Treatment
Therapy
Stage of symptoms
Nonsurgical therapies
Patient education
Acute
Activity modification
Acute
Behavioral therapy
Acute and chronic
Exercise therapy
Subacute and chronic
Oral medication
Non-narcotic analgesic
Acute
Narcotic analgesic
Acute
Nonsteroidal anti-inflammatory drugs
Acute and chronic
Muscle relaxants
Acute
Oral corticosteroids
Acute, only with radiculopathy
Antidepressants
Chronic
Topical treatment
Acute and chronic
Injection therapy
Epidural corticosteroids
Acute, only with radiculopathy
Soft tissue
Subacute and chronic
Facet joint
Subacute and chronic
Sacroiliac joint
Chronic
Modalities
Manipulation
Acute and chronic
Traction
Unknown
Acupuncture
Chronic
Transcutaneous electrical nerve stimulation
Unknown
Orthoses
Not recommended
15.3.1 Education, Activity Modification, Behavioral Therapy, and Exercise Therapy
15.3.1.1 Patient Education
Patient education, including information about correct spine biomechanics during regular activity and posture, and simple methods for reducing symptom are key elements in the management of both acute and chronic back pain. Ensuring that patients understand the favorable natural history of the disorder can empower them to take an active role in the treatment. As past incidences are the strongest predictor for future episodes of back pain, the importance of a lifelong commitment to active treatment must be conveyed to the symptomatic individuals. Several studies have demonstrated that brief education can be more effective than conventional care on reducing sick leave and disability (Brox et al. 2008).
More formal educational interventions have been the subject of investigation since the introduction of the Swedish back school in 1980 (Forssell 1980). The original program was designed to teach patients how to protect the spine during daily activities and involved four educational sessions on spine anatomy, biomechanics, ergonomics, optimal posture, and back exercises in a group setting. The specific format and content of back schools have varied over the years; however, the general concept has been the subject of several investigations and systematic reviews (Airaksinen et al. 2006; Cohen et al. 1994; Koes et al. 1994; Maier-Riehle and Härter 2001; Tveito et al. 2004). In comparison to other interventions or no treatment at all, the results of these studies conflict with the claims for success of back schools in reducing pain, improving function, and accelerating return to work. The most recent systematic reviews (Airaksinen et al. 2006; Brox et al. 2008; Heymans et al. 2005) conclude that forms of group back education can be effective for short-term improvements in pain and disability, especially as part of a multidisciplinary program. In addition, within an occupational setting, back school can have a positive effect on return to work and function.
15.3.1.2 Activity Modification
Most patients with acute back pain naturally modify their activities to avoid exacerbation of symptoms. This subconscious protective mechanism is likely helpful when bounded with appropriate education. It is generally accepted that, while activity may worsen symptoms, it is unlikely to cause physical injury to the spine or the surrounding soft tissues (Indahl et al. 1995). Therefore, the common recommendation is to limit activity for a short period of time (2–3 days). There is, however, strong evidence against the historically common recommendation for bed rest as a treatment for acute low back pain, which can negatively affect outcomes (Atlas and Volinn 1997; Waddell et al. 1997). Results of investigations support the view that after the acute symptoms subside, timely return to modified activities avoids the deleterious effects associated with prolonged immobilization and bed rest. Patients who continue moderate levels of activities during episodes of acute back pain generally have a more rapid recovery, quicker return to work, and a lower risk of chronic disability (Mäkelä et al. 2011; Waddell et al. 1997).
15.3.1.3 Behavioral Therapy
The concept of fear avoidance was introduced as a model of exaggerated pain perception in 1983 (Lethem et al. 1983) and has subsequently been applied to chronic back and musculoskeletal pain (Vlaeyen and Linton 2000; Waddell et al. 1993). Central to this model is the concept that the fear of increased pain, as a result of a movement or activity, may lead to a phobic state and result in inferior physical performance and increased disability. Conversely, confrontation of the fear of pain via exposure to an activity or movement can lead overtime to a reduction in fear. The application of this concept, by including fear-reducing techniques, in the treatment of low back pain in the primary care setting has been shown to produce an increase in activity, but not impact return to employment (Von Korff et al. 2005). Furthermore, when this type of cognitive intervention is combined with an exercise program, the effect on back pain, disability, and sick leave has been shown to be equivalent to that of spinal fusion (Brox et al. 2003; Brox et al. 2006).
