Chapter Four The principles of combined movement assessment
We are essentially searching for the patient’s ‘predominant dysfunction or fault’ in order to direct our intervention towards it. The process of ranking the importance of our findings requires that we test the hypothesis of ‘predominant dysfunction’ throughout our interaction with our patients. In short, during the examination of patients we are considering if our hypothesis will guide treatment more effectively than the next most likely hypothesis. In addition, during treatment we should be continually considering if our chosen intervention is in fact more effective than the next most likely intervention. This process of analytical assessment is not new and was advocated by Maitland (1986) and Grieve (1988, 1991) over 30 years ago.
Subjective examination
During the initial consultation the therapist will begin to form an impression of the patient based on verbal and non-verbal communication. Expert clinicians form an impression regarding diagnosis, management and expectations of the patient very quickly. Mixed methods of clinical reasoning are utilized in this process as outlined in Chapter 3.
Is it acceptable to reproduce symptoms – are they ‘severe’?
• Is the faulty position producing severe pain?
• Is positioning in the faulty position likely to cause a latent or long-term exacerbation of symptoms?
• Is there a position that will allow examination and treatment whilst avoiding unacceptable symptom reproduction?
• Is it likely that caution needs to be taken due to a patho-anatomical reason that would make the use of combined movement theory (CMT) unwise? See the contraindications to manual therapy in the box below.
What is the predominant pain mechanism?
• Is the patient’s predominant pain mechanism: nociceptive, peripheral neurogenic, central sensitivity, autonomic or affective?
 Clinical point Contraindications to spinal passive movement that takes a joint to the end of passive range or thrust techniques
Clinical point Contraindications to spinal passive movement that takes a joint to the end of passive range or thrust techniques
Relative contraindications
(See Gibbons & Tehan, 2001a,b; Grieve, 1991.)
What is the functional demonstration of the positional fault?
Patient presentations, suggestive of the suitability of a CMT approach, have symptoms predominantly influenced by specific positions or movements. Patients can often demonstrate these movements or positions and reproduce them in the course of replicating a functional activity. For example, patients with anterior stretch patterns of the mid cervical spine often relate symptom reproduction with activities inducing ipsilateral lateral flexion and rotation, e.g. reversing the car. The monitoring of change in the functional demonstration, during examination and treatment is a crucial monitor of treatment effectiveness. Again, the concept of a functional demonstration is a long-established tenet of the Maitland concept (Maitland, 1986) and at the heart of CMT.
Physical examination
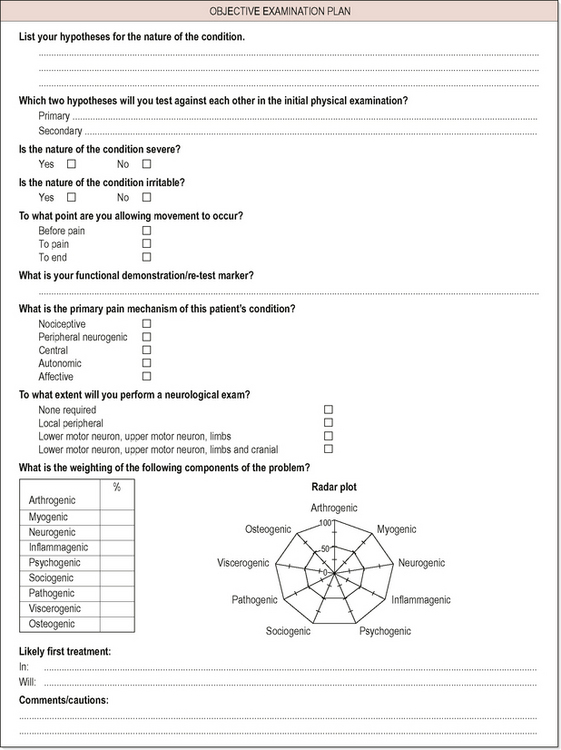
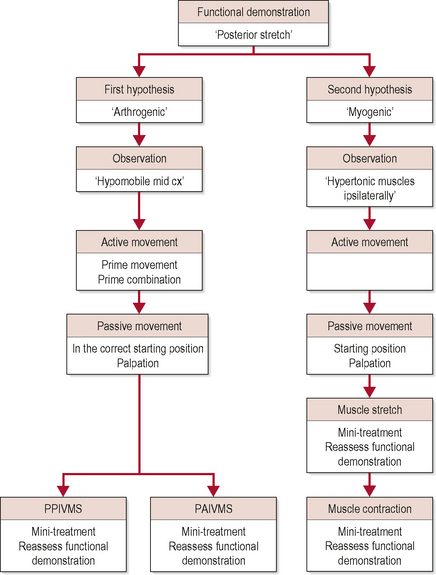
Each component begins with an assessment of movement fault (using the patient’s functional demonstration), testing procedures and a subsequent reassessment of functional demonstration. See Figure 4.2.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree