4 The shoulder
CHAPTER CONTENTS
Background
Musculoskeletal shoulder pain is a frequent presentation within physiotherapy, often with a multifactorial aetiology. It is a commonly treated problem in primary care: between seven and twenty five per 1000 adults consult general practitioners for shoulder problems (Lamberts et al 1991); and one in every three people experience shoulder pain at some stage of their lives. Of these, 54% of sufferers report ongoing symptoms at 3 years (Lewis & Tennent 2007). The most frequent diagnosis is that of rotator cuff disease (RCD) (van der Windt 1995); however, there is extremely poor correlation between magnetic resonance imaging, X-ray, ultrasound findings, and symptoms (Lewis & Tennent 2007). In addition, histological research does not provide strong evidence for an inflammatory tendon component associated with this condition; rather, the evidence points to the potential role of oxidative stress and the biochemical mediation of symptoms. Cytokines, vascular endothelial growth factor, interleukin-1beta (IL-1β), tumour necrosis factor alpha (TNF-α), and the neuropeptide substance P have all been cited as potential factors involved in tendon pathology and pain (Lewis & Tennent 2007). For those whose recovery is not self-limiting, slower or incomplete, a multitude of structures can contribute to the pain mechanism that will form the foundation of the treatment hypothesis.
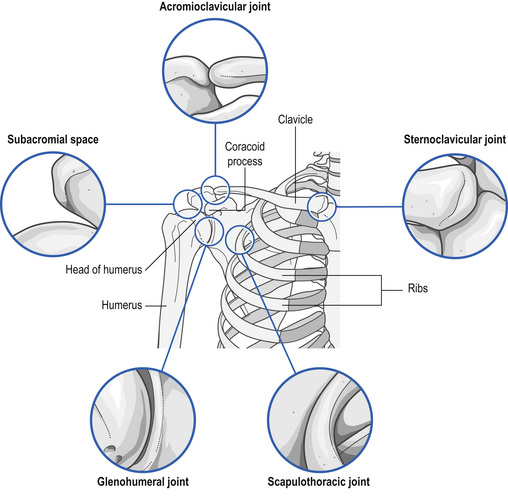
Donatelli (1997) refers to the shoulder as complex, which is composed of a number of joint structures and articulations that maintain the humerus in the joint space. Integrated and harmonious links between all structures are required for full mobility and function (Dempster 1965). The synchronized movement of four joints must occur for elevation to take place and for function to be achieved
It is necessary for the manual therapist to have a comprehensive understanding of functional biomechanics, movement phases, muscle imbalance, and injury pathology, including trauma, microtrauma, or disease processes that may interfere with any of the movement mechanisms giving rise to pain and dysfunction:
‘Acupuncture may be more or less effective for different pain types; therefore diagnosis of the predominant pain mechanisms should always underpin treatment decisions and prognosis.’ (Lundeberg & Ekholm 2001).
It is essential that relevant pain presentation mechanisms are addressed with the help of manual therapy, electrotherapy, and acupuncture intervention; once pain is under control, functional rehabilitation is facilitated (Lewis 2007). We cannot expect patients to enter into a therapeutic alliance without understanding how and why we are trying to achieve pain modulation; similarly, we must ask whether it is correct to treat the pain presentation if we do not understand the mechanisms ourselves. Assessment of these mechanisms is crucial for the development of the hypothesis that will dictate whether the manual or acupuncture intervention is to be effective (Lundeberg & Ekholm 2001).
Consider some of the structures involved in shoulder dysfunction:
The shoulder is an inherently mobile complex, with varying joint surfaces allowing the freedom of movement, and vast mobility occurs at the expense of stability (Donatelli 1997). Because there are over 20 muscles acting upon the joint to provide stability, the possibility of pain provoked from myofascial structures should never be overlooked. Indeed, it is recommended that this may well be the first line of investigation since restoration of full movement and full stability cannot occur if the muscle component is the pain-provoking structure (Ceccherelli et al 2001). Restoration of full muscle balance cannot occur with the presence of a dysfunctional motor end-plate, which prevents full muscle length. A shortened, abnormal muscle length will result in pain provoked by loading of the muscle, a characteristic presentation of myofascial pain involvement and resulting muscle weakness.
