mentalis, and buccinator gain attachment on its lateral aspect. Two broad, vertical rami extend upward from the mandible: the condyle and the coronoid process. The anterior of the two processes, the coronoid, serves as the attachment for the temporalis and masseter muscles.23 The condyle process articulates with the temporal bone. The bony surfaces of the condyle and the articular portion of the temporal bone are made of dense cortical bone. The articulating surface of the condyle is flattened from front to back with its medial–lateral length twice as long as its anterior–posterior length. The condyles are generally convex, possessing short bony projections known as medial and lateral poles.24 The mandibular fossa of the temporal bone is divided into two surfaces: articular and nonarticular.24 The articulating surface of the temporal bone is made up of a concave mandibular, or glenoid, fossa and a convex bony prominence called the articular eminence.25 The articular tubercle, situated anterior to the glenoid fossa, serves as an attachment for the temporomandibular (or lateral) ligament.23 The nonarticular surface of the fossa consists of a very thin layer of bone and fibrocartilage that occupies much of the superior and posterior walls of the fossa.24 Located between the articulating surface of the temporal bone and the mandibular condyle is a fibrocartilaginous disk (sometimes inappropriately referred to as “meniscus”) (Fig. 26-3). The biconcave shape of the disk is determined by the shape of the condyle and the articulating fossa.26 Rees20 has described the fibrocartilaginous disk as having three clearly defined transverse, ellipsoidal zones that are divided into three regions—posterior band, intermediate zone, and anterior band—of which the intermediate zone makes contact with the articular surface of the condyle. FIGURE 26-3 The TMJ disk and the pterygoid. (Reproduced, with permission, from Chapter 21. Infratemporal Fossa. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) Both the disk and the lateral pterygoid muscle develop from the first branchial arch, and there is very little differentiation among the muscle, the disk, and the joint capsule.27,28 The fibrocartilaginous disk is tethered by a number of structures: The disk usually is located on top of the condyle in the 12 o’clock to 1 o’clock position on the mandibular head when the jaw is closed.31 Since the only firm attachment of the disk to the condyle occurs medially and laterally, the disk can move somewhat independently of the condyle.32 The disk effectively divides the TMJ into a lower and an upper joint cavity (see Fig. 26-3): Blood vessels and nerves are found only in the thickened periphery of this disk, especially its posterior attachment; its middle articular portion is avascular and aneural.33 The supporting structures of the TMJ consist of periarticular connective tissue (ligament, tendon, capsule, and fascia). As its name implies, the periarticular connective tissue serves to keep the joints together and to limit the ranges of motion at the joint. For example, the ligaments of the TMJ protect and support the joint structures and act as passive restraints to joint movement. The synovial cavities are surrounded by loose connective tissue rather than by ligaments. The intercapsular structures are located posteriorly to the condyle. Anterior to the joint are the muscles of the medial and lateral pterygoid (see next section). There are no well-defined anterior or posterior ligaments between the mandibular condyle and the temporal bone. However, two strong ligaments help to provide joint stability: Two other ligaments assist with joint stability: The muscles of mastication are the key muscles when discussing TMD. Three of these muscles, the masseter, the medial pterygoid, and the temporalis (Fig. 26-4), function to raise the mandible during mouth closing. The lateral pterygoid and digastric muscles work together to depress the mandible during mouth opening. FIGURE 26-4 Lateral view of TMJ. (Reproduced, with permission, from Chapter 21. Infratemporal Fossa. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) Although these muscles work most efficiently in groups, an understanding of the specific anatomy and action(s) of the individual muscles is necessary for an appreciation of their coordinated function during masticatory activity (Tables 26-1 and 26-2). TABLE 26-1 Muscles of the Temporomandibular Joint Muscle Proximal Distal Innervation Medial pterygoid Medial surface of lateral pterygoid plate and tuberosity of maxilla Medial surface of mandible close to angle Mandibular division of trigeminal nerve Lateral pterygoid Greater wing of sphenoid and lateral pterygoid plate Neck of mandible and articular cartilage Mandibular division of trigeminal nerve Temporalis Temporal cranial fossa By way of a tendon into medial surface, apex, and anterior and posterior borders of mandibular ramus Anterior and posterior deep temporal nerves, which branch from anterior division of mandibular branch of trigeminal nerve Masseter Superficial portion: from anterior two-thirds of lower border of zygomatic arch; deep portion from medial surface of zygomatic arch Lateral surfaces of coronoid process of mandible, upper half of ramus, and angle of mandible Masseteric nerve from anterior trunk of mandibular division of trigeminal nerve Mylohyoid Medial surface of mandible Body of hyoid bone Mylohyoid branch of trigeminal nerve and mandibular division Geniohyoid Mental spine of mandible Body of hyoid bone Anterior (ventral) ramus of C1 via hypoglossal nerve Stylohyoid Styloid process of temporal bone Body of hyoid bone Facial nerve Anterior and posterior digastric Internal surface of mandible and mastoid process of temporal bone By intermediate tendon to hyoid bone Anterior: mandibular division of trigeminal nerve; posterior: facial nerve Sternohyoid Manubrium and medial end of clavicle Body of hyoid bone Ansa cervicalis Omohyoid Superior angle of scapula Inferior body of hyoid bone Ansa cervicalis Sternothyroid Posterior surface of manubrium Thyroid cartilage Ansa cervicalis Thyrohyoid Thyroid cartilage Inferior body and greater horn of hyoid bone C1 via hypoglossal nerve TABLE 26-2 Actions of the Temporomandibular Joint Muscles Action Muscles Acting Opening of mouth Lateral pterygoid Mylohyoid Geniohyoid Digastric Closing of mouth Masseter Temporalis Medial pterygoid Protrusion of mandible Lateral pterygoid Medial pterygoid Masseter Mylohyoid Geniohyoid Digastric Stylohyoid Temporalis (anterior fibers) Retraction of mandible Temporalis (posterior fibers) Masseter Digastric Stylohyoid Mylohyoid Geniohyoid Lateral deviation of mandible Lateral pterygoid (ipsilateral muscle) Medial pterygoid (contralateral muscle) Temporalis Masseter The temporalis muscle (Fig. 26-4) has its origin from the floor of the temporal fossa and the temporal fascia. The muscle travels inferiorly and anteriorly to insert on the anterior border of the coronoid process and the anterior border of the ramus of the mandible. The temporalis muscle is innervated by a branch of the mandibular division of the trigeminal nerve. In addition to assisting with mouth closing and side-to-side grinding of the teeth, the temporalis muscle provides a good deal of stability to the joint. The masseter (Fig. 26-4) is a two-layered quadrilateral-shaped muscle. The superficial portion arises from the anterior two-thirds of the lower border of the zygomatic arch. The deep portion arises from the medial surface of the zygomatic arch. Both sets of fibers blend anteriorly and form a raphe with the medial pterygoid.25 The masseter inserts on the lateral surface of the coronoid process of the mandible, the upper half of the ramus and angle of the mandible. The masseter muscle is innervated by a branch of the mandibular division of the trigeminal nerve. The major function of the masseter is to elevate the mandible, thereby occluding the teeth during mastication. The medial pterygoid muscle is a thick quadrilateral muscle, with a deep origin situated on the medial aspect of the mandibular ramus (Fig. 26-4). The muscle travels posteriorly to insert on the inferior and posterior aspects of the medial subsurface of the ramus and angle of the mandible. The medial pterygoid muscle is innervated by a branch of the mandibular division of the trigeminal nerve. Working bilaterally, and in association with the masseter and temporalis muscles, the medial pterygoids assist in mouth closing. Individually, the medial pterygoid muscle is capable of deviating the mandible toward the opposite side. The medial pterygoid muscle also assists the lateral pterygoid and anterior fibers of the temporalis muscle to produce protrusion of the mandible. Two divisions of the lateral pterygoid muscles are recognized, each of which is functionally and anatomically separate (Figs. 26-3 and 26-4). The superior head arises from the infratemporal surface of the greater wing of the sphenoid. The inferior head arises from the lateral surface of the lateral pterygoid plate. Despite several investigations,38–40 no consensus has been reached regarding the insertion of the lateral pterygoid muscle. However, the most commonly described insertion is at the anterior aspect of the neck of the mandibular condyle and capsule of the TMJ. The lateral pterygoid muscle is innervated by a branch of the mandibular division of the trigeminal nerve. The superior head of the lateral pterygoid is involved mainly with chewing and functions to rotate the disk anteriorly on the condyle during the closing movement.41,42 It has also been suggested that in normal function of the craniomandibular complex, the superior lateral pterygoid plays an important role in stabilizing and controlling the movements of the disk.43 The inferior head of the lateral pterygoid muscle exerts an anterior, lateral, and inferior pull on the mandible, thereby opening the jaw, protruding the mandible, and deviating the mandible to the opposite side. The infrahyoid muscles comprise the sternohyoid, omohyoid, sternothyroid, and thyrohyoid muscles (Fig. 26-5). FIGURE 26-5 The infrahyoid muscles. (Reproduced, with permission, from Chapter 25. Overview of the Neck. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) The sternohyoid muscle is a strap-like muscle that functions to depress the hyoid and assist in speech and mastication. The omohyoid muscle, situated lateral to the sternohyoid, consists of two bellies and functions to depress the hyoid. In addition, the muscle has been speculated to tense the inferior aspect of the deep cervical fascia in prolonged inspiratory efforts, thereby releasing tension on the apices of the lungs and on the internal jugular vein, which are attached to this fascial layer.25 The sternothyroid and thyrohyoid muscles (see Fig. 26-5) are located deep to the sternohyoid muscle. The sternothyroid muscle is involved in drawing the larynx downward, whereas the thyrohyoid depresses the hyoid and elevates the larynx. These infrahyoid muscles are innervated by fibers from the upper cervical nerves. The nerves to the lower part of these muscles are given off from a loop, the ansa cervicalis (cervical loop) (see Chapter 3). The suprahyoid muscles (Fig. 26-2), working with the infrahyoid muscles, play a major role in coordinating mandibular function, by providing a firm base on which the tongue and mandible can be moved. The geniohyoid muscle is a narrow muscle situated under the mylohyoid muscle. The muscle functions to elevate the hyoid bone. As its name suggests, the digastric muscle consists of two bellies. The posterior belly arises from the mastoid notch of the temporal bone while the anterior belly arises from the digastric fossa of the mandible. The posterior belly is innervated by a branch of the facial nerve. The anterior belly is innervated by the inferior alveolar branch of the trigeminal nerve. The two bellies of the digastric muscle are joined by a rounded tendon that attaches to the body and greater cornu of the hyoid bone through a fibrous loop or sling.25 Bilaterally, the two bellies of the digastric muscle assist in forced mouth opening by stabilizing the hyoid. The posterior bellies are especially active during coughing and swallowing.25 This flat, triangular muscle is functionally a muscle of the tongue, stabilizing or elevating the tongue while swallowing and elevating the floor of the mouth in the first stage of deglutition.25 The stylohyoid muscle elevates the hyoid and base of the tongue and has an undetermined role in speech, mastication, and swallowing. The TMJ is primarily supplied by three nerves that are part of the mandibular division of the fifth cranial (trigeminal) nerve (Fig. 26-6) (Box 26-1). Portions of the middle ear ossicles, middle ear musculature, and muscles of mastication all originate from the first branchial arch and are innervated by this nerve. Therefore, in a patient with altered bite mechanics, spasm of the muscles of mastication caused by a displaced condyle may cause neuromuscular dysfunction of all the muscles innervated by the trigeminal nerve, including the tensor palatini.44 FIGURE 26-6 The trigeminal nerve. (Reproduced, with permission, from Chapter 17. Cranial Nerves. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) There is considerable clinical interest in the interactions between the cervical and craniofacial regions. This interest stems from a number of reports concerning patients who have pain in the cervical and craniofacial areas simultaneously.32,45–48 In the suboccipital region, a series of dense neural connections, called the trigeminocervical complex, exists among trigeminal, facial, glossopharyngeal, and vagus nerves, with those of the upper C1–4 cervical spinal nerves (Fig. 26-7).17 Postural abnormalities resulting from various acute or chronic etiologies that produce suboccipital compression may, therefore, be responsible for craniofacial pain anywhere in the head, in addition to symptoms of dizziness or nystagmus.7,17,49 FIGURE 26-7 Neurology of the TMJ. (Reproduced, with permission, from Chapter 21. Infratemporal Fossa. In: Morton DA, Foreman K, Albertine KH. eds. The Big Picture: Gross Anatomy. New York, NY: McGraw-Hill; 2011.) TMJ-related headaches usually include pain near the TMJ and ear, ear fullness, temporal headaches, and facial pain.50 The dizziness associated with TMD tends to be of the nonvertiginous variety, with the patient complaining of unsteadiness, giddiness, or lightheadedness.51 Although the exact mechanism is unclear, postural influences, alteration in the position of the jaw by the malocclusion, and the subsequent mismatching between the cervical muscles might be the cause.51 The movements that occur at the TMJ are extremely complex. The TMJ has three degrees of freedom, with each of the degrees of freedom being associated with a separate axis of rotation.52 Two primary arthrokinematic movements (rotation and anterior translation) occur at this joint around three planes: sagittal, horizontal, and frontal. Rotation occurs from the beginning to the midrange of movement. In addition to the rotational motions during mouth opening and closing and lateral deviations, movements at the TMJ involve arthrokinematic rolls and slides. Gliding, translation, or sliding movements occur in the upper cavity, whereas rotation or hinged movement occurs in the lower cavity. The motions of protrusion and retrusion are planar glides. Thus, Occlusal positions are functional positions of the TMJ. The occlusal position is defined as the point at which contact between some or all of the teeth occurs. Under normal circumstances, the upper molars rest directly on the lower molars and the upper incisors slightly override the lower incisors. The ideal position provides mutual protection of the anterior and posterior teeth, comfortable and painless mandibular function, and stability.17 Mouth opening occurs in a series of steps (Table 26-3). In the erect position, the condyles begin to rotate anteriorly and translate inferiorly and laterally during the first 25 degrees of opening as the jaw opens. The upper head of the lateral pterygoid muscle and the anterior head of the digastric muscle draw the disk anteriorly and prepare for condylar rotation during movement.32 This initial condylar rotation occurs as the mandibular elevators (masseter, temporalis, and medial pterygoid muscles) gradually relax and lengthen, allowing gravity to depress the mandible (see Fig. 26-8).32 The directions of the fibers of the lateral and medial temporomandibular ligaments also keep the condyle from moving posteriorly. The fibrous capsule and parts of the temporomandibular ligament limit excessive lateral movement of the condyle. The rotation occurs through the two condylar heads between the articular disk and the condyle. As the mandible moves forward on opening, the disks move medially and posteriorly until the collateral ligaments, and the lateral pterygoid stop their movement. During the last 15 degrees of opening, the rotation ceases due to tightening of the collateral ligaments, and is replaced by an anterior translation of the condyles (see Fig. 26-8).56 During this translation, the condyle and disk move together. The anterior translation, which is produced mainly by muscle contraction, serves to prevent mandibular encroachment of the anterior neck structures. Opening is also assisted by the other suprahyoid muscles.32 In extremely wide opening, such as that occurs with yawning, the functional joint contact is on the distal aspect of the condyle, and the anterior lateral aspect of the condyle contacts the posterior part of the masseter muscle. In this position, the soft-tissue structures are in a position of stretch, making them more prone to dysfunction.57 FIGURE 26-8 Mouth opening and closing. TABLE 26-3 Arthrokinematic Steps of the Temporomandibular Joint Step Movement Rest position Joint is in an open-packed position Rotation There is a mid-opening Condylar joint surfaces glide forward, inferior joint surface of disk has a relative posterior glide, upper lateral pterygoid relaxes, inferior pterygoid contracts, and posterior connective tissue is in a functional state of rest Functional opening Disk and condyle experience a short anterior translatory glide; superior and inferior heads of lateral pterygoid contract to guide disk and condyle forward Posterior connective tissue is in a functional tightening Translation There is full opening Disk and condyle glide anteriorly and caudally Superior and inferior heads of lateral pterygoid contract to guide disk and condyle fully forward Posterior connective tissues tighten Closure Surface of condyle joint glides posteriorly, and disk glides relative to anterior surface Superior head of lateral pterygoid contracts and inferior head relaxes Posterior connective tissue returns to its functional length Data from Rocabado M. Arthrokinematics of the temporomandibular joint. In: Gelb H, ed. Clinical Management of Head, Neck and TMJ Pain and Dysfunction. Philadelphia, PA: WB Saunders; 1985. Closing of the mouth involves a reversal of the movements described for mouth opening. The condyles translate posteriorly as a result of an interaction between the retracting portions of the masseter and temporalis muscle and the retracting portions of the mandibular depressors (see Fig. 26-8).52 As the condyles translate posteriorly and glide medially, they hinge on the