Problem
Solution
Oversizing
ap
Anterior referencing
Overstuffing of flexion gap, reduced ROM, stiffness
Downsize femoral component
1. Add more flexion to fill flexion gap
2. Recut distal femur 2 mm, and use thicker PE
ap
Posterior referencing
Overstuffing of patellofemoral joint, increased patellofemoral pressure, increased pain, decreased ROM
Downsize femoral component
1. With anterior notching <3 mm
2. Shift femoral component 2 mm anterior, recut distal femur 2 mm and use thicker PE
ml
Irritation of capsule and collateral ligaments
Downsize femoral component, additional measures as above
Undersizing
ap
Anterior referencing
Instability of flexion gap, increased wear
Use same size femoral component
1. Add more flexion to fill flexion gap
2. Recut distal femur 2 mm and use thicker PE
ap
Posterior referencing
Notching of anterior cortex, increased fracture risk if >3 mm
Use same size femoral component
1. With anterior notching <3 mm
2. Shift femoral component 2 mm anterior, recut distal femur 2 mm and use thicker PE
ml
Possible medialisation of trochlea
Place femoral component as lateral as possible
The most common problem is adequate sizing of the femoral component, as this is influenced by the underlying principles, “anterior referencing” or “posterior referencing” (Figs. 15.1, 15.2, 15.3, and 15.4), as well as “femur first” or “tibia first” [8]. Femoral size is determined by the anteroposterior dimension, as the reconstruction of the posterior condylar offset is important for reconstructing knee kinematics [9].
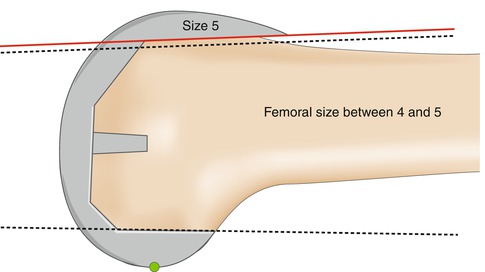
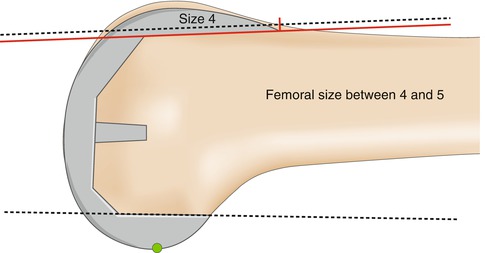
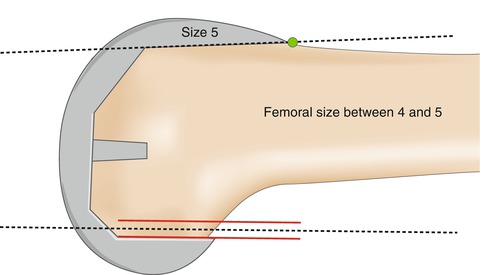
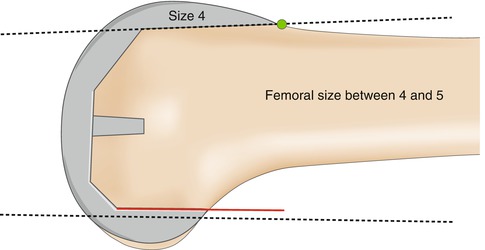
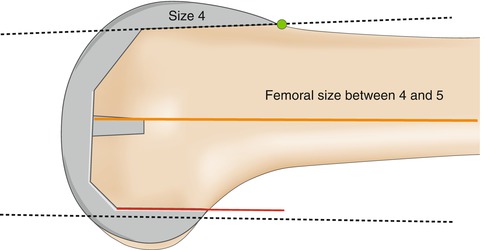
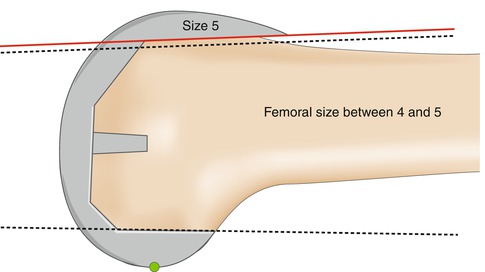
Fig. 15.1
Oversizing the femoral component in a posterior referenced system overstuffing of patellofemoral joint
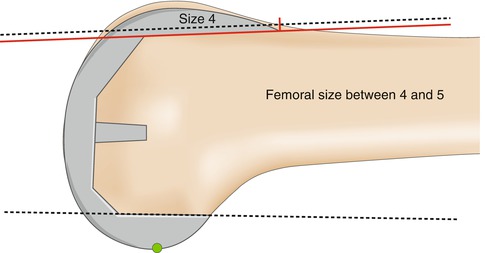
Fig. 15.2
Undersizing the femoral component in a posterior referenced system anterior notching
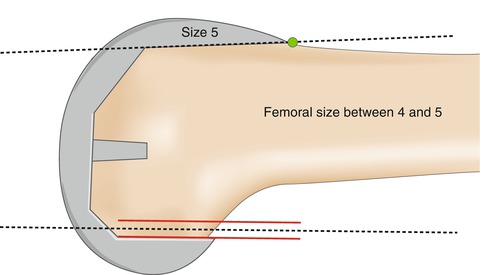
Fig. 15.3
Oversizing the femoral component in an anterior referenced system tightness of flexion gap
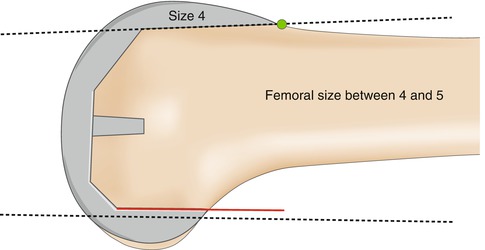
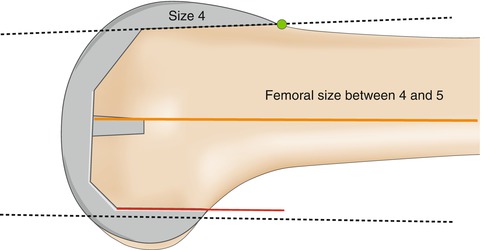
Fig. 15.4
Undersizing the femoral component in an anterior referenced system flexion gap instability
Femoral size is determined by the anteroposterior dimension, as the reconstruction of the posterior condylar offset is important for reconstructing knee kinematics.
Direct correlation has been reported between posterior condylar offset and range of motion [1]. In case of decreased posterior condylar offset, the range of flexion will decrease. If the posterior condylar offset is reduced by 2 mm, the flexion decreases in mean 12.2°.
Although inter- and intraobserver reliability of femoral sizing is very accurate [18], size measurement of the femoral component is highly dependent on the method used: “flexion space balancing”, used in most “tibia-first” instruments, leads to smaller size measurements than “size-matched resection”, used in most “femur-first” instruments [8]. Preoperative varus knees are more sensitive to these differences. In 6.7 % there is a side difference of femoral sizes in the same patient [4].
“Flexion space balancing”, used in most “tibia-first” instruments, leads to smaller size measurements than “size-matched resection”, used in most “femur-first” instruments.
A flexion or extension error of the distal femoral cut leads to the choice of an up- or downsized femoral component [17]. This fact can also be used in case downsizing is required: additional flexion of the femoral component by 2° leads to 1 mm less resection of the posterior femoral condyles [22] (Fig. 15.5).
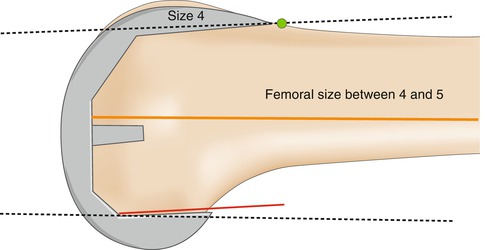
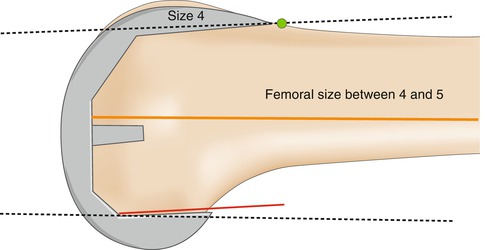
Fig. 15.5
Increased flexion of the femoral component to fill flexion gap
A mediolateral overhang of more than 3 mm irritates the capsule, the ITB or collateral ligaments and causes pain [15].
There has been broad discussion of whether mediolateral overhang can be avoided by the use of “gender” implants. In general, the ratio between the transepicondylar width and the height of the condyles is constant, but some narrow femora could require narrower implants to avoid mediolateral overhang [19]. On the other hand, despite reduced overhang by using “gender” knee implants, there are no differences in clinical outcome [6].
In the case that the chosen femoral size doesn’t cover the whole mediolateral width, a lateralisation rather than medialisation of the implant is recommended in order to improve patellar tracking (Fig. 15.6).


Fig. 15.6
Lateralisation of femoral TKR implant, if implant does not cover mediolateral width
When the chosen femoral size doesn’t cover the whole mediolateral width, a lateralisation rather than medialisation of the implant is recommended in order to improve patellar tracking.
In general, a change of size in a posterior referenced TKR system means a change of the anterior bone cut (Figs. 15.1 and 15.2).
Oversizing the femoral component in a posterior referenced system means overstuffing of the patellofemoral joint and leads to increased patellofemoral pressure and possibly pain (Fig. 15.1) [10].
Undersizing the femoral component in a posterior referenced system means notching of the anterior cortex and a possible risk of fracture (Figs. 15.2 and 15.7). Minimal anterior notching has no influence on the risk of fracture [20, 7], as long as femoral notching of more than 3 mm with sharp edges at the proximal end of the femoral prostheses is avoided [24].
Fig. 15.7
Femoral undersizing with a posterior referenced TKR system: notching of the anterior femoral cortex
Oversizing the femoral component in a posterior referenced system leads to overstuffing of the patellofemoral joint and increased patellofemoral pressure. Undersizing the femoral component in a posterior referenced system means notching of the anterior cortex and a possible risk of fracture.
In general, a change of size in an anterior referenced TKR system means a change of the posterior bone cut (Figs. 15.3 and 15.4).
Oversizing the femoral component in an anterior referenced system means overstuffing of the flexion gap and a reduced ROM [2, 12].
Undersizing the femoral component in an anterior referenced system leads to flexion instability, increased polyethylene (PE) wear and decreased flexion (Fig. 15.8) [1].










