3 Cervical spine
CHAPTER CONTENTS
Introduction
The application of the biopsychosocial and evidence-based models directs the assessment and management of cervical spine disorders. In physiotherapy, the biopsychosocial model recognizes the presence of injury, pathology, and pain, and integrates them with psychological and social issues to manage cervical spine dysfunction and pain syndromes (Jones et al 2002). Rehabilitation of the cervical spine involves pain management, physical therapies, assurance, explanation, education, self-help strategies, ergonomics, and most importantly, exercise.
Assessment
Objective assessment
The aim of manual assessment of the cervical spine is to identify the presence of any organic musculoskeletal physical impairment related to the patient’s pain. The initial focus should be on the investigation of any subjective findings, which may indicate cervical artery insufficiency, craniocervical ligament instability, or neurological lesion. Early detection of the presence of any of these factors may impose further restrictions on examination and treatment. Any potential symptoms must be monitored carefully throughout the examination.
Cervical artery insufficiency and manipulative therapy
Research investigating what was previously called vertebral artery testing now suggests that therapists should now be aware of and incorporate the entire cervical blood flow into their diagnostic triage. Currently, there is a move away from the cardinal vertebral artery signs (Thiel & Rix 2005) and functional pre-screening tests in patients who are susceptible to a spontaneous dissection event during manual or manipulative therapy (Kerry et al 2007). Clinicians should be aware that symptoms of cervical artery dissection are diverse, and not only include the classic brainstem signs and symptoms, but can also include symptoms such as unilateral head and neck pain (Sturzenegger 1994). The latest Australian Physiotherapy Association guidelines (APA 2006; Magarey et al 2004) suggest that history taking is the best indicator to use when identifying those patients who may be at risk. Key questioning around atherosclerotic risk factors and repeated or significant trauma are two areas that may help a clinician in their clinical reasoning (Mitchell 2002).
Craniocervical ligament instability testing
As with cervical artery testing, craniocervical ligament instability testing has shown to have poor sensitivity and specificity (Cattrysse et al 1997). Therefore, a comprehensive history and a decision made from a clinician’s index of suspicion should guide the management of a patient. Krakenes et al (2002) estimated a probable incidence of alar ligament injuries in 39% of patients with chronic whiplash associated disorder (WAD). A history of upper cervical pain post trauma, radiological evidence of craniocervical abnormalities, congenital craniocervical anomalies, and degenerative conditions, which may be associated with craniocervical instability, can all be indications for further investigation or testing. Symptoms of cervical artery insufficiency, cord signs, and parenthesis of the lips or tongue (compression of the hypoglossal nerve at the ventral ramus of C2) may raise the index of suspicion of craniocervical instability. The classic tests used clinically are the Sharp-Purser test (transverse ligament), the tectorial membrane flexion test, and alar ligament stress tests (Aspinall 1990).
Neurological examination
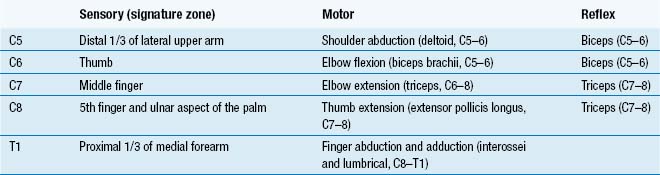
Many nerve root injuries go undiagnosed (Gifford 2001) because the nervous system often provokes vague distributions of pain as well as the classic dermatomal distributions. A good neurological examination provides key information about the structures involved, the patient’s prognosis, and the efficacy of treatment. A comprehensive history, combined with neurological and musculoskeletal examination, has been shown to provide good diagnostic accuracy in patients with cervical radiculopathy (Wainner et al 2003). Detailed neurological examinations have been described in the literature (Butler 2000). Table 3.1 outlines the sensory signature zones (Butler 2000), associated muscle tests, and muscle stretch reflex for the mid- to lower cervical spine.
Adverse neural dynamics
A neural provocation or neurodynamic test is a sequence of movements designed to assess the mechanics and physiology of that part of the nervous system by elongating the length of the nerve (Coppieters et al 2002). The following tests are useful in the clinical picture of cervical spine dysfunction:
Both the slump and upper limb neurodynamic test have shown to heighten responses in subjects with chronic WAD (Sterling et al 2002; Yeung et al 1997). Jull (2001) found that there was a 10% increase in the incidence of sensitized neuromeningeal structures using the passive neck flexion test in chronic headache sufferers.
Observation
Forward head posture has historically been linked with cervical dysfunction (Janda 1994). Currently, the literature associating forward head posture and cervical spine pain is not strong (Dalton & Coutts 1994; Griegel-Morris et al 1992; Haughie et al 1995; Johnson 1998; Treleaven et al 1994; Watson & Trott 1993). The importance of any observations must be put into context on a multifactorial basis. Deviations may be normal variations. Postural differences may reflect structural, muscle, joint, and neural system sensitivity, be reactive to pain states, or may reflect psychological factors.
Active range of movement
There is now enough research indicating that disorders of the cervical musculoskeletal system are characterized by a reduction in range of motion (ROM) (Dall’Alba et al 2001; Hall & Robinson 2004; Zwart 1997). Deficits in ROM appear not to be pathology specific; however, assessment of active ROM may give an insight about the structures affected. Distribution of pain associated with bilateral rotation, side bend, upper cervical spine flexion, lower cervical spine flexion, and extension, plus extension rotation quadrants, should be recorded. Active tests may be progressed by:
Techniques for segmental localization can also be useful; for example, rotation performed in full flexion to assess upper cervical spine rotation (C1 to C2) has been shown to be limited in the majority of cervicogenic headache sufferer (Hall & Robinson 2004). Sustained positioning can also be of benefit, especially when subtle pain originating from the nervous system is apparent. The key findings of the active movement examination should be recorded. This information should lead the practitioner in the direction for further physical examination and provide important outcome measures.
Manual assessment
Passive, manual assessment can be broken down into:
PAIVMs are short lever techniques used during assessment of the cervical spine and are also beneficial in the treatment of acute conditions or in elderly patients (Hing et al 2003). PPIVMs use combined movements to access restriction in a joint using a longer lever.
The manual examination provides basic in vivo measures of pain reproduction and the elastic properties of the viscoelastic tissues of the spinal motion segment. This information should support or reject the clinician’s hypothesis gleaned from the initial subjective and objective findings. A clinician’s ability to detect a symptomatic segment in the cervical spine has been a point of debate, which questions the basis for the manual examination. Jull et al (1988) performed the pioneering study comparing manual examination to local segmental blocks in the cervical spine. In this study, the experienced manual therapist correctly detected all 15 symptomatic segments in patients with cervical pain. However, King et al (2007) reproduced Jull et al’s study using a larger number of subjects and new local segmental blocking techniques. The results of this later study showed significantly lower levels of accuracy in the manual examination. There continues to be discussion about whether the local segmental block is an accurate diagnostic tool and about other methodological differences published in the studies. The manual examination has also been shown to have poor inter-tester and intra-tester reliability with regard to detecting stiffness (Maher & Adams 1994).
Motor and sensory assessment
There is now a significant amount of research demonstrating that there are impairments to the motor system associated with cervical spine dysfunction that do not spontaneously resolve (Falla et al 2004; Jull 2000; Tjell & Rosenhall 1998; Tjell et al 2003). This research has shown that there is impairment to the deep stability muscles of the cervical spine and shoulder girdle, and in some instances, oculomotor and global proprioceptive strategies.
Asking the patient to sit up and assume what they perceive is correct posture may be a useful way for assessing the patient’s ability to assume a normal upright position. Clinically, if there is an obvious postural dysfunction, it is useful to alter the apparent problem and assess whether it affects the patient’s symptoms. Consideration should be given to the appropriate sitting, standing, or functional positions. Special attention should be given to the interaction of the shoulder girdle and cervical spine. Loss of the feed-forward postural mechanisms associated with upper limb movement (Falla et al 2004) and low-load holding capacity of the deep cervical flexors and scapulothoracic muscles (Grant et al 1997) have been associated with chronic cervical spine dysfunction. Assessment of shoulder elevation and simple workstation tasks can be clinically useful in detecting dysfunction. The two most common postural dysfunctions affecting the upper limb and cervical spine are a downwardly rotated scapular and a protracted, elevated scapula (Janda 1994; Sahrmann 2002).
Specific analysis of the deep flexors of the cervical spine can be done by looking at a patient’s active cervical spine extension and the craniocervical flexion test (C-CFT). Active cervical spine extension tests a patient’s ability to eccentrically use the deep flexors muscles. Dysfunction is commonly seen either when a patient will not allow the head centre of rotation to pass behind the frontal plane or when they perform a compensatory strategy, therefore loading the osseoligamentous structures of the cervical spine (Jull et al 2004). The recovery from this position is also useful to show compensatory motor strategies. The C-CFT, as described by Jull et al (2004), uses a pressure biofeedback unit (Pressure Biofeedback Unit, Chattanooga Group, Hixon, USA). This tool will augment the skills of a clinician in movement and muscle analysis in order to assess the function of the deep stability muscles of the neck. The aim of the test is twofold: first, to assess the movement pattern by asking the patient to progressively move the needle up in 2 mmHg increments from 20 to 30 mmHg so as to assess the use of superficial neck muscles and the patient’s kinaesthetic sense; and secondly, to look at the holding capacity for the muscles starting at 22 mmHg for 10-second periods. This test gives key information in the implementation of a patient’s home exercise programme. The postural control system for the body receives important information from cervical spine afferents. The deep muscles of the upper cervical spine have a high number of muscle spindles, which are responsible for the complex interaction between the cervical spine, ocular motor, proprioceptive balance control, and vestibular systems. Dizziness and unsteadiness are the next most frequent complaints (after pain) in subjects with WAD (Treleaven et al 2003, 2005). Tests for balance, proprioception, and eye movement control are described elsewhere in the literature to which readers are referred (Jull et al 2004).
Diagnosis
Making a diagnosis is essential for goal setting and the clinician’s evaluation of treatment. The diagnosis should consider the tissue affected; the time frame of tissues healing, and the apparent pain mechanisms. This will guide a clinician through the appropriate clinical reasoning and evidence-based pathway for management. Assessment is an ongoing, progressive task that must accompany the treatment. Red flag conditions should be identified and referred on to the appropriate health professional immediately. Early identification of yellow flags and patients who may benefit from cognitive behavioural therapy (CBT) is essential for the effective management of this patient group. Outcomes such as visual analogue score (VAS) for pain, function, and performance can then be used to record the outcomes of treatment. The Neck Disability Index (NDI) (Vernon & Moi 1992) and the Patient-Specific Functional Scale (PSFS) (Westerway et al 1998) are two other commonly used outcome measures. Common cervical spine problems seen within a musculoskeletal clinic include:
Treatment
The aims of physiotherapy treatment are:
A multimodal treatment approach involving manual therapy and a therapeutic home exercise programme (including cervical stability and proprioceptive training) have been shown to be of benefit in the treatment of both traumatic and idiopathic cervical spine pain (Allison et al 2002; Cleland et al 2007a, b; Jull et al 2002).
Spinal manual and manipulative therapy
Although there is ongoing discussion about the safety issues associated with manipulation of the cervical spine, manual and manipulative spinal therapy (DeFabio 1999) continue to be widely used in the treatment of cervical spine dysfunction. The exact mobilization and manipulation mechanisms that provide therapeutic benefit are not known. Research indicates there is a multisystem response from the motor, sensory, and sympathetic nervous systems (Sterling et al 2000; Vernon et al 1990; Wright 1995; Wright & Vincenzino 1995). Importantly, it also appears that manual therapy may also improve the performance of the therapeutic exercise programme (Sterling 2000). Most theoretical models of manual therapy use manual assessment (active ROM, PPIVM, and PAIVM) and apparent pathological state to determine grade and direction of movement. For simple mechanical cervical spine pain, the sequence of palpation, mobilization, and manipulation of a spinal segment is logical and simple in clinical application. The most common clinical dysfunctions usually involve ipsilateral rotation and side bend dysfunctions. The graded application of palpation, mobilization, and manipulation to restore a mid-cervical spine dysfunction is shown in Fig. 3.1. The techniques are progressed as the patient’s symptoms allow and the tissue-healing model indicates. With more complex pathologies (e.g. acute traumas, nerve root irritation, segmental instabilities and arthropathies) more care is needed in the selection of manual therapy techniques and their application. Tables 3.2 and 3.3 suggest some indications, precautions, and contraindications to cervical spine mobilization and manipulation (adapted from Aspinall 1989; Bogduk 1994; Gibbons & Tehan 2000; Gross et al 1996; Kerry & Taylor 2006; McCarthy 2001; Magarey et al 2004; Maitland 2000; Mitchell 2002; Rubinstein et al 2005; Shekelle & Coulter 1997; Sran 2007).
Table 3.2 Indications, precautions, and contraindications to cervical mobilization
| Indications | |
| Precautions | |
| Contraindications |
Table 3.3 Indications, precautions and contraindications to cervical spinal manipulation