Mechanisms of myofascial pain
If any of the above is the cause, then the aim of acupuncture intervention must be:
Patients will clearly report a myofascial component to their pain if they describe:
Rotator cuff disease
Rotator cuff disease (RCD) represents the most common cause of modern shoulder pain and disability. Much of the clinical literature on RCD focuses on subacromial impingement and supraspinatus tendinopathy, although other patterns of lesions are also recognized. Both extrinsic and intrinsic factors to the cuff tendon are thought to be involved in the pathogenesis, leading on to a spectrum of conditions ranging from subacromial bursitis to mechanical failure of the cuff tendon itself (Barying et al 2007). Careful history and examination followed by pertinent investigation are essential to establish the correct diagnosis. The main aim of treatment is to improve symptoms and restore the function of the affected shoulder.
There is no definitive evidence for the efficacy of physical therapy interventions in the management of RCD (Al-Shenqiti & Oldham 2005). Myofascial pain syndromes are common conditions that result from active TrPts (Sola et al. 1955). Myofascial pain has two important components: motor dysfunction of the muscle, and sensory abnormality characterized by either local or referred pain (Whyte-Ferguson & Gerwin 2005). There are a number of clinical diagnostic characteristics that may be presented during assessment that can be used to confirm and/or exclude the presence of MTrPts. The reliability of TrPt identification has been the subject of much criticism (Bohr 1996), but the reliability of physical signs is essential to obtaining meaningful clinical information (Al-Shenqiti & Oldham 2005; Nice et al 1992). These indicators include: spot tenderness, pain recognition, and referred pain pattern.
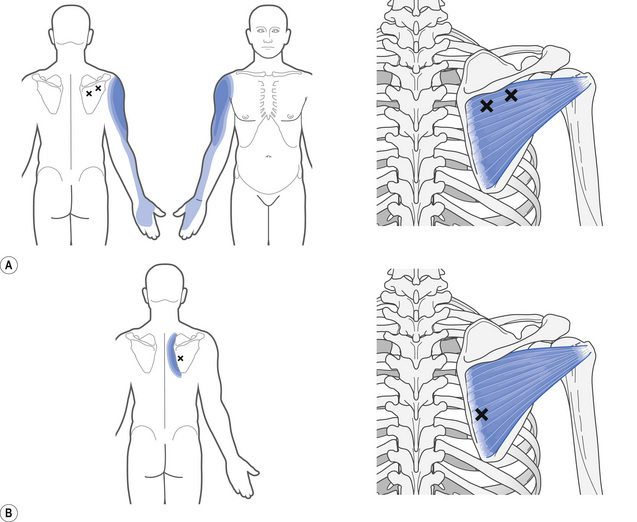
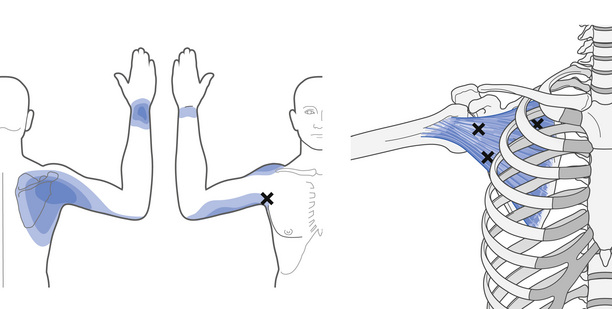
Patients demonstrating diagnostic rotator cuff tears on magnetic resonance imaging (MRI) investigation may respond favourably to the deactivation of TrPts, but it is essential to understand both the anatomical presentation of pain and the muscles commonly involved (Fig. 4.2). It is equally important to adopt rigor and standardization of assessment in order to eliminate the contributing myofascial pain component of rotor cuff pain presentation. The TrPts must be deactivated prior to shoulder stability exercise, postural and ergonomic retraining, and any future muscle imbalance and scapula retraining. The most common TrPts are found in the infraspinatus muscle, whilst the subscapularis is least affected muscle in RCD (Al Shenqiti & Oldham 2005).