disks. The disks then glide posteriorly and superiorly on the temporal bone along with the condyles (as a result of the actions of the masseter, medial pterygoid, and temporalis muscles).42 When the jaws are closed to maximal occlusal contact, the condyles contact the disks, and the disks contact the posterior slopes of the articular tubercles and the glenoid fossae. Protrusion is a forward movement of the mandible that occurs at the superior joint compartments, which consists of the disk and condyle moving downward, forward, and laterally. The muscles responsible for protrusion are the anterior fibers of the temporalis and the medial and lateral pterygoid muscles. Retrusion is a backward movement of the mandible, produced by the posterior fibers of the temporalis and assisted by the suprahyoid muscles. The retrusive range is limited by the extensibility of the temporomandibular ligaments.58 If a protrusion movement occurs unilaterally, it is called a lateral excursion, or deviation. For example, if only the left TMJ protrudes, the jaw deviates to the right. Lateral movements of the mandible are the result of asymmetric muscle contractions (Fig. 26-9). During a lateral excursion to the right, the condyle and the disk on the left side glide inferiorly, anteriorly, and laterally in the sagittal plane and medially in the horizontal plane along the articular eminence. The condyle and the disk on the right side rotate laterally on a sagittal plane and translate medially in the horizontal plane while remaining in the fossa. FIGURE 26-9 Lateral deviation to the left. The close-packed position of the TMJ is difficult to determine because the position of maximal muscle tightness is also the position of least joint surface congruity and vice versa. Rocabado56 considers there to be two close-packed positions, named according to the end position of the mandibular head in the fossa: Under this premise, the open-packed, or “rest” position is any position away from the anterior or posterior close-packed positions of the joint.56 The rest position, or “freeway space” corresponds to the position of the TMJ where the residual tension of the muscles is at rest and no contact occurs between maxillary and mandibular teeth. In this position, the tongue is against the palate of the mouth with its most anterior–superior tip in the area just posterior to the rear of the upper central incisors.59 The capsular pattern of the TMJ is a limitation of mouth opening. If one joint is more involved than the other, the jaw will laterally deviate to the same side during opening. Currently, clinical examination is the gold standard for diagnosing TMDs. Given the multifactorial causes of TMD, a comprehensive examination of the entire upper quadrant, including the cervical spine and shoulders, usually is warranted. In general, the TMJ and the upper three cervical joints all refer symptoms to the head, whereas the mid-to-low cervical spine typically refers symptoms to the shoulder and the arm.61–63 An accurate diagnosis of TMD involves a careful evaluation of the information gleaned from the history, systems review, and tests and measures. In most chronic cases, a behavioral or psychological examination is required.3,31,63–68 Since postural dysfunctions are closely related to TMJ symptoms, the clinician should always perform a postural examination as part of a comprehensive examination of this joint. An examination form for the TMJ examination is shown in Table 26-4. TABLE 26-4 Temporomandibular Examination Form A comprehensive history will help identify the possible source(s) of the orofacial pain and provide a screen for other causative or contributing factors.69 During the history, the clinician should observe whether the patient’s mouth moves comfortably. The severity of the symptoms and the time before the symptoms subside can provide the clinician with valuable information regarding possible pathology. Red flags related to cardiac history (e.g., angina or history of myocardial infarction) and brain function (e.g., sudden-onset severe headaches, weakness, or slurred speech) must be investigated early in the history taking.70 The clinician should determine from the patient the main reason for the visit. There are three cardinal features of TMDs, which can be local or remote: TABLE 26-5 Patient Reports of Pain in TMJ Disorders Test and Measure Test Procedure Population Reliability Kappa Values Visual analog scale 100-mm line with the end defined as no pain and worst pain imaginable 38 consecutive patients referred with TMJ disorders κ = 0.38 Numeric scale 10-point scale with 0 indicating no paint and 10 representing worst pain κ = 0.36 Behavior rating scale Six-point scale ranging from minor discomfort to very strong discomfort κ = 0.68 Verbal scale Five-point scale ranging from no pain to very severe pain κ = 0.44 Data from Magnusson T, List T, Helkimo M. Self-assessment of pain and discomfort in patients with temporomandibular disorders: a comparison of five different scales with respect to their precision and sensitivity as well as their capacity to register memory of pain and discomfort. J Oral Rehabil. 1995;22:549–556.; Cleland J. Temporomandibular Joint, Orthopaedic Clinical Examination: An Evidence-Based Approach for Physical Therapists. Carlstadt, NJ. Icon Learning Systems, LLC; 2005:39–89. With permission from Icon Learning Systems. In addition, it is important to determine: TABLE 26-6 Checklist of Psychological and Behavioral Factors Inconsistent, inappropriate, or vague reports of pain Overdramatization of symptoms Symptoms that vary with life events Significant pain of >6 months’ duration Repeated failures with conventional therapies Inconsistent response to medications History of other stress-related disorders Major life events (e.g., new job, marriage, divorce, and death) Evidence of drug abuse Clinically significant anxiety or depression Evidence of secondary gain Note: The significance of these factors depends on the particular patient. Data from McNeill C, Mohl ND, Rugh JD, et al. Temporomandibular disorders: Diagnosis, management, education, and research. J Am Dent Assoc. 1990;120:253–260. Pain or dysfunction in the orofacial region often results from nonmusculoskeletal causes such as otolaryngologic, neurologic, vascular, neoplastic, psychogenic, and infectious diseases. Clinicians often see patients with a TMD who present with nonspecific symptoms such as neck pain, headaches (see Chapter 5), earaches, tinnitus, and sinusitis.70 Patients with sinusitis complain of acute facial pain or pressure type headaches, and may present with nasal congestion, a reduced sense of smell, postnasal drip, fever or malaise, and aching teeth associated with certain weather conditions or times of the year.80 Ear disorders, such as an inner or outer ear infection, can produce pre-auricular symptoms in around the TMJ.81 Conversely, hyperactivity of the masticatory and tensor tympani muscles can cause ear pain, tinnitus, and feelings of fullness in the ear.82 Finally, patients with eye disorders may experience pain around the eye, numbness, a headache, and other symptoms similar to TMD, a cervicogenic headache (see Chapter 23), or a primary headache (see Chapter 5).70 Unexplained weight loss, ataxia, weakness, fever with pain, nystagmus, and neurologic deficits are characteristic of intracranial disorders.83 Neurovascular disorders are associated with a migraine headache and its variants, carotidynia, and cluster headaches (see Chapter 5). Neuropathic disorders include trigeminal neuralgia, glossopharyngeal neuralgia, and occipital neuralgia. A cranial nerve screen (see Chapter 3) should be completed on each patient presenting with orofacial pain with particular attention on the fifth cranial nerve (trigeminal), which supplies motor and sensory innervation to the masticatory region. Once the possibility of cervical, systemic, psychogenic, or ear or sinus problems has been ruled out, the next step is to consider the possibility of TMJ pain and impairment. Examination of the TMJ structures includes observation, and a thorough mobility and palpation examination to identify impairments and functional limitations. The posture of the head and neck are assessed for asymmetry. The forward head posture (FHP–see Chapters 6 and 25) frequently is associated with TMD.34,84,85 This is likely because of the direct impact an FHP can have on oral symmetry during occlusion. Occlusion occurs when the teeth are in contact and the mouth is closed—when tapping the teeth together in the neutral position, all of the teeth appear to strike simultaneously. However, if the same task is attempted while placing the head forward, it is the anterior teeth that occlude first. A deviation from normal occlusion is defined as malocclusion—improper positioning of the teeth and jaws. Malocclusion is a variation of normal growth and development which can affect the bite, the ability to clean teeth properly, gum tissue health, jaw growth, speech development, and appearance. The consequences of this repetitive functional malocclusion during food or gum chewing should be apparent. A chronic FHP may result in an adaptive shortening of the deep cervical fascia and muscles, which can exaggerate the functional malocclusion. Most people have some degree of malocclusion, although it is not usually serious enough to require treatment. Malocclusions can be divided mainly into three types, depending on the sagittal relations of teeth and jaws, by Angle’s classification method, which is based on the relative position of the first maxillary molar86: The clinician should also note whether the teeth are normally aligned or whether there is any crossbite, underbite, or overbite.
CHAPTER 26
The Temporomandibular Joint
OVERVIEW
 the mandible;
the mandible;
 the rudiments of the inner ear bones, the malleus, and incus;
the rudiments of the inner ear bones, the malleus, and incus;
 the anterior malleolar and sphenomandibular ligaments of the TMJ;
the anterior malleolar and sphenomandibular ligaments of the TMJ;
 the tensor tympani and the tensor veli palatini of the inner ear;
the tensor tympani and the tensor veli palatini of the inner ear;
 the mylohyoid and the anterior belly of the digastric muscle; and
the mylohyoid and the anterior belly of the digastric muscle; and
 the trigeminal mandibular nerve.
the trigeminal mandibular nerve.
 the superior component of the hyoid bone and the lesser cornu bone;
the superior component of the hyoid bone and the lesser cornu bone;
 the stapes muscle;
the stapes muscle;
 the temporal styloid process;
the temporal styloid process;
 the stylohyoid ligament;
the stylohyoid ligament;
 the stapedius muscle;
the stapedius muscle;
 the stylohyoid muscle;
the stylohyoid muscle;
 the posterior belly of the digastric muscle;
the posterior belly of the digastric muscle;
 the muscles of facial expression and mastication;
the muscles of facial expression and mastication;
 the platysma muscle; and
the platysma muscle; and
 the glossopharyngeal nerve.
the glossopharyngeal nerve.
 Predisposing factors include the structural, neurologic, hormonal, and metabolic features of an individual.
Predisposing factors include the structural, neurologic, hormonal, and metabolic features of an individual.
 Precipitating factors generally fall into the following four categories: (1) overt, extrinsic trauma to the head, the neck, or the jaw; (2) repeated low-grade extrinsic trauma, such as nail biting and chewing gum; (3) repeated low-grade intrinsic trauma such as teeth clenching or bruxism (grinding teeth); and (4) stress that passes a certain threshold, which is individual for each patient.
Precipitating factors generally fall into the following four categories: (1) overt, extrinsic trauma to the head, the neck, or the jaw; (2) repeated low-grade extrinsic trauma, such as nail biting and chewing gum; (3) repeated low-grade intrinsic trauma such as teeth clenching or bruxism (grinding teeth); and (4) stress that passes a certain threshold, which is individual for each patient.
 Perpetuating or contributing factors are those that aid in the continuation of symptoms. These can include systemic disease and cervical pathology.
Perpetuating or contributing factors are those that aid in the continuation of symptoms. These can include systemic disease and cervical pathology.
 Jaw muscles
Jaw muscles
 Bone and cartilage joint structures
Bone and cartilage joint structures
 Facial structures
Facial structures
 Soft-tissue joint structures, including the articular disk and synovium
Soft-tissue joint structures, including the articular disk and synovium
 Jaw and joint function
Jaw and joint function
 Cervical and upper thoracic spine function
Cervical and upper thoracic spine function
 Posture and dysfunction
Posture and dysfunction
 Systemic disease
Systemic disease
 Psychosocial issues
Psychosocial issues
 rheumatoid arthritis with synovitis, arthralgia, condylar degenerative disease, and open bite deformity;
rheumatoid arthritis with synovitis, arthralgia, condylar degenerative disease, and open bite deformity;
 chronic pain with a behavioral disorder;
chronic pain with a behavioral disorder;
 myofascial pain and impairment; and
myofascial pain and impairment; and
 internal disk derangement, with displacement and reduction.
internal disk derangement, with displacement and reduction.
ANATOMY
Bony Anatomy
Maxilla
Sphenoid Bone
Hyoid Bone
Mandible
Temporal Bone
Fibrocartilaginous Disk
 Medial and lateral collateral diskal ligaments firmly attach the fibrocartilaginous disk to the medial and lateral poles of the condyle, permitting anterior and posterior rotation of the disk on the condyle during mouth opening and closing.29,30
Medial and lateral collateral diskal ligaments firmly attach the fibrocartilaginous disk to the medial and lateral poles of the condyle, permitting anterior and posterior rotation of the disk on the condyle during mouth opening and closing.29,30
 Posteriorly, the disk is attached by fibroelastic tissue to the posterior mandibular fossa and the back of the mandibular condyle.29,30
Posteriorly, the disk is attached by fibroelastic tissue to the posterior mandibular fossa and the back of the mandibular condyle.29,30
 Anteriorly, the disk is attached to the upper part of the tendon of the lateral pterygoid muscle (Fig. 26-3).29,30
Anteriorly, the disk is attached to the upper part of the tendon of the lateral pterygoid muscle (Fig. 26-3).29,30
 Lower compartment. This compartment, bordered by the mandibular condyle and the inferior surface of the articular disk, is where, under normal conditions, the osteokinematic spin (rotation) of the condyle occurs.8
Lower compartment. This compartment, bordered by the mandibular condyle and the inferior surface of the articular disk, is where, under normal conditions, the osteokinematic spin (rotation) of the condyle occurs.8
 Upper compartment. This compartment, bordered by the mandibular fossa and the superior surface of the articular disk, primarily allows only translation of the disk and condyle along the fossa, and onto the articular eminence.8
Upper compartment. This compartment, bordered by the mandibular fossa and the superior surface of the articular disk, primarily allows only translation of the disk and condyle along the fossa, and onto the articular eminence.8
Supporting Structures
Muscles
Temporalis
The Masseter
The Medial Pterygoid
The Lateral Pterygoid
Infrahyoid or “Strap” Muscles
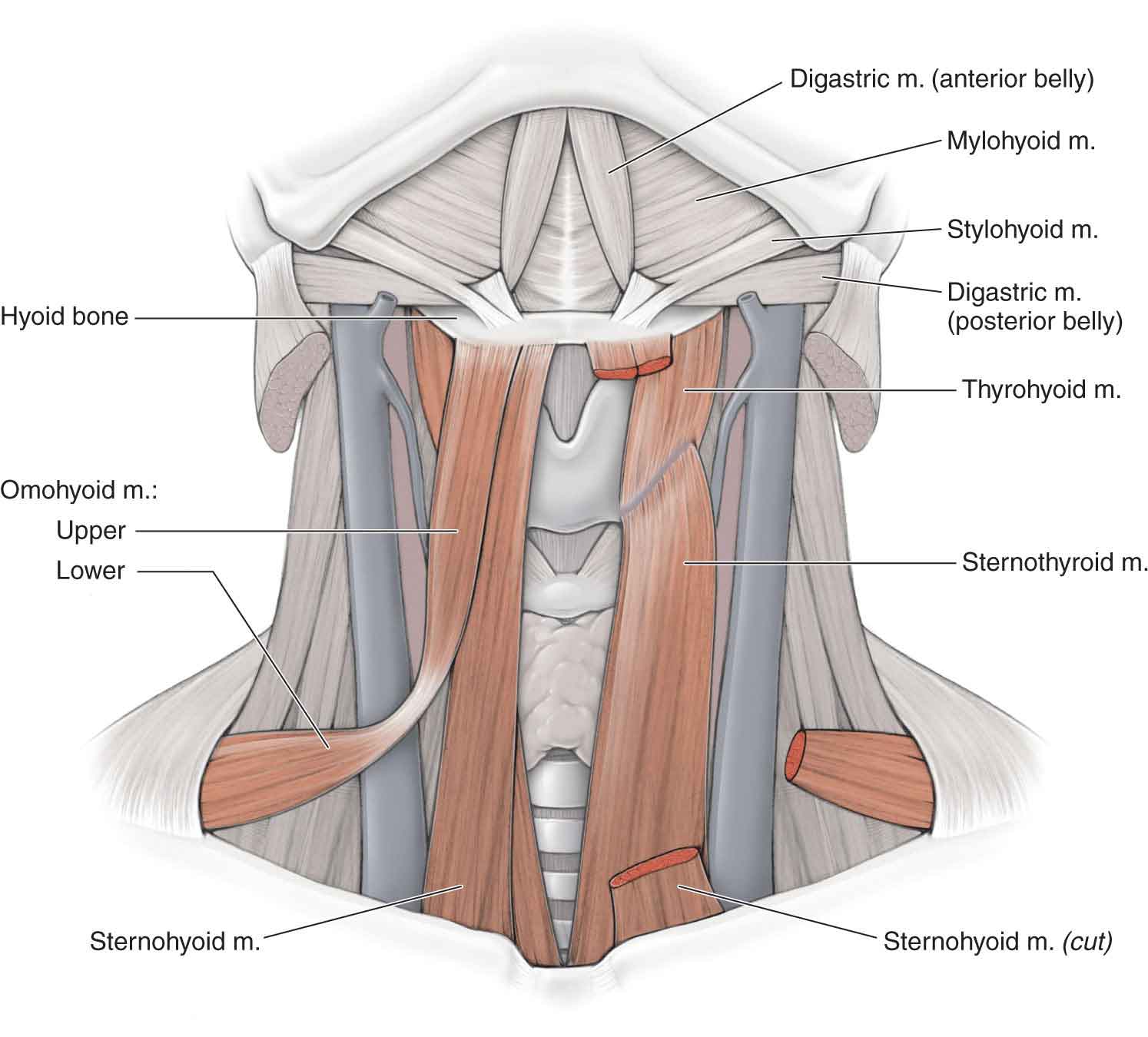
Sternohyoid
Omohyoid
Sternothyroid and Thyrohyoid
Suprahyoid Muscles
Geniohyoid
Digastric
Mylohyoid
Stylohyoid
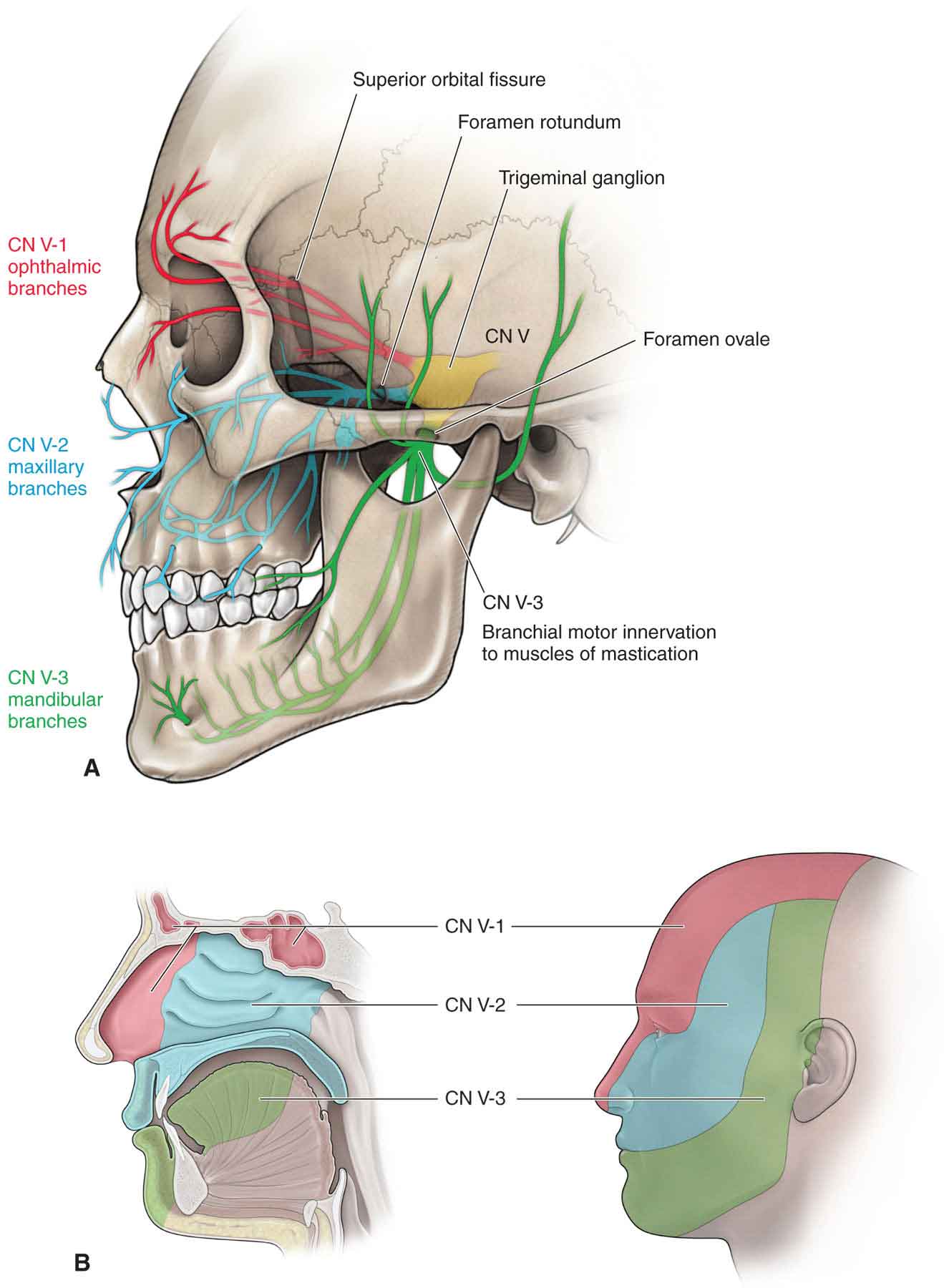
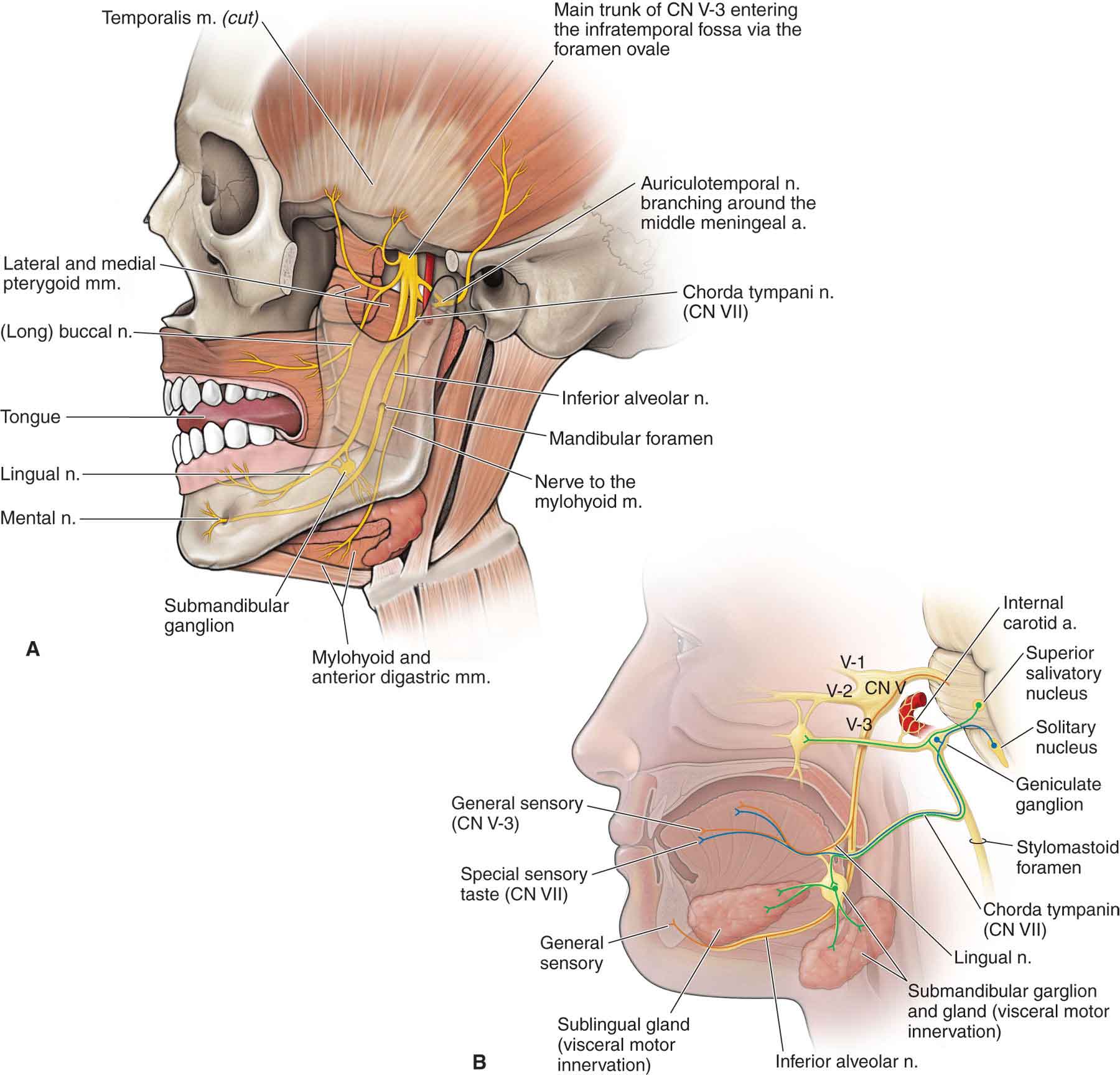
Nerve Supply
BIOMECHANICS
 mouth opening, contralateral deviation, and protrusion all involve an anterior osteokinematic rotation of the mandible and an anterior, inferior, and lateral glide of the mandibular head and disk;
mouth opening, contralateral deviation, and protrusion all involve an anterior osteokinematic rotation of the mandible and an anterior, inferior, and lateral glide of the mandibular head and disk;
 mouth closing, ipsilateral deviation, and retrusion all involve a posterior osteokinematic rotation of the mandible and an anterior, inferior, and lateral glide of the mandibular head and disk.
mouth closing, ipsilateral deviation, and retrusion all involve a posterior osteokinematic rotation of the mandible and an anterior, inferior, and lateral glide of the mandibular head and disk.
Occlusal Position
 The median occlusal position corresponds to the position in which all of the teeth are fully interdigitated19 and is considered the start position for all mandibular motions. The median occlusal position is dependent on the presence, shape, and position of the teeth. Protrusion of the upper or lower incisors, failure of the upper incisors to overlap with the lower incisors, absent or abnormally shaped teeth, and back teeth that do not meet are all causes of malocclusion.
The median occlusal position corresponds to the position in which all of the teeth are fully interdigitated19 and is considered the start position for all mandibular motions. The median occlusal position is dependent on the presence, shape, and position of the teeth. Protrusion of the upper or lower incisors, failure of the upper incisors to overlap with the lower incisors, absent or abnormally shaped teeth, and back teeth that do not meet are all causes of malocclusion.
 The centric position is considered to be the position that implies the most retruded, unstrained position of the mandible from which lateral movements are possible, and the components of the oral apparatus are the most balanced.53 Ideally, the centric position should coincide with the median occlusal position.53 It is worth remembering that malocclusion is probably very common in the general nonsymptomatic patient and may or may not be relevant to the presenting symptoms.54 Rather than being a primary etiologic factor in TMD, malocclusion is likely to have a secondary or contributory role.17,55
The centric position is considered to be the position that implies the most retruded, unstrained position of the mandible from which lateral movements are possible, and the components of the oral apparatus are the most balanced.53 Ideally, the centric position should coincide with the median occlusal position.53 It is worth remembering that malocclusion is probably very common in the general nonsymptomatic patient and may or may not be relevant to the presenting symptoms.54 Rather than being a primary etiologic factor in TMD, malocclusion is likely to have a secondary or contributory role.17,55
Mouth Opening
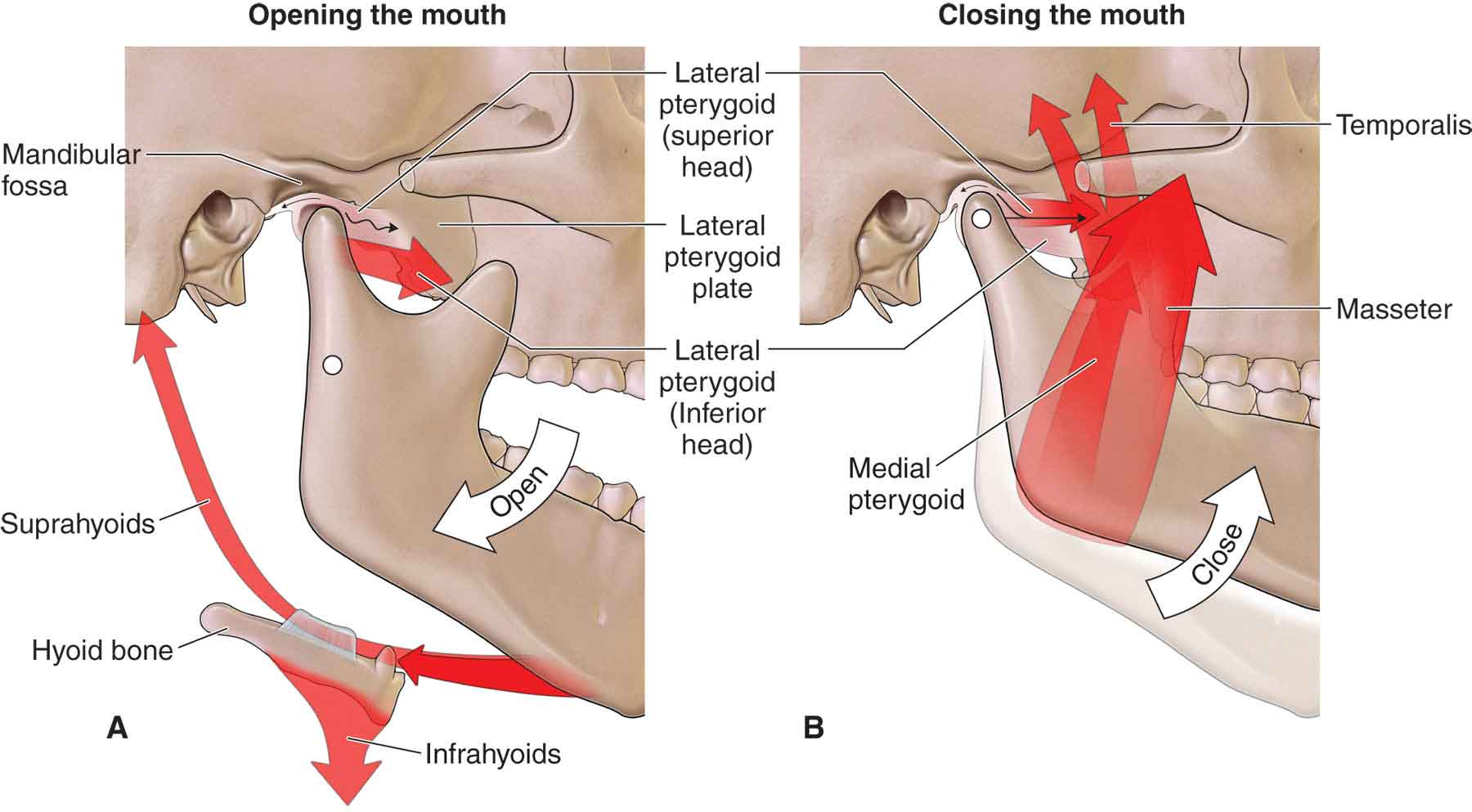
Mouth Closing
Protrusion
Retrusion
Lateral Excursion
The Close- and Open-Packed (Resting) Positions
 Anterior close-packed position. This position is the position of maximum opening of the joint.
Anterior close-packed position. This position is the position of maximum opening of the joint.
 Posterior close-packed position. This position is the maximum retruded position of the joint.
Posterior close-packed position. This position is the maximum retruded position of the joint.
Capsular Pattern
EXAMINATION

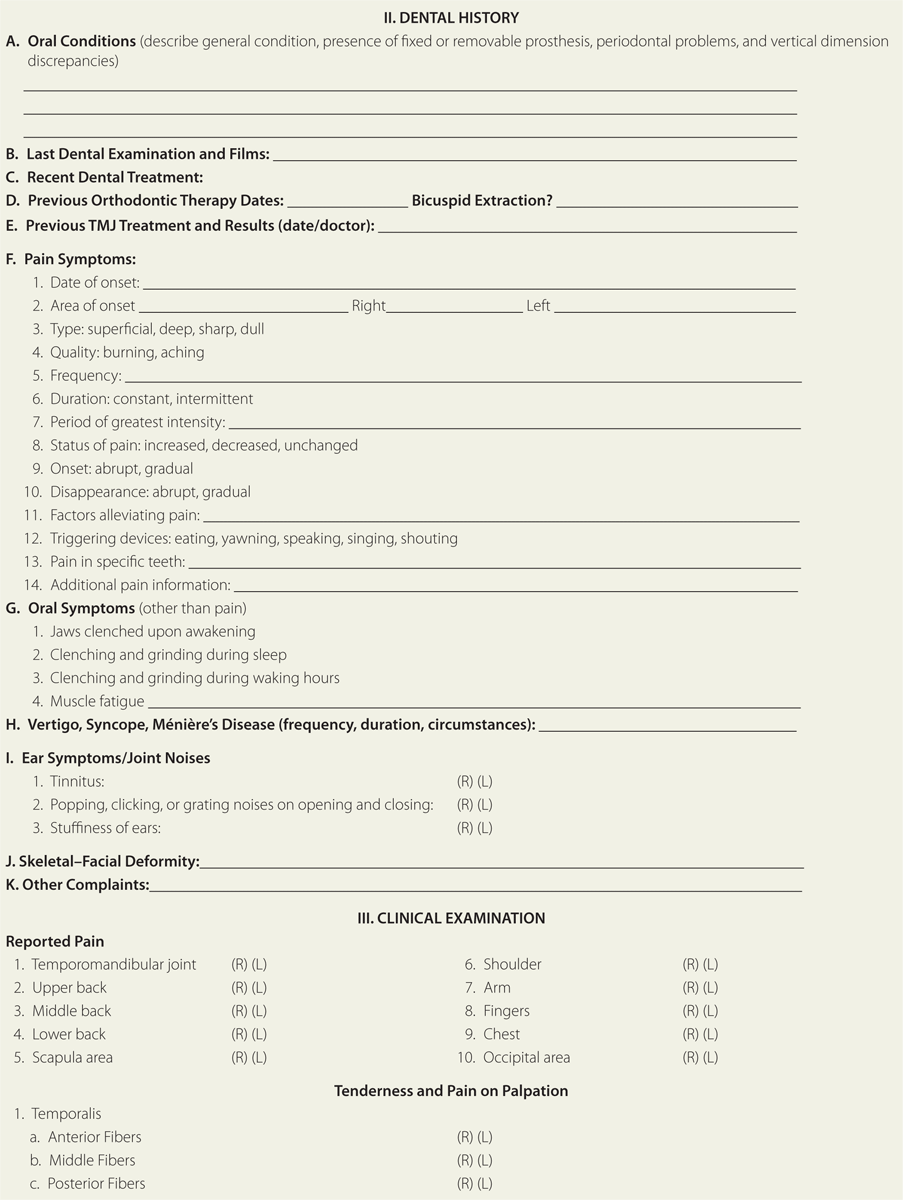
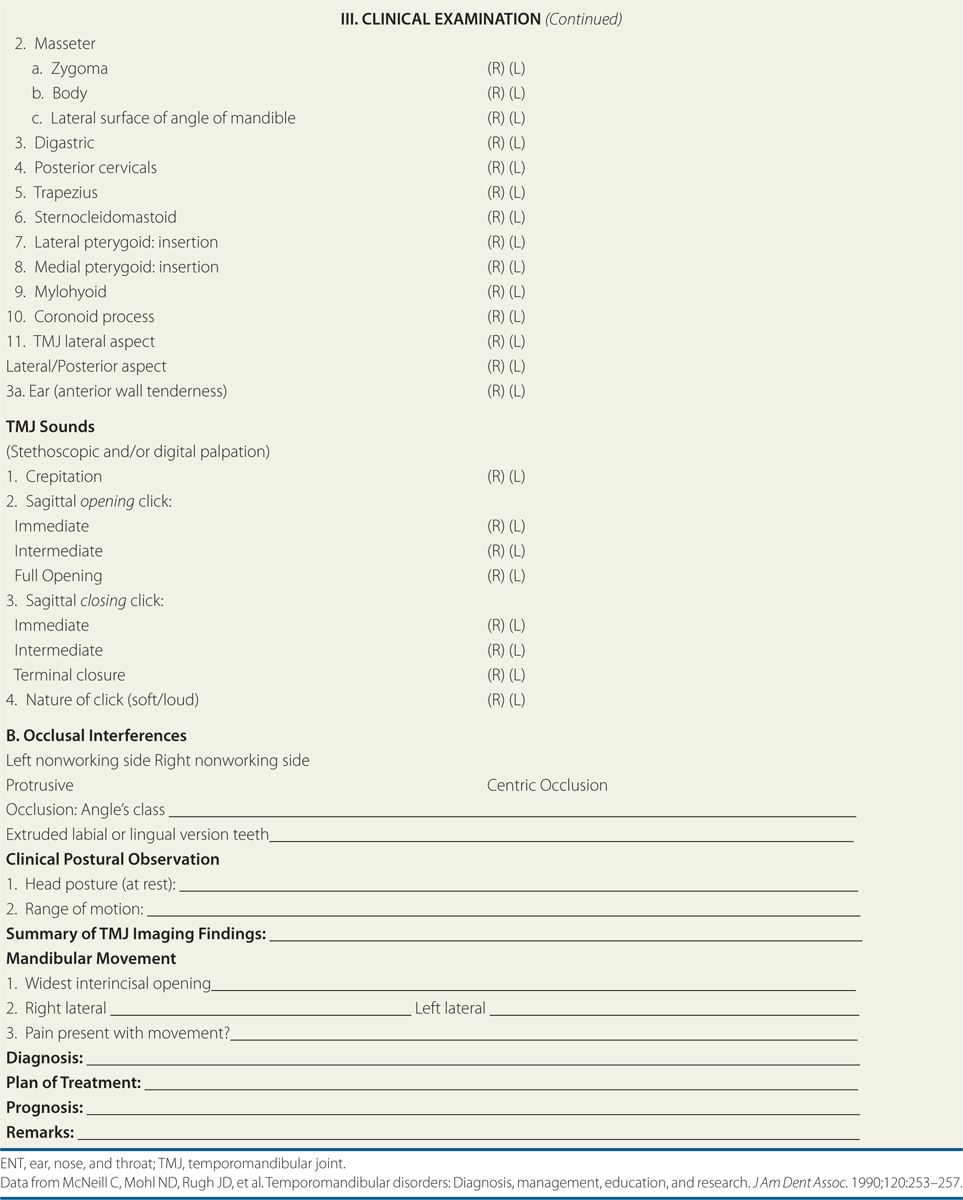
History
 Restricted jaw function. Limited mouth opening, which may be reported as intermittent or progressive, is a key feature of TMD. A key question to determine restricted jaw function is, “Have you ever had your jaw lock or catch so that it would not open all the way? If so, was this limitation in jaw opening severe enough to interfere with your ability to eat? Have you ever noticed clicking, or popping or other sounds in your joint?”71 Patients may describe a generalized tight feeling, which may indicate a muscular disorder, or capsulitis, or the sensation that the jaw suddenly “catches” or “locks,” which usually is related to a mechanical interference within the joint (an internal derangement).16 Associated signs of an internal derangement include pain and deviation of mandibular movements during opening and closing (refer to Practice Pattern 4D, under “Intervention Strategies” section later), and biting firm objects. Pain in the fully open position is probably caused by an extra-articular problem. Locking may imply that the mouth does not fully open or does not fully close and is often related to problems of the disk or joint degeneration. A gradual onset of symptoms after minor or prolonged physical activity may be indicative of a mechanical derangement. Symptoms of a mechanical nature generally are eased with rest. The irritability of a disorder is determined by the degree of activity necessary to provoke a symptom response.
Restricted jaw function. Limited mouth opening, which may be reported as intermittent or progressive, is a key feature of TMD. A key question to determine restricted jaw function is, “Have you ever had your jaw lock or catch so that it would not open all the way? If so, was this limitation in jaw opening severe enough to interfere with your ability to eat? Have you ever noticed clicking, or popping or other sounds in your joint?”71 Patients may describe a generalized tight feeling, which may indicate a muscular disorder, or capsulitis, or the sensation that the jaw suddenly “catches” or “locks,” which usually is related to a mechanical interference within the joint (an internal derangement).16 Associated signs of an internal derangement include pain and deviation of mandibular movements during opening and closing (refer to Practice Pattern 4D, under “Intervention Strategies” section later), and biting firm objects. Pain in the fully open position is probably caused by an extra-articular problem. Locking may imply that the mouth does not fully open or does not fully close and is often related to problems of the disk or joint degeneration. A gradual onset of symptoms after minor or prolonged physical activity may be indicative of a mechanical derangement. Symptoms of a mechanical nature generally are eased with rest. The irritability of a disorder is determined by the degree of activity necessary to provoke a symptom response.
 Joint noises. Joint noises (crepitus) of the TMJ may or may not be significant, because joint sounds occur in approximately 50% of healthy populations.72 Some joint sounds are not audible to the clinician, so a stethoscope may be required. “Hard” crepitus is a diffuse sustained noise that occurs during a significant portion of the opening or closing cycle, or both and is an evidence of a change in osseous contour.57 Clicking describes a brief noise that occurs at some point during opening, closing, or both [see the discussion of range of motion (ROM) testing, later]. Jaw clicking during mouth opening or closing may be suggestive of an internal derangement consisting of an anterior disk displacement with reduction.73,74
Joint noises. Joint noises (crepitus) of the TMJ may or may not be significant, because joint sounds occur in approximately 50% of healthy populations.72 Some joint sounds are not audible to the clinician, so a stethoscope may be required. “Hard” crepitus is a diffuse sustained noise that occurs during a significant portion of the opening or closing cycle, or both and is an evidence of a change in osseous contour.57 Clicking describes a brief noise that occurs at some point during opening, closing, or both [see the discussion of range of motion (ROM) testing, later]. Jaw clicking during mouth opening or closing may be suggestive of an internal derangement consisting of an anterior disk displacement with reduction.73,74
 Orofacial pain. TMJ pain should be evaluated carefully in terms of its onset, nature, intensity, site, duration, aggravating and relieving factors, and how it relates to joint noise and restricted mandibular movements. Information about the nature of the pain will be critical in determining the possibility of primary headaches (migraine, cluster) and secondary headaches related to the eyes, ears, sinus, dental structures, medication complications, and/or neurologic types of pain. Unrelenting pain unrelated to musculoskeltal function is an indication for referral. Key questions have been examined and determined to have strong sensitivity and specificity in incriminating TMDs as the source of pain.76 The initiating question should be, “Have you had pain or stiffness in the face, jaw, temple, in front of the ear, or in the ear in the past month?”70 A positive response should be followed by a question about whether the symptoms are altered by any of the following jaw activities: chewing, talking, singing, yawning, kissing, moving the jaw.69 Specific questions about activities and postures of a sustained nature, such as sitting, sleeping, and driving, should be asked. Orofacial pain associated with mouth opening or closing and jaw crepitus is suggestive of osteoarthrosis, capsulitis, or internal derangement consisting of an anterior disk displacement with reduction.73,74 Information about cervical dysfunction is essential to determine whether the cervical spine is causing or exacerbating the headache/facial pain.70 In a study by Magnusson et al.,77 five different scales of self-assessment of pain were tested in patients with TMJ disorders. The precision and sensitivity and the capacity to register memory of pain and discomfort were compared for each of the five scales (Table 26-5). From these results, the behavior rating scale can be recommended when measuring pain and discomfort in patients with TMJ disorders.
Orofacial pain. TMJ pain should be evaluated carefully in terms of its onset, nature, intensity, site, duration, aggravating and relieving factors, and how it relates to joint noise and restricted mandibular movements. Information about the nature of the pain will be critical in determining the possibility of primary headaches (migraine, cluster) and secondary headaches related to the eyes, ears, sinus, dental structures, medication complications, and/or neurologic types of pain. Unrelenting pain unrelated to musculoskeltal function is an indication for referral. Key questions have been examined and determined to have strong sensitivity and specificity in incriminating TMDs as the source of pain.76 The initiating question should be, “Have you had pain or stiffness in the face, jaw, temple, in front of the ear, or in the ear in the past month?”70 A positive response should be followed by a question about whether the symptoms are altered by any of the following jaw activities: chewing, talking, singing, yawning, kissing, moving the jaw.69 Specific questions about activities and postures of a sustained nature, such as sitting, sleeping, and driving, should be asked. Orofacial pain associated with mouth opening or closing and jaw crepitus is suggestive of osteoarthrosis, capsulitis, or internal derangement consisting of an anterior disk displacement with reduction.73,74 Information about cervical dysfunction is essential to determine whether the cervical spine is causing or exacerbating the headache/facial pain.70 In a study by Magnusson et al.,77 five different scales of self-assessment of pain were tested in patients with TMJ disorders. The precision and sensitivity and the capacity to register memory of pain and discomfort were compared for each of the five scales (Table 26-5). From these results, the behavior rating scale can be recommended when measuring pain and discomfort in patients with TMJ disorders.
 If the presenting symptoms were caused by trauma or surgery, or if the onset of pain occurred gradually. Questions should focus on any history of trauma during birth or childhood, as well as more recently.
If the presenting symptoms were caused by trauma or surgery, or if the onset of pain occurred gradually. Questions should focus on any history of trauma during birth or childhood, as well as more recently.
 If there are any emotional factors in the patient’s background that may provoke habitual protrusion or muscular tension. Chronic head, neck, and back pain often are associated with psychogenic causes. Psychiatric disorders, usually, are manifested in patients whose afflictions seem to be excessive or persist beyond what would be normal for that condition. The clinician should listen for reports of psychological stress overload, malaise, anxiety, sleep problems, changes in eating patents, weight changes, unexplained fatigue, and other signs of depression, which might exacerbate pain through central mechanisms.79 The checklist outlined in Table 26-6 can be used by the clinician to identify factors that may warrant an examination by a mental health professional.
If there are any emotional factors in the patient’s background that may provoke habitual protrusion or muscular tension. Chronic head, neck, and back pain often are associated with psychogenic causes. Psychiatric disorders, usually, are manifested in patients whose afflictions seem to be excessive or persist beyond what would be normal for that condition. The clinician should listen for reports of psychological stress overload, malaise, anxiety, sleep problems, changes in eating patents, weight changes, unexplained fatigue, and other signs of depression, which might exacerbate pain through central mechanisms.79 The checklist outlined in Table 26-6 can be used by the clinician to identify factors that may warrant an examination by a mental health professional.
 If the patient is aware of any parafunctional habits (cheek biting, nail biting, pencil chewing, teeth clenching, or bruxism). For example, does the patient chew on one side more than the other? Chewing more on one side versus the other is typically the result of malocclusion (see later). In addition, favoring one side can lead to a loss of vertical dimension (the distance between any two arbitrary points on the face). A simple way to measure the aforementioned is to measure from the lateral edge of the eye to the corner of the mouth and from the base of the nose to the chin.
If the patient is aware of any parafunctional habits (cheek biting, nail biting, pencil chewing, teeth clenching, or bruxism). For example, does the patient chew on one side more than the other? Chewing more on one side versus the other is typically the result of malocclusion (see later). In addition, favoring one side can lead to a loss of vertical dimension (the distance between any two arbitrary points on the face). A simple way to measure the aforementioned is to measure from the lateral edge of the eye to the corner of the mouth and from the base of the nose to the chin.
 The behavior of symptoms over a 24-hour period. This information assists the clinician in formulating causal relationships.
The behavior of symptoms over a 24-hour period. This information assists the clinician in formulating causal relationships.
 Whether the symptoms are improving or worsening.
Whether the symptoms are improving or worsening.
 The relationship of eating to the symptoms. Alcohol, chocolate, and other foods such as ice cream can cause head pain in some individuals, suggesting a vasomotor-related pain.
The relationship of eating to the symptoms. Alcohol, chocolate, and other foods such as ice cream can cause head pain in some individuals, suggesting a vasomotor-related pain.
 The patient’s past dental and orthodontic history.
The patient’s past dental and orthodontic history.
Systems Review
Tests and Measures
Observation
 Class I (Neutroclusion): The molar relationship of the occlusion is normal, but the other teeth have problems such as spacing, crowding, and over or under eruption.
Class I (Neutroclusion): The molar relationship of the occlusion is normal, but the other teeth have problems such as spacing, crowding, and over or under eruption.
 Class II (Distoclusion): The upper molars are placed anteriorly. There are two subtypes:
Class II (Distoclusion): The upper molars are placed anteriorly. There are two subtypes:
 Class II Division 1 (large overjet): The molar relationships are like that of Class II and the anterior teeth are protruded.
Class II Division 1 (large overjet): The molar relationships are like that of Class II and the anterior teeth are protruded.
 Class II Division 2 (deep overbite): The molar relationships are like that of class II but there is lateral flaring of the lateral maxillary incisors.
Class II Division 2 (deep overbite): The molar relationships are like that of class II but there is lateral flaring of the lateral maxillary incisors.
 Class III (Mesioclusions): The lower front teeth are more prominent than the upper front teeth. In this case, the patient very often has a large mandible or a short maxillary bone.
Class III (Mesioclusions): The lower front teeth are more prominent than the upper front teeth. In this case, the patient very often has a large mandible or a short maxillary bone.
 Crossbite: This occurs when the teeth of the mandible are lateral to the upper maxillary teeth on one side and medial on the opposite side. An anterior crossbite occurs when the lower incisors are anterior to the upper incisors, whereas a posterior crossbite occurs when there is a abnormal transverse relationship of the teeth.
Crossbite: This occurs when the teeth of the mandible are lateral to the upper maxillary teeth on one side and medial on the opposite side. An anterior crossbite occurs when the lower incisors are anterior to the upper incisors, whereas a posterior crossbite occurs when there is a abnormal transverse relationship of the teeth.
 Underbite: This occurs when the mandibular teeth are anterior to the maxillary teeth either unilaterally, bilaterally, or in pairs.
Underbite: This occurs when the mandibular teeth are anterior to the maxillary teeth either unilaterally, bilaterally, or in pairs.
 Overbite: This occurs when the anterior maxillary incisors extend below the anterior mandibular incisors when the jaw is in central occlusion.
Overbite: This occurs when the anterior maxillary incisors extend below the anterior mandibular incisors when the jaw is in central occlusion.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





