Fig. 48.1
From left to right: First-generation, second-generation, and third-generation mixing systems, respectively. A liquid monomer and powder are both provided by the supplier

Fig. 48.2
Polymerization process of the cement, the thermal energy yielded allows for a temperature rise of up to 110 °C
Air entrapments during the preparation process account for increased fragility and contribute to micro-crack formation. In the first-generation mixing systems, the cement was manually mixed using a spatula and bowl, consequently introducing a high degree of porosity into the cement. The noxious effects of the methyl methacrylate vapors on the preparer are also not to be neglected. The second-generation systems evolved thereafter with −30 kPa negative chamber systems and contemporary third-generation systems with −70 kPa. The different systems were tested, and the use of negative pressures of at least −70 kPa proved to be best in reducing cement porosity and thereby increasing compressive and flexural strengths, allowing for increasing use by surgeons (Fig.48.3) [5].


Fig. 48.3
Cross section of two cement balls prepared either using the first-generation bowl and spatula method (Left) or third-generation under-pressure mixing system (Right). The image shows a clear reduction in number and size of pores when using the later system
A powder component is added to the liquid component for polymerization of the PMMA. The polymerization time of the cement is about 12–15 min under room temperature. There is a suggested correlation between room temperature and polymerization time.
48.2 Advanced Cementing Technique
Fundamental to the long-term success of a cemented TKR is meticulous bone preparation and careful cement application. Several generations of cementing technique have evolved over the last five decades.
Bone preparation should lead to a clean, dry, and debris-free bone surface. It is well known that bone debris inhibits cement penetration and the presence of blood reduces shear strength by up to 50 % [2, 12]. A pneumatic tourniquet helps to achieve a blood-free bone surface. However, tourniquet time should be limited, in particular when treating multi-morbid patients with a high-risk profile, e.g., high risk of thromboembolic event or peripheral vascular disease. A 5-fold increased risk of thromboembolic events has been shown in patients in whom a tourniquet has been used [15]. However a meta-analysis of the literature showed no difference in the incidence of deep vein thrombosis or pulmonary embolism after TKR with or without tourniquet [1].
The use of lavage should strongly be encouraged due to evidently improved component fixation [17]. Pulsatile lavage in particular was proven most effective in freeing trabecular bone from remaining debris, thereby improving cement penetration and the shear strength of the cement-bone interface (Figs. 48.4 and 48.5) [16].
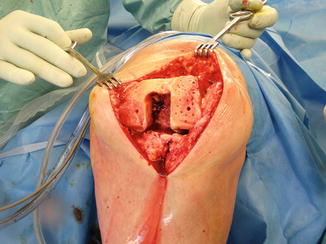

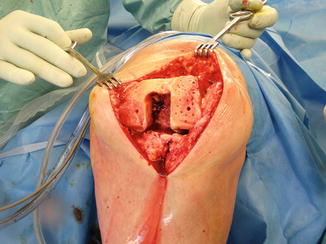
Fig. 48.4
Prepared bone surface after drilling and lavage prior to cementation

Fig. 48.5
Illustration of pulsatile lavage
Bone drilling in sclerotic areas further increases the surface and thus enhances cement penetration.
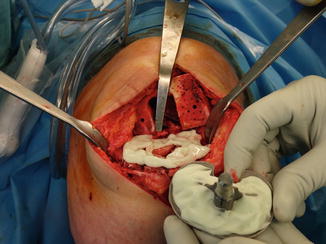
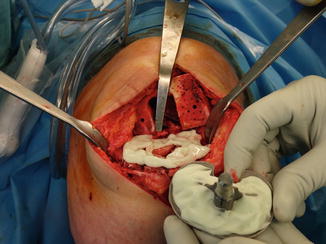
Fig. 48.6
Double cementation technique of tibial TKR component
After meticulous preparation of the bone interface, the TKR component is cemented to the bone (Fig. 48.6). A minimal penetration depth of 4 mm should be achieved for adequate bone-cement resistance [8, 19]. Deep penetration beyond 10 mm is disfavored and is likely to be associated with thermal necrosis, and hence interface weakening, a devastating procedure in the worst case of revision [3]. Penetration depths achieved by pressurized syringes or guns far exceed those achieved by hand cementing alone (5.2 and 4.9 mm vs. 2.4 mm, respectively), and this highlights the benefits of pressurized cement application regardless of the tools used, as less incidence of radiolucencies has been found (Fig. 48.7) [11]. Negative pressure intrusion techniques have only shown benefits in in vitro studies. Due to a lack of clinical evidence, no clear recommendation can be given here.


Fig. 48.7
Pressurized cement gun prepared for use
Cementing for TKR varies regarding the sequence of component cementation. Some surgeons start with the femoral component or patella and others with the tibial component, and the most important aspect regardless of the sequence is caution not to displace a fixed component during cementation of the other. Many surgeons mix a single cement batch for all components, which has a cost and time-sparing advantage. It is, however, fair to note that the process becomes more demanding due to the time pressure of having to cement all components with one countdown. For that reason, it is helpful to mix two separate batches of cement with a 2–3 min time difference, allowing for two separate countdowns and therefore not jeopardize the cementing process for any of the components.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