15.3.1.4 Exercise Therapy
Exercise therapy, including trunk or core stabilization, restoring normal lumbosacral motion, and low-impact aerobic activity, is among the most commonly prescribed noninvasive interventions for patients with back pain. Based on the current literature, exercise therapy is no more effective for pain relief or functional improvement when compared to no treatment or other nonoperative interventions for acute low back pain (Chou et al. 2007b; Hayden et al. 2005). There is, however, a general acceptance that low-impact cardiovascular and aerobic fitness programs are beneficial in that they can reduce fatigue, improve mood, and prevent general deconditioning (Anshel and Russell 1994; Casazza et al. 1998). Trunk stabilization and muscle strengthening exercises are not tolerated by patients; thus, they are not recommended during acute episodes of back pain. Low-impact aerobic exercise can be commenced as early as tolerated, often by 2 weeks after the onset of acute low back pain, and activity can progress in a graded fashion.
In contrast to the acute situation, for chronic pain, low back pain exercise therapy has been shown to have a beneficial effect (Chou et al. 2007b). When compared to no treatment, usual care, or other noninvasive treatments, exercise therapy has been associated with a small but significant improvement in pain and function (Hayden et al. 2005; Team 2004). Exercise therapy has also been linked with reduced sick leave and a higher rate of return to work within 1 year of treatment in patients with subacute (<90 days of sick leave) low back pain who were not already severely disabled (Oesch et al. 2010). Core strengthening exercises are routinely recommended to improve performance and prevent future injuries (McGill 2010).
15.3.2 Medications
Most patients with both acute and chronic low back pain will include medication in the management of their condition. While the oral route of administration is most common, injections also play a role. The most common classes of oral drugs include analgesics, nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and antidepressants. Injection therapy employs the use of corticosteroids and often local anesthetics. As the choices are numerous, it is important to distinguish specific indications, doses, durations, and potential side effects. Patient education with regard to use of safe and effective medication so as to avoid dependence, particularly when prescribing narcotic analgesics, is an important consideration and should be included in the treatment goals.
15.3.2.1 Analgesics
Analgesic medications can be divided into narcotic and non-narcotic. Few patients require narcotics and most have adequate pain relief from over-the-counter analgesics.
15.3.2.1.1 Non-narcotic Analgesics
Acetaminophen is effective for mild to moderate pain. Although prolonged use of high-dose acetaminophen is contraindicated and may result in hepatotoxicity, acetaminophen is generally safe, affordable, and available over the counter thus making it a common choice for most patients with acute low back pain (Malanga and Nadler 1999). Acetaminophen use in patients with chronic low back pain and with known liver sensitivities due to disease or alcohol abuse is generally not recommended. In patients with renal impairment, acetaminophen is recommended over NSAIDs as the risk of renal toxicity due to acetaminophen is low. Acetaminophen does not have any muscle-relaxing or anti-inflammatory properties.
In patients with more severe pain, the centrally acting non-opiate analgesic tramadol is an attractive alternative as it has a more favorable side effect profile and lower potential for abuse than narcotics. Based on a meta-analysis, which included 908 patients being treated for chronic lower back pain, tramadol was shown to be superior to placebo in reducing pain and improving function (Deshpande et al. 2007). Tramadol inhibits uptake of serotonin and norepinephrine and should therefore be used with caution in patients on monoamine oxidase inhibitors. Dosage should be reduced in patients over the age of 75 years old or in those with renal or hepatic function impairment.
15.3.2.1.2 Narcotic Analgesics
Despite ongoing controversies concerning the use of narcotic (also known as opioid) analgesics for the treatment of chronic low back pain, there has been a steady rise in prescription rates of both long- and short-acting varieties of these medications (Deyo et al. 2011). Concerns with opioid analgesics center around the high risk of dependency and the complications related to overdose, which have risen in parallel to prescription rates (Edlund et al. 2010). The use of narcotics to treat chronic low back pain has been associated with age, psychiatric and personality disorders, and substance abuse as opposed to severity of the underlying pathology (Breckenridge and Clark 2003). With regard to efficacy, there is some evidence to suggest that short-term use of narcotic analgesics may be efficacious; however, long-term use has little or no benefit in reduction of pain (Martell et al. 2007) or improvement of function (Deshpande et al. 2007). When chronic narcotics are prescribed, aberrant medication-taking behavior can be found in as high as 24 % of patients (Martell et al. 2007). Therefore, use of these medications requires regular follow-up to evaluate efficacy, overuse, and complications.
15.3.2.2 Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs are among the most widely prescribed groups of medications for the treatment of back pain. Their mechanism of actions involves inhibition of cyclooxygenase (COX), an essential enzyme for the synthesis of the pro-inflammatory prostaglandins. Two types of COX enzymes exist, with COX-1 implicated in the protection of the gastric and intestinal lining and COX-2 involved in the pathways that produce pain, fever, and inflammation. The first-generation NSAIDs (e.g., ibuprofen, naproxen) nonspecifically inhibit both COX enzymes. The second-generation NSAIDs (e.g., celecoxib, meloxicam) are more selectively directed at COX-2 inhibition. In an effort to reduce gastrointestinal side effects associated with the first-generation NSAID, several randomized controlled studies have demonstrated a significant effect on the improvement of pain and possibly function for the treatment of both acute and chronic back pain (Chou et al. 2007a; White et al. 2011). COX-2-selective NSAIDs are probably as effective as nonselective NSAIDs. Remarkably, there have been few studies that directly compare the two drugs (Pohjolainen et al. 2000). However, both prescription and over-the-counter NSAIDs are associated with adverse effect, including gastrointestinal upset, bleeding, and exacerbation of preexisting renal dysfunction. Patients should therefore be closely monitored, especially with long-term usage.
15.3.2.2.1 Box 15.2 Prostaglandins (PG) Biosynthesis
The starting molecule for PG biosynthesis is the fatty acid of the phospholipid phosphatidylinositol. PG and related molecules are eicosanoids, the term derived from “eicosa” meaning “twenty,” referring to the 20 carbons of the fatty acid. Most PGs are synthesized from arachidonic acid, released by phospholipase A2. PG biosynthesis has two control points. The first control point is the release of the fatty acid from the phospholipid. The second is prostaglandin synthase, also known as cyclooxygenase (COX). The eicosanoids generally act locally due to their short half-lives.


Prostaglandins (PG) biosynthesis. Cox cyclooxygenase, PG prostaglandin, TX thromboxane
15.3.2.2.2 Box 15.3 Cyclooxygenase (COX) Inhibitors
The mechanism of action of NSAIDs is based on their ability to block the synthesis of prostaglandin (PG) by inhibiting COX, an enzyme responsible for catalyzing the conversion of arachidonic acid to prostaglandin, PGH2. In 1991, Daniel Simmons of Brigham Young University discovered a second isoform of the COX enzymes, now known as COX-2 (Xie et al. 1991). Research has since clarified that the COX-1 isoform is a constitutive enzyme responsible for the maintenance of renal and gastric functions. The COX-2 isoform, however, is an inducible enzyme which drives the inflammatory process. The classical NSAIDs (e.g., aspirin, ibuprofen, naproxen) nonspecifically inhibit both COX isoforms and are thus associated with side effects, mostly notable a risk of gastric injury and bleeding. Therefore, since its discovery, there has been a push to develop medications which selectively inhibit the COX-2 isoform and potentially increase the safety profile of these important drugs, primarily by limiting gastrointestinal side effects. The use of computer-aided drug design, where a computer modeling is used to synthesize a drug based on the structure of a particular target, was instrumental in the development of this new drug class. The introduction of COX-2 inhibitors was met with significant enthusiasm, and they became among the most widely prescribed medications. This enthusiasm was tempered when a somewhat controversial study demonstrated a fourfold increased risk of myocardial infarction in patients taking rofecoxib (Vioxx), one of the more commonly prescribed COX-2 inhibitors, when compared to patients taking naproxen, a classical NSAID. Rofecoxib was voluntarily removed from the market by Merck, the drug’s manufacturer, in 2004. Since 2005, no new COX-2 inhibitors have been approved for use in the USA. Other COX-2 inhibitors remain on the market and are still widely prescribed including celecoxib (Celebrex) and parecoxib (Dynastat, only available in Europe). Current research is exploring new application for this class of drugs including prevention or treatment of neuroblastoma, colon cancer, and neuropsychiatric disorders (Lau et al. 2007).
A third isozyme, COX-3, was discovered in 2002; it is thought to be a splice variant of COX-1. Comparison of canine COX-3 activity with murine COX-1 and COX-2 demonstrated that this enzyme is selectively inhibited by analgesic/antipyretic drugs such as acetaminophen and is potently inhibited by some nonsteroidal anti-inflammatory drugs.
COX-inhibiting nitric oxide (NO) donors (aka NO-NSAIDs) are another novel class of drugs developed to further improve the safety profile of the traditional NSAIDs by taking advantage of some of the known effects of NO (Wallace et al. 1994). These are produced by chemically fusing existing NSAIDs to a nitric oxide-donating moiety and are intended to provide the COX-inhibiting benefits in addition to vasorelaxation, and inhibition of white blood cell adhesion and caspase activity (Keeble and Moore 2002). No NO-NSAIDs have been approved for use at this time; however, several are in clinical trials.
Lipoxygenase (LOX)/COX inhibitors are a final novel class of NSAIDs. These drugs inhibit not only COX and prostaglandin formation but also inhibition of 5-lipoxygenase (LOX) and prevent formation of leukotrienes, another family of molecules involved in the inflammatory pathway. LOX/COX inhibitors have been shown to be effective and have a tolerable safety profile in pre-market studies (Alvaro-Gracia 2004).
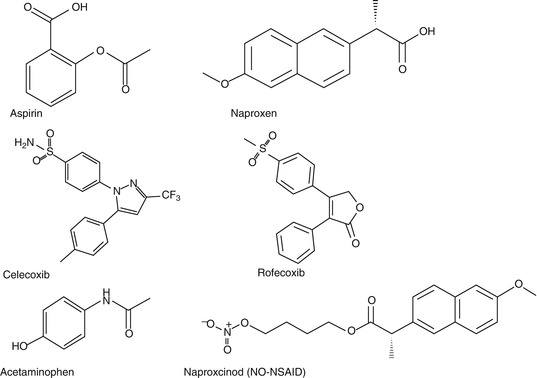
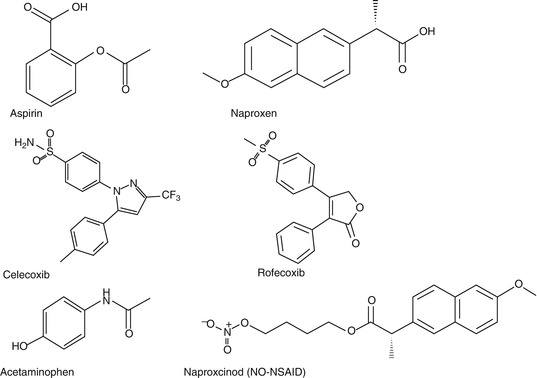
Chemical structure of common cyclooxygenase (COX) inhibitors
References
Alvaro-Gracia JM (2004) Licofelone – clinical update on a novel LOX/COX inhibitor for the treatment of osteoarthritis. Rheumatology (Oxford) 43(Suppl 1):i21–i25
Keeble JE, Moore PK (2002) Pharmacology and potential therapeutic applications of nitric oxide-releasing non-steroidal anti-inflammatory and related nitric oxide-donating drugs. Br J Pharmacol 137(3):295–310
Lau L, Hansford LM, Cheng LS, Hang M, Baruchel S, Kaplan DR, Irwin MS (2007) Cyclooxygenase inhibitors modulate the p53/HDM2 pathway and enhance chemotherapy-induced apoptosis in neuroblastoma. Oncogene 26(13):1920–1931
Wallace JL, Reuter B, Cicala C, McKnight W, Grisham MB, Cirino G (1994) Novel nonsteroidal anti-inflammatory drug derivatives with markedly reduced ulcerogenic properties in the rat. Gastroenterology 107(1):173–179
Xie WL, Chipman JG, Robertson DL, Erikson RL, Simmons DL (1991) Expression of a mitogen-responsive gene encoding prostaglandin synthase is regulated by mRNA splicing. Proc Natl Acad Sci U S A 88(7):2692–2696
15.3.2.3 Muscle Relaxants
Acute back pain is often accompanied by muscle spasm, but the association with pain is not well understood. Nonetheless, both benzodiazepine (e.g., diazepam) and non-benzodiazepine (e.g., cyclobenzaprine, methocarbamol) muscle relaxants are often prescribed as part of the treatment regimen. Systematic reviews of clinical trials have found that muscle relaxants are superior to placebo for the treatment of acute and chronic low back pain (Chou et al. 2007a; Van Tulder et al. 2003). There are no well-controlled studies that directly compare the efficacy of muscle relaxants to that of NSAIDs. Muscle relaxants are likely to be most beneficial as an adjunct to pharmacologic therapies with other drug classes, specifically NSAIDs and analgesics (Chou et al. 2007a; Van Tulder et al. 2003). There is little evidence to aid with the selection of one muscle relaxant over the others. Carisoprodol was found to be superior to diazepam in one study (Van Tulder et al. 2003). However, due to issues with dependency and abuse when combined with narcotics, the use of carisoprodol is generally limited. Muscle relaxants have been shown to lead to a number of central nervous system adverse effects, including somnolence and dizziness. These are increased when used in conjunction with other medications and should be closely monitored by the treating physician.
15.3.2.4 Oral Corticosteroids
The systemic administration of corticosteroids can be an effective treatment for patients with acute radiculopathy. However, when back pain is not accompanied by radiculopathy, studies have shown no clinically significant benefit over placebo (Chou et al. 2007a). Systemic corticosteroids can have a significant side effect when administered over the long term or in high doses in the short term. Thus, this class of medications is only recommended for the treatment of low back pain with radiculopathy.
15.3.2.5 Antidepressants
There is an intimate association between pain and mood, especially in chronic pain disorders (Fishbain et al. 1997). While the mechanism is unknown, there is some evidence that tricyclic antidepressants (TCAs) can effectively alleviate neuropathic pain, independent of mood or depression status (McQuay et al. 1996). Serotonin reuptake inhibitors (SSRIs) are less effective than TCAs; however, they are prescribed for neuropathic pain (Jung et al. 1997). The utility of antidepressants in the treatment of low back pain is not as clear. The efficacy of both tricyclic antidepressants and selective SSRIs has been the subject of several studies and recent systematic reviews. There is no generally accepted role for antidepressants in the treatment of acute back pain. For chronic back pain, TCAs have been demonstrated to be moderately effective in pain reduction when compared to placebo (Chou et al. 2007a; Staiger et al. 2003; White et al. 2011). As with neuropathic pain, SSRIs are not as effective as TCAs and offer no benefit over placebo. The effect of antidepressants on function is not clear (Staiger et al. 2003). Antidepressants can have significant side effects, including drowsiness, dry mouth, dizziness, and constipation. Some of these adverse events can be mitigated with low starting doses that are slowly titrated up for efficacy. Due to the sedative properties of TCAs, these drugs should be administered at night and may in fact improve the sleep disturbance often associated with chronic back pain (Harman et al. 2002).
15.3.2.6 Topical Treatments
Both topical NSAIDs and local anesthetics in the form of patches, creams, or gels are used to treat low back pain. Topical application of NSAIDs is attractive as it can theoretically reduce the adverse events associated with their systemic administration. It should be noted, however, that with all topical formulations, systemic NSAID absorption occurs to variable degrees and adverse effects have been documented (Zimmerman et al. 1995). There is evidence to suggest that topical NSAIDs are effective for the treatment of musculoskeletal pain, although there is no evidence with regard to their efficacy specifically for acute or chronic back pain (Haroutiunian et al. 2010). Adhesive local anesthetic lidocaine patches are also often used to treat back pain. Again, their efficacy is unknown. Thus, topical treatments should be used with discretion and caution as adjuvants to other treatment modalities.
15.3.3 Injection Therapy
Therapeutic injections are often incorporated into back pain treatment regimens, particularly after less invasive methods, including exercise and oral medications, have failed. Injections can be directed at anatomic location both within and around the axial skeleton. Injection therapy should only be considered when a reasonable etiologic diagnosis has been made and should not be used for nonspecific low back pain.
15.3.3.1 Epidural Corticosteroid Injections and Medial Branch Blocks
Injection of corticosteroid, often with local anesthetic, is commonly administered for treatment of acute and chronic spine pathology. The medication can be delivered via an interlaminar, caudal, or transforaminal approach, depending on the pathoanatomy and specific patient symptoms. The potent anti-inflammatory effects of the corticosteroids coupled with the analgesic effects of local anesthetics are thought to interrupt the pain and spasm cycle as well as nociceptive transmission. Preclinical experiments suggest that corticosteroids can reduce cell membrane permeability, diminish neural peptide synthesis and neuronal discharge, and moderate sensitization of dorsal horn neurons (Byröd et al. 2000; Devor et al. 1985; Lee et al. 1998). While specialized training is required for all epidural injections, caudal injection is the least technically demanding and has a lower risk of dural puncture when compared to the other approaches. Transforaminal injections must be directed at specific pathologies, while interlaminar injections can result in more broad distribution of medication. Fluoroscopy is routinely used to improve the accuracy of injection needle placement, although an improvement in efficacy has not been proven (Chou et al. 2009a).
The efficacy of epidural corticosteroid injections has been the subject of multiple studies and reviews. In patients with back pain accompanied by radiculopathy, there is some, albeit weak, evidence to suggest the epidural corticosteroid injection provides short-term (up to 6 weeks) pain relief (Carette et al. 1997; Karppinen et al. 2001; Ng et al. 2005). There is, however, no evidence that epidural corticosteroid injections are effective in patients with back pain without radicular symptoms and they are, therefore, not a recommended treatment option (Chou et al. 2009a, b). When epidural injection therapy is pursued, a series of two to three injections is often recommended. Generally, no more than three injections are administered over a 6–12-month period, and if there is no response to the first injection, there is some evidence to suggest that further injections within the acute period are unlikely to be of significant benefit (Arden et al. 2005). Complications from epidural injections are rare; however, dural puncture, epidural hematoma, spinal cord injury, infection, and nerve damage have been reported (Chou et al. 2009a).
15.3.3.2 Soft Tissue Injections
Injections for back pain outside of the spine, the most common being trigger point injections, are targeted at soft tissue structures believed to be significant pain generators. These treatments involve the injection of local anesthetic and/or corticosteroid into specific myofascial trigger points, which are thought to result from irritable foci of taut muscle bands. Focal pressure on these points should produce a local twitch response with distally referred pain (Kraus and Fischer 1991). This so-called myofascial syndrome generally responds to a regimen of exercise or manual therapy, with injections considered as an adjuvant. The evidence to support local trigger point injection therapy alone is weak, showing short-term relief for subacute or chronic back pain (Chou et al. 2009a, b). However, some studies showed no difference when compared to placebo, and the addition of corticosteroid to local anesthetic does not appear to exert a significant effect. Therefore, the number of intramuscular injections should be limited, as there is concern for development of muscle damage, scar tissue, and altered function after multiple injections.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








