Fig. 11.1
Prior SLAP repair in a 34-year-old male, 1 year out from surgery. The rotator interval (RI) is significantly scarred with resultant loss of ER at the side in adduction. The probe is on the anterior loose suture from prior repair. The cannula is through the scarred RI
The importance of CHL release in a refractory frozen shoulder suggests its role in the pathoanatomy of this problem [3, 23] . The CHL is one of the primary restraints to external rotation during shoulder adduction, which is of significance clinically in a frozen shoulder [18, 25], and it is also thought to be the main pathologic structure restricting external rotation [10, 18, 23] and forward flexion in a frozen shoulder (Fig. 11.2). Patients will complain of pain, especially anteriosuperior, and have tenderness in anterior shoulder joint. There will be commensurate losses in motion and pain at the extreme limits of motion.


Fig. 11.2
Starting to release the superior aspect of the RI with a basket cutter
RI lesions can be difficult to evaluate during physical exam since they are often concomitant with anterior, posterior, and multidirectional instability (MDI) [7]. During the examination, it is essential to compare the injured shoulder with the opposite side in order to find any asymmetry in appearance, strength, sensation, stability, or ROM. Asymmetrical loss of ER in abduction may reveal overconstraint of the inferior ligaments, while loss of ER at the side may imply overconstraint of the superior capsule, RI, or SSc [7]. While making a surgical plan, it is imperative to test shoulder stability with focus on glenohumeral ligaments in order to determine the exact type of laxity. The sulcus sign test is a strong predictor of RI lesion [22] (Fig. 11.3). Throughout the test, a downward traction may cause inferior subluxation of the humeral head, and if the sign does not disappear with external rotation, the patient most likely has an RI lesion. In cases where the RI is intact, the sulcus sign will disappear due to proper function of the CHL [20].
Fig. 11.3
(a, b) Sulcus sign test being performed. Downward traction on the arm causes a sulcus sign in internal rotation (a), and presence of the sign in external rotation is a predictable indication for an RI lesion
11.5 Treatment
Different imaging modalities such as computed tomography (CT), MRI, and MRA can be used to diagnose RI pathology [7]. Plain radiographs are usually taken to assess any abnormalities within the joint such as osteoarthritis, glenoid bone loss, or humeral head deficiency. If there is any concern with regard to bony defects a three-dimensional CT reconstruction should be ordered. MRA is the most sensitive of all imaging studies, but if it is not properly performed, it can be extremely difficult to interpret the resulting image [7]. MRI in the oblique, coronal, and axial planes can be useful in assessing the structures within the anterosuperior capsule. In the coronal view, the RI can be seen superiorly from the SSc and inferiorly from the SS, while in the axial plane, the anterior coracohumeral ligament and SGHL can be seen anteriorly from the RI region. These views can be useful to assess thickening of CHL [4].
Initial management strategies are conservative, and the majority of patients with a frozen shoulder do well with symptomatic treatment, activity modification, and physical therapy [24]. Early on, in the acute inflammatory phase, aggressive physical therapy and exercise may be counterproductive, aggravating the patient’s pain. During this phase, analgesia and activity modification prove more useful [24]. As the patient’s pain eases, gentle physical therapist assisted range of motion and patient self-guided exercises are prescribed. A specific four-direction shoulder stretching exercise program has been successful [9].
While the literature reveals mixed reviews, corticosteroid injections are often used in parallel to physical therapy to assist with symptomatic control [9], but whether the pain relief is long term is unknown [11]. Refractory cases of frozen shoulder may necessitate manipulation under anesthesia (MUA) or surgical soft-tissue release. MUA may be done alone, or combined with an arthroscopic soft-tissue release procedure. It is unclear whether manipulation decreases the natural history of a frozen shoulder [1, 26]. Robinson et al. reported that arthroscopic release compared with manipulation in refractory cases has been shown to attain similar range of motion outcomes, but greater pain relief and functional improvement occurred in the arthroscopic release group [24].
The sequence of arthroscopic release and manipulation procedures is debated. MUA prior to arthroscopic capsular release has the disadvantage of uncontrolled tearing of tissues, increase in bleeding, and difficulty with subsequent arthroscopic release. Arthroscopy as the first step has the benefit of better visualization without a post-manipulation hemarthrosis [7] and is the recommended first step in surgical treatment.
The patient may be positioned in the lateral or beach chair position. Once acceptable visualization is established, a thick, robust capsule is usually confirmed. Synovitis and scar tissue within the RI may be debrided with a 3.5–4.0-mm oscillating shaver and electrocautery. Initial release consists of contractures within the RI, including the CHL, anterior capsule, SGHL and possibly the MGHL, and the subscapularis bursa (Fig. 11.4). If present, release of the adhesions between the conjoint tendon and the subscapularis is performed; however, care is taken not to release or cut the SSc (Fig. 11.5). Continuing anteroinferiorly, the anterior capsule and anterior band of the inferior glenohumeral ligament (IGHL) are released. The release is then extended across the axillary pouch lateral to the labrum to allow for improved forward flexion, with caution to avoid the axillary nerve. Further intervention may be performed to release the posterior band of the IGHL and posterior capsule; however, the extent of release is influenced by clinical exam and surgeon preference [24, 27].
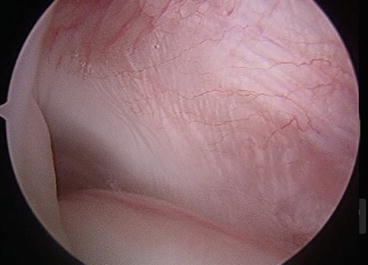
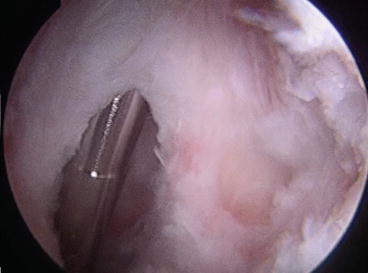
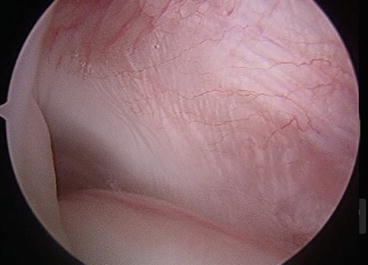
Fig. 11.4
RI contractures are part of the initial release of the RI that will contribute to resolving stiffness
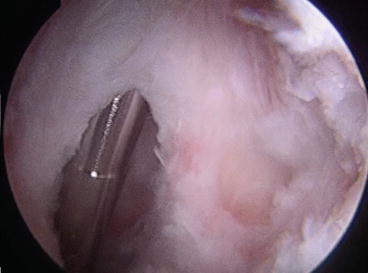
Fig. 11.5
The RI release is shown here, starting medially and extending laterally. Care must be taken not to cut the subscapularis tendon that is located inferiorly
If performed, gentle manipulation is executed in a controlled manner after the controlled arthroscopic debridement, beginning with passive forward flexion to rupture the inferior capsule, followed by external rotation in glenohumeral adduction, then abduction, followed by internal rotation with the arm abducted. Care should be taken to avoid fracture of the humerus and manipulation should not be performed in an osteoporotic patient [6, 17]. A postoperative course of physical therapy is crucial to preserve motion gains, with daily therapy for 2 weeks, followed by a supervised progression of home exercises. Adequate analgesia is critical to promote participation in rehabilitation, and may be administered by an indwelling interscalene catheter postoperatively [24].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








