Chapter 8 The Nonmanipulable Subluxation
After reading this chapter you should be able to answer the following questions:
| Question 1 | Is there a difference between hypermobility and instability? |
| Question 2 | Are there any contraindications to manipulation noted on these radiographs? |
| Question 3 | What procedural error did the practitioner make when taking this x-ray series? |
The first problem confronting the clinician in the evaluation of a nonmanipulable subluxation is lack of consistency of terminology; the second problem is recognizing the associated clinical and radiologic signs. A nonmanipulable subluxation is a vertebral motion segment with radiologic or clinical features indicating that an adjustive force or osseous manipulation to this motion segment would be harmful or dangerous and is therefore contraindicated. Although it is well recognized that many pathologic processes affecting the skeletal system, such as malignant tumors and infections, are absolute contraindications to manipulation of the affected area, this chapter focuses on those conditions that may result in hypermobility, instability, or osseous fusion of the spinal motion segment. See Table 8-1 for criteria for defining nonmanipulable subluxations.
Table 8-1 Criteria for Defining Nonmanipulable Subluxations
| Condition | Characteristics | Manipulation |
|---|---|---|
| Hypermobility | Excessive motion (reversible) | Nonrepetitive |
| Instability | Insufficient soft tissue (irreversible) | Contraindicated |
| Congenitally blocked segment | Motion absent (irreversible) | Contraindicated |
| Surgically fused segment | Motion absent (irreversible) | Contraindicated |
Definitions of Instability and Hypermobility of the Cervical Spine
Clinical instability of the spine is defined as follows:
Loss of the ability of the spine under physiologic loads to maintain relationships between vertebrae in such a way that there is neither damage nor subsequent irritation to the spinal cord or nerve roots, and in addition, there is no development of incapacitating deformities or pain due to structural changes.1
The terms instability and hypermobility are often confused, both in practice and in the literature.2–5 It is important to differentiate between these two conditions as they relate to the spine because the clinical significance and thus the therapeutic approaches to the these two entities are not the same. Segmental hypermobility has been defined as follows:
The mobility of a given motion unit (segment) which is excessive but not so extreme as to be life-threatening or require surgery.5
Several authors claim that hypermobility may be a precursor to the development of instability at a later date if not properly managed.2,3,6 Some think that hypermobility is “… a distinct category along a continuum from normal joint motion to pathological movement.”5
Chiropractic principles emphasize the importance of manipulating those motion segments that are fixed, or hypomobile, with the goal of restoring normal motion,7,8 while avoiding motion segments that are already hypermobile, or unstable.8,9 With this goal in mind, how are nonmanipulable subluxations recognized?
Excessive intersegmental motion to the degree that damage to the spinal cord or nerve roots becomes a potential hazard has several causes. These include acute trauma, repetitive microtraumas, congenital anomalies, degenerative and inflammatory arthropathies, surgical fusions and laminectomies, and compensatory phenomena caused by loss of motion in adjacent segments.6,10–12
Clinical Manifestations of Hypermobility and Instability in the Cervical Spine
Segmental hypermobility in children may simulate the symptoms of chronic rheumatic disease, making it difficult to properly diagnose.5 Adult patients may complain of a variety of symptoms that seem to be slowly progressive, building over a period of years. The complaints include recurrent episodes of neck pain, which is often described as “dull” or “aching,”5 with or without muscle spasm. The pain is either unilateral or bilateral and commonly located in the area of C5-C6. There may be associated crepitus in the neck at the end ranges of motion, and the patient often complains of “tight, tired, stressed” feelings throughout the neck. Headaches may be associated.5 These clinical features are nonspecific and alone would not necessarily make the clinician think of excessive segmental motion. Some authors claim that cervical instability (they do not differentiate hypermobility from instability) is related to loss of the lordosis.11 This finding alone, however, is insignificant because many factors may produce loss of cervical lordosis, including the fact that it can be normal and asymptomatic. Additional physical examination findings include hypertrophy of the anterior neck and anterior chest musculature with protraction of the scapula and elevation of the clavicles. Active and passive ranges of motion are usually limited. Segmental palpation may show hypermobility of the involved segments with restrictions above and below the affected levels.5,11 Patients with segmental hypermobility are more likely to exhibit symptomatic degenerative joint disease (DJD) than those patients with DJD with no hypermobility.5 Actual segmental instability may demonstrate similar clinical findings to hypermobility with the additional potential for neurologic signs and symptoms and progressive deterioration.6,10
Radiographic Evaluation of Hypermobility and Instability in the Cervical Spine
The definitive diagnosis of intersegmental hypermobility and instability has relied on the evaluation of kinematic radiographic studies of the cervical spine in the sagittal plane.5,6,10,12–15 The chiropractic profession has used these radiographs for decades to assess global range of motion and intersegmental range of motion and to attempt to objectify the effects of manipulation.15,16 Neutral, flexion, and extension lateral radiographs are taken by various methods devised for assessing normal and abnormal motion.6,7,12,14–17 These studies have traditionally been performed actively by the patient without reinforcement by the doctor. Dvorak et al.,12 however, emphasize the value of obtaining functional radiographic studies of the cervical spine both with the patient actively moving the neck and passively, with the doctor forcing the patient’s neck beyond the point where the patient actively ceases motion. They claim that many more hypermobile segments are discovered on the passive kinematic studies as compared with evaluating active flexion/extension radiographs only. Caution is advised when passively forcing the patient beyond the active range of motion since further damage may be caused to previously injured structures.