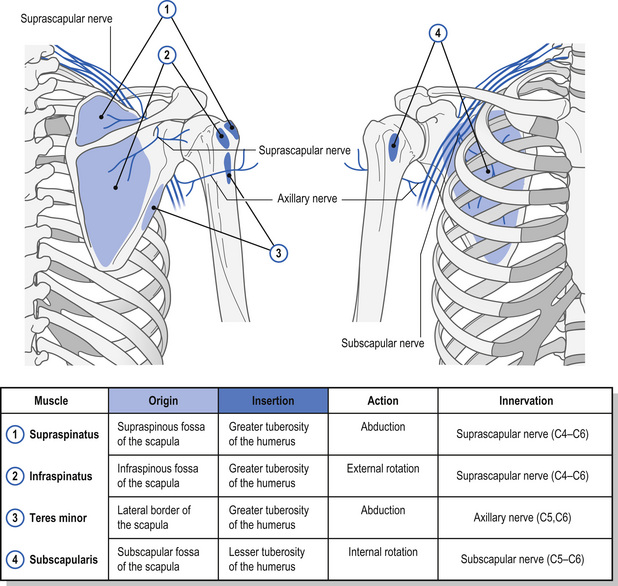
Muscles involved
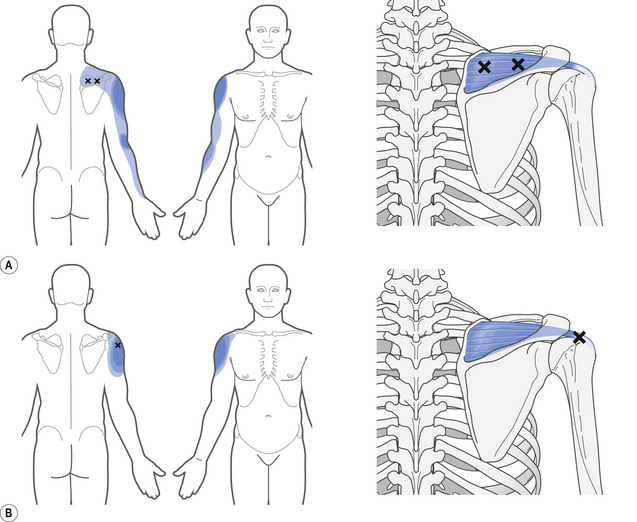
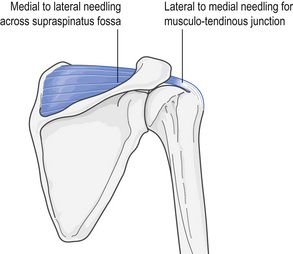
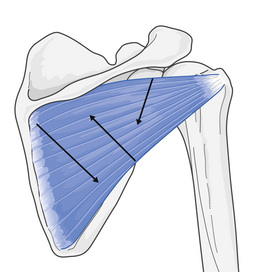
The supraspinatus muscle
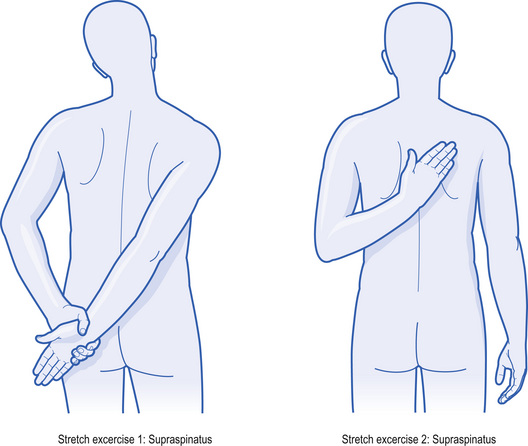
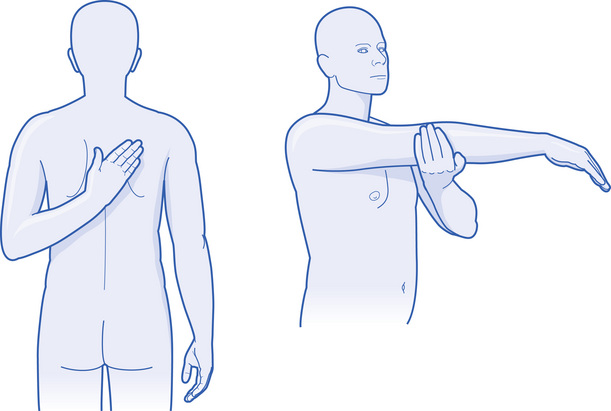
A major function of the supraspinatus (Figs. 4.3 and 4.4) is to maintain balance amongst the other rotator cuff muscles and therefore offer stability to the joint. A common clinical symptom is ‘a catch’ of severe pain whilst the movement of elevation is attempted, with a positive Neer or Hawkins sign, or both. Pain is referred to the mid-deltoid region, extending to the arm and forearm if severe, especially at the lateral epicondyle of the elbow. It may often be mistaken for subdeltoid bursitis or later epicondylitis (Simons et al 1999), but in reality, the supraspinatus muscle is in direct contact with the bursa and, hence, we are presented with nociceptive sensitization. It is necessary to undertake TrPt release and manage the patient with appropriate stretching and muscle re-education. This muscle should not be stretched if related RCD processes are present (Fig. 4.5).
The infraspinatus muscle
Infraspinatus injury is a common presentation characterized by deep, intense pain at the anterior edge of the shoulder within the bicipital groove, radiating down the radial aspect of arm and forearm, and it is identified as a major source of arm pain (Figs. 4.6 and 4.7) (Travell 1952). The pain is associated with abduction and medial rotation, and is most commonly a result of the acute overload associated with whiplash injury. If joint restriction accompanies the trigger point, then mobilization of the acromioclavicular and sternoclavicular articulations may be required. If there is suspicion of rotator cuff damage, the infraspinatus should not be stretched, but sustained myofascial contract–relax should be used (Fig. 4.8).
Isolated posterior pain is usually not involved in a single muscle pain presentation. However, if the patient complains of dysaesthesia in the fourth and fifth fingers, this may well be attributed to a single muscle element (Escobar & Ballesteros 1998). This is usually the result of overload stresses, and repetition of upward reaching and extension of the shoulder, commonly associated with window cleaning. Its action is often coupled with the infraspinatus, and it is necessary to deactivate both muscles before any muscle imbalance retraining.
The subscapularis muscle
Subscapularis trigger point pain referral presents with posterior scapula and shoulder pain in the form of a ‘watchstrap band’ of pain on the affected arm (Fig. 4.9) (Zohn 1988). The subscapularis medially rotates and adducts the arm and patients initially have pain on medial rotation and abduction; for example, when throwing a ball or playing golf. It can also manifest in patients following hemiplegia. Gradually abduction is restricted to below 45° and is often diagnosed as frozen shoulder. The subscapularis is often overlooked in shoulder dysfunction (Donatelli 1997; Simons et al 1999). It has a large and relatively inaccessible muscle mass that serves to sensitize the other rotator cuff muscles, which often develop latent TrPts. This leads to loss of rotation and pain patterns that may mimic joint range of movement loss, especially in lateral rotation. Management aims to identify the factors involved, whilst pain management remains a priority because pain leads to inhibition of rotator cuff and shoulder weakness (Donatelli 1997; Itoi et al 2007). The goals of the rehabilitation process should include:
What if inflammation is present?
Although the evidence for the presentation of inflammatory processes in RCD is poor, there are some indications that these processes are present in cases of acute injury. Acupuncture is thought to have a modulating effect on both the systemic and peripheral mechanisms implicated in neurogenic inflammation (Ceccherelli et al 2002). After stimulation with acupuncture, calcitonin gene-related peptide (CGRP), substance P, and beta-endorphin are all released (Raud & Lundeberg 1991). Substance P initiates mast cells and macrophages to secrete inflammatory mediators; CGRP stimulates vasodilatation and thus induces peripheral events, improving tissue function and pain relief. If the acupuncture is too intense and too frequent, it can result in overstimulation of substance P and CGRP, causing a proinflammatory effect. Well-performed acupuncture (obtaining de Qi) that is low dose and frequently applied (two or three times per week for 10 to 20 minutes) using points distal to the injury site, at the segmental dorsal horn or on the contralateral side (Bradnam 2002) at the start of the injury process, could provoke a sustained low-dose release of CGRP with resulting anti-inflammatory effects (Sandberg et al 2004) and without activation of proinflammatory agents (Raud & Lundeberg 1991
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree