Fig. 1.1
There are 3 factors that make up the assessment and classification of the stiff shoulder: anatomy, pathology and time (Copyright Dr Gregory Bain)
1.4.1 Anatomical Factors in Normal Joint Function
To produce active motion requires a series of normal physiological events to occur to the normal anatomical structures. This commences with the central nervous system, which initiates the intent to mobilise the joint, which then affects multiple anatomical structures to produce the active motion.
1.4.2 The Shoulder “Machine”
The different anatomical components that must work together to produce functional shoulder movement can be simplified using the analogy of a crane (Fig. 1.2). An electric motor drives a lever arm that moves around a fulcrum. The anatomical components and their function can be divided up according to the different components: electric, motor, tension cable, articulation and lever. The shoulder articulation has several tendons that act across it, creating a series of individual motors that all act on the same fulcrum and lever arm. This creates a balanced system that can control motion and provide dynamic stability to the articulation (Fig. 1.3).
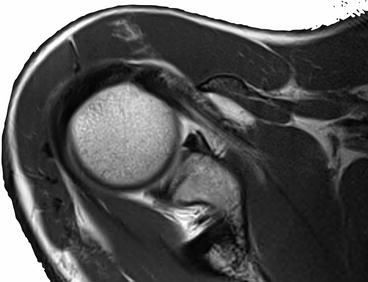
Fig. 1.2
The shoulder machine: with nerve (electrical switch, cord, coordination, sensory feedback), motor (motor and cable) and articular components. Articular components include the joint (bearings), capsular (housing) and osseous components (levers). Not shown are the other local extra-articular components such as the bursa, adventitia and skin (Copyright Dr Gregory Bain)
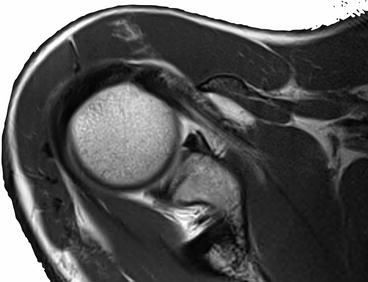
Fig. 1.3
The subscapularis (SSC) and infraspinatus (ISP) work in a coordinated fashion, in front and behind the articulation, to control the motion and provide dynamic stability for the joint. Note that the fascial attachments from the anterior and posterior are joined. This combined motion allows fine control, co-contraction for stability, eccentric contraction for control
1.4.3 Electrical
The central nervous system (CNS) is the control room; it assesses the environment, identifies a need to perform an action and then initiates and coordinates the multiple muscles involved. Activity is modified according to sensory information relayed back from the joint and extra-articular sensory organs. The CNS activates the switch, which is conducted by the peripheral nerves to the muscle motor.
1.4.4 Motor
The motor generates tension in the cable that attaches to the lever arm. Traction on the cable alters the position of the lever arm in space. The muscle is not like a typical motor, but is like a solenoid, which is an electric motor that can contract, but requires to be passively stretched, to regain the muscle length. Altering the tension in the tendon will alter the position of the bone.
1.4.5 Fulcrum
The glenohumeral articular surface is the fulcrum about which the lever (humerus) moves. It has several components that combine to allow efficient conversion of tensile force of the tendon into movement of the humeral lever. The articular cartilage is the bearing surface, with the synovial fluid the lubricant. The fulcrum is constrained by the articular congruency, the labral bumper and the ligaments. The load placed across the articular surface is supported by the subchondral and metaphyseal bone. The rotator cuff tendons reinforce the capsule and provide a dynamic restrain to the articulation, particularly with functional activities.
1.4.6 Lever Arm
The humerus is the lever arm in this system. The cable inserts into the humeral metaphysis and the force is transmitted to the diaphysis. Ultimately this positions the forearm and hand in space.
1.4.7 Other Structures
The surrounding extra-articular structures need to be compliant and not impede upon the motion of the entire lever mechanism. This includes the muscles, adventitia, bursa and skin.
1.5 Pathological Factors in Abnormal Joint Motion
1.5.1 Active vs. Passive Movement
Normal movement of the joint requires all components of the motor and lever system to be functional. If there is an isolated motor deficiency, then there will be weakness and possibly a lag, but there will be a full range of passive motion.
If there is an isolated fulcrum deficiency, then there will be a restriction of passive and active motion, but there will be normal strength.
1.5.2 Pathological Effect
The primary pathological effect will be different depending upon the anatomical site of the pathology.
CNS
Poor control, initiation or coordination of motion, presenting as dyskinesia, tremor and spasticity.
Peripheral Nerves
Signal does not reach the motor, leading to the lower motor neuron signs of flaccid paralysis, wasting and weakness. Failure to relay sensory input back to the CNS will impair the normal modification of activity in response to microtrauma or pain. This can result in a neuropathic arthropathy.
Muscle
Reduced power produced presenting as weakness.
Tendon
Muscular force does not reach the lever arm, presenting as weakness and loss of dynamic control of the articulation.
Articular Surface and Synovial Fluid
The articulation loses its smooth motion, which may present as crepitus, synovitis, effusion and pain. The guarding response to this pain (conscious or unconscious) impairs the shoulder motor.
Capsule
Contracture of the capsule will reduce the passive joint motion. If the capsulolabral complex is insufficient, the joint will be unstable.
Pathology affecting the subchondral bone plate and/or the other load-bearing areas of the scapula and humerus can compromise the ability of the bone to bear the joint reactive force. The fulcrum cannot support the lever arms.
The presence of marginal osteophytes may block the motion of a joint, similar to a wedge placed against the fulcrum, blocking the lever arm from moving.
Extra-articular Tissue
Loss of tissue compliance increases the effort required to mobilise the joint and may impede motion. Examples include contractures of the skin (e.g. burns, trauma and surgery), contractures and heterotopic ossification of the intermuscular planes and thickened bursa.
1.5.3 Individual Pathology
The different elements of the normal shoulder anatomy form a balanced system.
When one element of the system becomes dysfunctional, this will affect the function of other elements. With time, secondary and tertiary pathologies may develop in these other elements. Failure to identify and address these additional pathologies will negatively affect the functional outcome of any treatment.
The unique set of pathological processes present in each patient with shoulder contracture is a function of their premorbid state, the initial insult to the shoulder and their response to that insult over time (Fig. 1.4).
Fig. 1.4
Pathoanatomy of the stiff shoulder. The initial insult was a fall, which produced a tear of the rotator cuff. The response is a failed attempt at healing and development of a capsular contracture with superior migration of the humeral head. The secondary insult is degeneration of the articular surface, which is the final common pathway. Note how anatomy, pathology and time are linked. The presentation is due to three different pathologies, of three anatomical structures at three different times (Copyright Dr Gregory Bain)
1.5.4 Premorbid Status
There are many aspects of the individual that may be important in the development and presentation of the patient:
Congenital or developmental abnormality (e.g. Sprengel shoulder, retroverted glenoid, Ehlers–Danlos syndrome)
Normal individual anatomical variability (e.g. glenoid version, ligamentous laxity)
Epidemiological factors, e.g. age, gender, ethnicity, genetic predisposition [5]
Mental state, e.g. psychological and psychiatric conditions, motivation to rehabilitate, secondary gain issues
Lifestyle factors, e.g. smoking, exercise and physical fitness
Systemic conditions, e.g. diabetes, Dupuytren’s contracture, hypothyroidism and generalised arthritis
1.5.5 Primary Insult
The insult is the event that causes the motor and wheel system to become deranged. This may be an acute event, such as a traumatic fracture or dislocation, or a more chronic process such as inflammatory disease or degenerative changes seen in idiopathic osteoarthritis. Usually there is a single cause of the initial event. The insult may also be due to a systemic condition, such as synovial inflammation due to autoimmune disease or joint haemorrhage due to bleeding disorders. There are many possible pathological disorders that can affect the shoulder motor. The surgical sieve is a commonly used method to ensure that uncommon causes are not overlooked (Fig. 1.5).