Spinal radiographs can be analyzed by hand, using templating procedures (see Chapter 6) or with the aid of computer digitizing. Digital video fluoroscopy is also used to assess the entire intersegmental motion.13,14 (See Chapter 20.) The various assessment methods emphasize measuring translation in the sagittal plane, analyzing intervertebral angles, and calculating the axes of rotation.6,17,18 There is consensus that the quantity of normal intersegmental motion varies considerably between the various motion segments of the cervical spine and that this intersegmental motion decreases with increasing age.6,13,14,16 Some authors state that the “amount” of motion at an intervertebral segment is not as important as the “path” of the motion.13
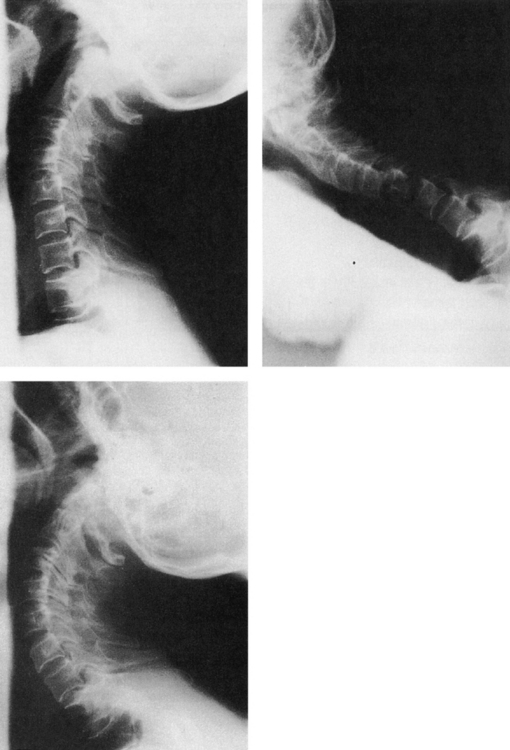
Henderson and Dormon6 developed a method of assessing intersegmental motion in the sagittal plane that can easily be applied to flexion and extension radiographs in clinical practice. Normal and abnormal intersegmental motion is defined in terms of a percentage of the sagittal body diameter (SBD). Absolute hypermobility is defined as intersegmental motion that falls between 61% and 72% of the sagittal body diameter, whereas instability is any motion exceeding 72% of the SBD. This is one of the only studies to attempt to objectively differentiate hypermobility from instability. It is useful as a guide as long as the clinician keeps in mind that the range of normal segmental motion differs between and within subjects. Other studies have defined instability as a translation in the sagittal plane of one vertebra on another in excess of 3.5 mm during flexion to extension.18 This is a useful and simple method for evaluation of excessive joint motion. Figure 8-1 demonstrates neutral, flexion, and extension lateral radiographs of a patient with an anterolisthesis of C3 (evident on neutral film) along with facet arthrosis between C2 and C3. Notice that the anterolisthesis increased during flexion and completely reduced during extension, giving an overall excursion of approximately 4 mm. This figure is consistent with a diagnosis of intersegmental instability, and this motion segment should not be manipulated.
Causes of Cervical Spine Hypermobility and Instability
Acute Trauma
Figure 8-2 represents the flexion and extension lateral radiographs of a teenage girl who fell onto her head while doing handstands at school. She complained of neck pain and stiffness immediately after the incident.
The flexion-extension radiographs of the young woman in Figure 8-2 demonstrate several of the classic signs of posttraumatic instability caused by ligamentous and discal injury at C4-5.
There is an acute kyphotic angulation between C4 and C5 with an anterolisthesis of C4, fanning of the spinous processes, gapping and overriding of the articular facets, and a loss of disc height at this level. The findings do not completely reduce on the extension film and would have been evident on a neutral lateral radiograph. The dangerous error made by the clinician responsible for this radiographic series was to have taken flexion-extension films in the first place because of the history of recent trauma.
In cases of acute cervical trauma, the neutral lateral radiograph must be taken first and scrutinized thoroughly for any signs of instability and ligamentous damage before subjecting the patient to motion studies.10,12,19 If any signs of instability are noted, flexion-extension radiographs, as well as manipulation, are contraindicated. The patient should be placed carefully into a cervical collar and taken to the hospital. Halo bracing and surgical fusion are the appropriate treatments for acute traumatic instability. In addition to these signs, prevertebral swelling, displacement of the prevertebral fat stripe, and an increase in the ADI (atlantodental interval) may be noted in patients with acute posttraumatic instability.19
Latent or occult posttraumatic instability of the cervical spine is the physician’s nightmare because the initial neutral lateral cervical radiograph may be seen as “normal.” Reasons for this include technically inadequate radiographs; for example, the lower cervical spine may be obscured by the shoulders, muscle spasms may temporarily reduce a displaced vertebra, or hyperextension/hyperflexion dislocations may spontaneously reduce on recoil of the neck.10,19 In such cases, careful analysis of the neutral lateral radiograph may show the warning signs of prevertebral soft tissue swelling and displacement of the prevertebral soft tissue stripe. An upright neutral lateral radiograph must be taken because subtle signs of posttraumatic instability may not be visible on supine cross-table lateral radiographs.19
Anomalies
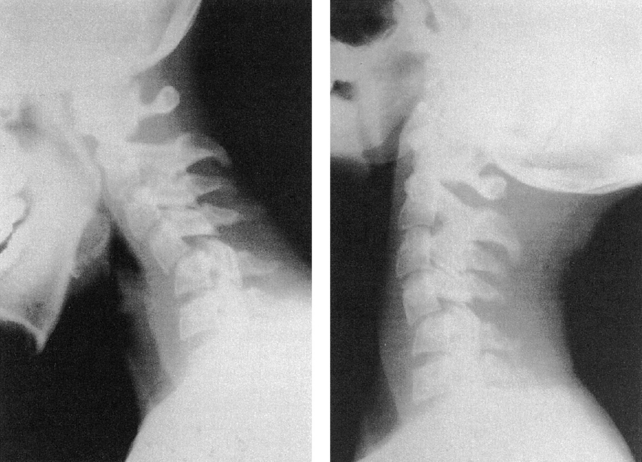
Look at the radiographs of the 60-year-old woman in Figure 8-3, A and B. This patient complained of neck pain and stiffness after an automobile accident.
Was her automobile accident responsible for the radiographic changes seen?
This type of question plagues clinicians daily and is one that usually has no definite answer. If you said that this patient has a dens fracture caused by her recent trauma, you are 100% wrong! There is definitely instability of C1 on C2 as noted by the marked translation in the sagittal plane during flexion and extension. Perhaps the accident caused her to rupture her transverse ligament? Wrong again. Posttraumatic rupture of the transverse ligament is very rare, and the patient is more likely to fracture the dens than to rupture this ligament.19,20 The clue on the lateral views lies in the shape of the anterior tubercle of C1. Rather than the classic “D” shape with a straight posterior margin, this patient’s anterior tubercle is rounded and hypertrophied. This important radiographic sign indicates an anomaly of the upper cervical complex.20 You may have noticed that the dens was not visualized on the lateral view, and the open-mouth projection provides the evidence that the dens is absent (Figure 8-3, C). Other anomalies of the upper cervical spine that may result in instability include the os odontoideum and odontoid hypoplasia.20 Flexion-extension views are indicated when anomalies are suggested to determine the presence or absence of instability. Translation in the sagittal plane of more than 3.5 mm18 is considered instability, and these patients should be referred for surgical consultation.
Blocked Vertebrae
Figure 8-4 depicts the classic congenital blocked vertebra at C5-C6 with normal bone density, normal vertebral body height, wasp waist, and remnant disc. Congenital blocked vertebrae are common anomalies whose clinical significance relates to the effect that this fusion has on adjacent mobile segments, and not to the fact that two segments are fused together.6,20 Obviously, chiropractors do not attempt to manipulate blocked vertebra. What must be remembered, however, is that blocked vertebrae, whether they are congenital or surgical (Figure 8-5), can result in increased motion and potential instability at adjacent motion segments.6,20 The patient in Figure 8-4 has large osteophytes at the adjacent anterior body margins between C6 and C7, indicating probable instability at some time. Whether this motion segment or the upper cervical motion segments are currently unstable cannot be determined on this neutral lateral film alone. Clinicians must be cognizant that the fused segments can cause adjacent hypermobilities or instabilities and must thoroughly evaluate these patients before manipulation.
Absence of the Transverse Ligament in Down Syndrome
Down syndrome, or mongolism, is a common congenital abnormality caused by trisomy of the twenty-first chromosome. The significance of this syndrome to chiropractors is that up to 20% of people with Down syndrome are born without a transverse ligament and are prone to instability of C1 on C2. Every patient with Down syndrome must be checked for this potentially life-threatening condition by taking a flexion lateral radiograph before manipulation of the upper cervical spine to evaluate the ADI.20 A measurement of greater than 5 mm in the child or 3 mm in the adult is abnormal.20,21
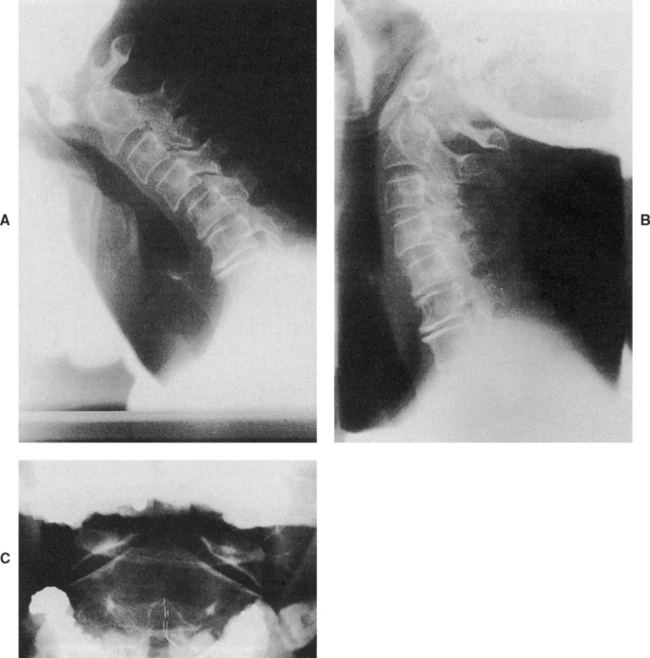
Inflammatory Arthropathies
Now look at the flexion lateral film in Figure 8-6, B. The neutral lateral radiograph (Figure 8-6, A) demonstrates mild degenerative disc disease in the middle and lower cervical spine (C7 is not included on the film). The ADI is within normal limits. This is not the case, however, on the flexion lateral film of the same patient! The ADI now measures 6 mm, well above the maximum normal value of 3 mm. Note also the anterior displacement of the posterior spinal line, another indicator of C1-2 instability. Without the flexion lateral view, the clinician would not have realized that this patient, who has a history of rheumatoid arthritis (RA), has ruptured her transverse ligament and now has a potentially life-threatening instability. Obviously, manipulation is contraindicated in her upper cervical spine. Rheumatoid arthritis is notorious for affecting the upper cervical complex. As many as 40% of RA patients develop atlantoaxial subluxation in the course of the disease.21 Other causes of instability with RA include erosion of the dens, posterior arch, and destruction of the alar ligaments.21
Although rheumatoid arthritis is the most common of the inflammatory arthropathies that cause rupture of the transverse ligament, it must be remembered that any of the inflammatory arthropathies, for example, ankylosing spondylitis, psoriatic arthritis, Reiter’s syndrome, systemic lupus erythematosus, and juvenile rheumatoid arthritis, also can rupture this ligament and cause instability.20,22
Ankylosing spondylitis, as its name implies, can lead to osseous spinal fusion. Spinal manipulative therapy is not of benefit once these segments have become fused. However, as described under congenital and surgical blocked vertebrae, motion segments that are fused predispose nonfused segments to become hypermobile or unstable.6,20
Figure 8-7 depicts the lateral cervical radiograph of a man with longstanding ankylosing spondylitis with the typical appearance of the “bamboo spine.” He suffered a minimal trauma recently and can suddenly move his neck better than he has been able to in years. He is thrilled and believes that the accident has helped his ankylosing spondylitis. Do you agree?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree