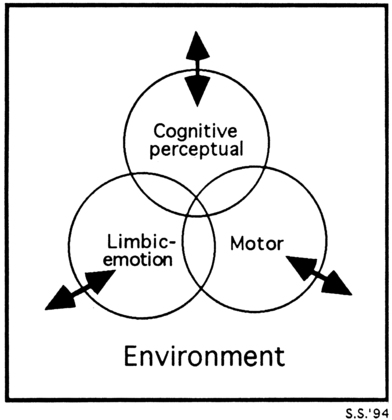
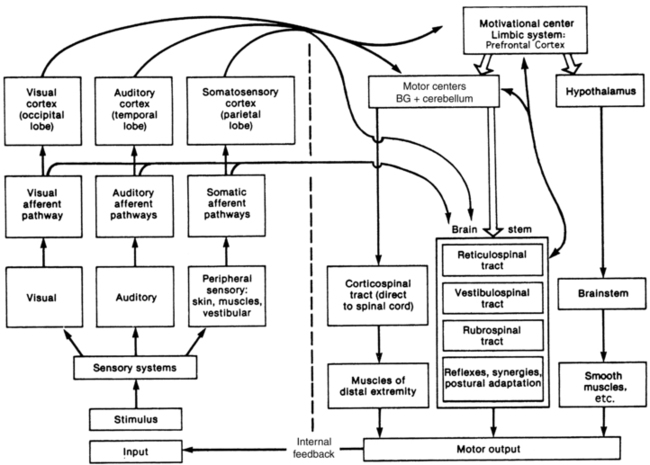
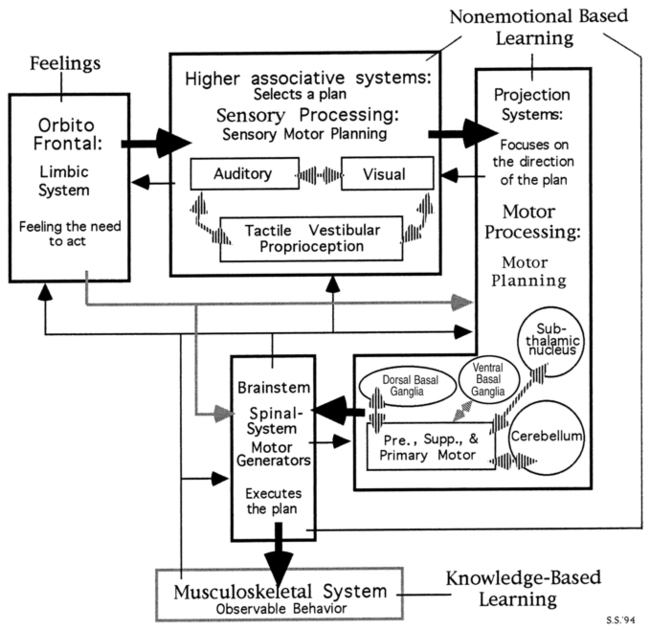
DARCY A. UMPHRED, PT, PhD, FAPTA, MARCIA HALL THOMPSON, PT, DPT, DSc and THERESE MARIE WEST, PhD, MT-BC, FAMI After reading this chapter the student or therapist will be able to: 1. Understand the complexity of the limbic network and the influence of the limbic network on behavioral and functional responses. 2. Describe the behavioral responses directly influenced by the limbic network. 3. Describe the structures of the limbic network. 4. Describe the interaction between the limbic network and body systems responsible for behavioral responses. 5. Differentiate between limbic-driven motor control responses and frontal, cerebellar, and basal ganglia motor regulation. 6. Differentiate between declarative and procedural learning. 7. Identify signs of both positive and negative limbic network influence on a client’s observable behavior and functional responses. 8. Describe appropriate treatment interventions or program modifications for both the limbic high and limbic low client. 9. Understand the influence of the therapist over the limbic network and behavioral and functional responses, and effectively integrate limbic network treatment techniques into current treatment models. Since the publication of the fifth edition of this book, the limbic network has emerged as a key component of central nervous system (CNS) function, becoming one of the most researched areas of the CNS when analyzing behavior, learning, emotions, and their influence on activities and participation. In the past, review of the literature on the limbic network was limited to investigating potential interactions of other systems with nuclei within the limbic network. This is no longer the case, as neuroscience research has helped to identify the critical nature of behaviors controlled or influenced by the limbic network. Based on research at a cellular level,1–3 a consciousness level,4–7 a bodily systems level,8–10 and a quantum level11–13 it is now clear that the motor system is just one of the many systems affected by the complex limbic network.14–21 Obviously, the human organism is a complex totality made up of many interlocking parts. The medical system has traditionally divided the body into systems and has forgotten that each specific system is co-dependent on many other systems for function. Today the medical profession is rediscovering the importance of how the systems interact with and influence one another.22,23 It is very important that movement specialists do not fall into the same trap as medicine in the past and look at movement from only a biomechanical, muscular, neurological, cardiopulmonary, or integumentary system perspective. They must consider the interaction among systems and their subsystems within an individual. For example, the motor system is a system in and of itself. But cognitive impairment and limbic network involvement can lead to tremendous errors in motor responses even when the motor system is intact. In our clients with CNS dysfunction, impairments exist in the motor and limbic network and in cognition, thus creating the potential for a complex set of behavioral responses to internal or external environmental influences. The concept of patient/client-centered therapy has evolved to become an important aspect of health care delivery.24–34 The desire to improve or regain function can be self-motivated, but very often it is instilled through the clinician to the patient that his or her best interests and unique goals are the focus of the health care team. This belief is based on trust, hope, and attainable steps toward desired and realistic goals. Patients know that their desires, interests, and needs as unique and valued members of society are considered. They first believe and then recognize that they are persons with specific problems and desired outcomes. Although they may have specific medical diagnoses, be placed on clinical pathways, administered drugs, and sent off to the next facility in a couple of days, patients need to feel that they, as individuals, have not lost all individuality and that someone cares. That need is a feeling of security and safety that bonds a patient to a therapist along the journey of learning.35–37 Before understanding and becoming compassionate regarding the needs of other people, such as patients with signs and symptoms of neurological problems, therapists need to understand their own limbic network and how it affects others who might interact with them.38–43 Because both occupational and physical therapy professions have evolved to using enablement models and systems interactions to explain movement responses of their respective client populations, separating limbic from true motor or cognitive impairments will help guide the clinician toward intervention strategies that will lead to the quickest and most effective outcomes. The complexity of the limbic anatomy, physiology, and neurochemistry baffles the minds of basic science doctoral students. The changes in understanding of cellular metabolism, membrane potentials, and the new mysteries of cell communication and memory perplex the world of science and neuroscience.44–47 How this microcosm relates to the macroworld and how the external environments influence not only consciousness but all levels of CNS function are slowly unraveling but still remain mysteries. Yet a therapist deals with the limbic network of clients on a moment-to-moment functional level throughout the day. Figure 5-1 illustrates the interlocking co-dependency of all major CNS components with the environment. At no time does any system stand in isolation. Thus from a clinical perspective the therapist should always maintain focus on the whole environment and all major interactive components within it, while directing attention to any specific component. How the feedback (internal and external) to the patient’s CNS changes the neurochemistry and membrane potential, triggers memory, creates new pathways, or elicits other potential responses is not the responsibility of the clinician or therapist. The responsibility of the clinician is accurate documentation of changes and consistency of those changes toward desired patient outcomes. The professions that focus on movement science are interacting more closely with the neurosciences and other biological sciences and many related professions to unravel many of these mysteries and create better assessment and intervention procedures for future patients. The primary purpose of this chapter is to discuss the influence of the limbic network on motor learning, motor performance, neuroplasticity, and functional independence in life activities. If a person is fearful or apprehensive, motor performance and the ability to learn either a motor skill or intellectual information will be very different48–55 from that of an individual who feels safe, is given respect, and becomes part of the decision-making process and thus functions inherently with control.52,56–61 An individual will naturally have feelings of loss and reservations or fears about the unknown future after injury to any part of the body, but especially the CNS (see Chapter 6). Yet that individual needs to be willing to experience the unknown to learn and adapt. The willingness, drive, and adaptability of that individual will affect the optimal plasticity of the CNS.62 The limbic network is a key player that drives and motivates that individual. The lack of awareness of that variable or its effect on patient performance will ultimately lead to questions and doubts about the effectiveness and efficacy of both assessment and intervention results. Similarly, if this system is overwhelmed either internally or externally, it will dramatically affect neuroplasticity and motor learning as well as cognitive, syntactical learning (see Chapter 4). At the conclusion of this chapter it is hoped that therapists will comprehend why there is a need to learn to modulate or neutralize the limbic network so that patients can functionally control movement and experience cognitive learning. Then therapists need to reintroduce emotions into the activity and allow the patient to once again experience movement and cognitive success during various levels of emotional demands and environments. This change in the emotional environment will create novelty of the task. This novelty is a critical motivator for learning and will drive neuroplasticity.63–65 It is not easy to find a generally accepted definition of the “limbic network or complex,” its boundaries, and the components that should be included. Mesulam66 likens this to a fifth-century bce philosopher’s quotation, “the nature of God is like a circle of which the center is everywhere and the circumference is nowhere.” Brodal67 suggests that functional separation of brain regions becomes less clear as we discover the interrelatedness through continuing research. He sees the limbic network reaching out and encompassing the entire brain and all its functional components and sees no purpose in defining such subdivision. Although the anatomical descriptions of the limbic network may vary from author to author, the functional significance of this system is widely acknowledged in defining human behavior and behavioral neurology.68 Brooks69 divides the brain into the limbic brain and the nonlimbic sensorimotor brain. He also defines the two limbic and nonlimbic systems functionally, not anatomically, because their anatomical separation according to function is almost impossible and task specific (Figure 5-2). The sensorimotor portion is involved in perception of nonlimbic somatosensory sensations and motor performance. Brooks defines the limbic brain component as primitive and essential for survival, sensing the “need” to act. The limbic brain is also responsible for memory and the ability to select what to learn from each experience, either positive or negative. Thus the overall purpose of the limbic network is to initiate need-directed motor activity for survival, based on experience. The limbic network therefore initiates and can send neurons up to the frontal lobe or down to the brainstem and thus regulates motor output. Kandel and colleagues56 state that functional behavior requires three major systems: the sensory, the motor, and the motivational or limbic systems. When a seemingly simple action, such as swinging a golf club, is analyzed, the sensory system is recruited for visual, tactile, and proprioceptive input to guide the motor systems for precise, coordinated muscle recruitment and postural control. The motivational (limbic) system does the following: (1) provides intentional drive for the movement initiation, (2) integrates the total motor input, and (3) modifies motor expression accordingly, influencing both the autonomic and the somatic sensorimotor systems. It thereby plays a role in controlling the skeletal muscles through input to the frontal lobe and brain stem and the smooth muscles and glands through the hypothalamus, which lies at the “heart” of the limbic network (Figure 5-3). Noback and co-workers70 state that the limbic network is involved with many of the expressions that make us human; namely, emotions, behaviors, and feeling states. That humanness also has individuality. Our unique memory storage, our variable responses to different environmental contexts, and our control or lack thereof over our emotional sensitivity to environmental stimuli all play roles in molding each one of us. Because of this uniqueness, each therapist and each client need to be accepted for their own individuality. Broca71 first conceptualized the anatomical regions of the limbic lobe as forming a ring around the brain stem. Today, neuroanatomists do not differentiate an anatomical lobe as limbic, but rather refer to a complex system that encompasses cortical, diencephalon, and brain stem structures.56 This description is less precise and encompasses but is not limited to the orbitofrontal and prefrontal cortex, hippocampus, parahippocampal gyrus, cingulate gyrus, dentate gyrus, amygdaloid body, septal area, hypothalamus, and some nuclei of the thalamus.56,72–76 Anatomists stress the importance of looking at the interrelated structures and segments or loops within the complex limbic region.77,78 These multiple nuclei and interlinking circuits play crucial roles in behavioral and emotional changes77,79,80 and declarative memory.79–96 The loss of any link can affect the outcome activity of the whole circuit. Thus damage to any area of the brain can potentially cause malfunctions in any or all other areas, and the entire circuit may need reorganization to restore function. Researchers do not ascribe a specific single function to CNS formations but see each as part of a system participating to various degrees in the multitude of behavioral responses (see Chapters 3 and 4 for additional information). Therefore the loss of any part of higher centers or the limbic network may not be clearly definable functionally, and the return of function is not always easy to predict. Recovery of function after injury may involve mechanisms that allow reorganizing of the structure and function of cortical, subcortical, and spinal circuits. In very young infants, areas within opposite hemispheres may “take over” function, whereas in more mature brains reorganization of existing systems seems to be the current accepted hypothesis within the expanding knowledge of neuroplasticity.97–100 For complex behavior, such as in motor functioning requiring many steps, the limbic network, cortex, hypothalamus, basal ganglia, and brain stem work as an integrated unit, with any damaged area causing the whole system to initially malfunction. Without change or encouragement of appropriate external and internal environmental changes that will create neuroplasticity, the initial malfunction can become permanent.101 The timing for optimal neuroplasticity has not yet been established. The medical use of drugs to alter cellular activity and plasticity after CNS damage has become a huge pharmaceutical research area (see Chapter 36). Early as well as later drug therapy may encourage neuroplasticity.102–108 The same questions must be asked about early instead of later rehabilitation intervention, as well as the limbic influence over the motor system. A loss of function or a change in behavior cannot necessarily be localized as to the underlying cause. A lesion in one area may cause secondary dysfunction of a different area that is not actually damaged. Strub and Black109 view behavior as occurring on distinct interrelated levels that represent behavioral hierarchies. Starting at level 1, a state of alertness to the internal and external environment must be maintained for motor or mental activity to occur. The brain stem reticular activating system brings about this state of general arousal by relaying in an ascending pathway to the thalamus, the limbic network, and the cerebral cortex. To proceed from a state of general arousal to one of “selective attention” requires the communication of information to and from the cortex, the thalamus, and the limbic network and its modulation over the brain stem and spinal pattern generators.56,110 On level 3 only cerebral cortical areas are activated. This level deals with abstract conceptualization of verbal or quantitative entities. It is at this level that the somatosensory and frontal motor cortices work together to perceptually and procedurally develop motor programs. The prefrontal areas of the frontal lobe can influence the development of these motor programs, thus again illustrating the limbic influence over the motor system.111,112 Level 4 behavior is concerned with the expression of social aspects of behavior, personality, and lifestyle. Again, the limbic network and its relationship to the frontal lobe are vital. The shift to the World Health Organization International Classification of Functioning, Disability and Health (WHO-ICF) model, which reflects patient-centered therapy, has actualized the critical importance of this level of human behavior.24,28,31,113,114 As Western medicine is unraveling the mysteries behind the neurochemistry of the limbic network58,115–117 and alternative medicine is establishing effectiveness and efficacy for various interventions and philosophies (see Chapter 39), a fifth level of limbic function may become the link between the hard science of today and the unexplained mysteries. Those medical mysteries would be defined as unexplained yet identified events that have either been forgotten or been hidden from the world by those scientists—mysteries such as why some people heal from terminal illnesses spontaneously, various others heal in ways not accepted by traditional medicine,60,118 and still others just die without any known disease or pathological condition.119–122 One critical component everyone identifies as part of that unexplained healing is a belief by the client that he or she will heal. That belief has a strong emotional component,120 and that may be the fifth level of limbic function. How conscious intent drives hypothalamic autoimmune function is being unraveled scientifically, and clinicians often observe these changes in their patients. Through observation it becomes apparent that clients who believe they will get better often do, and those who believe they will not generally do not. Whether belief comes from a religious, spiritual, or hard science paradigm, that belief drives behavior, and that drive has a large limbic component. Moore123 eloquently describes the limbic network as the area of the brain that moves us. The word MOVE can be used as a mnemonic for the functions of the limbic network. Memory: attention and retrieval, declarative learning Motivation: desire to learn, try, or benefit from the external environment Olfaction (especially in infants) Only sensory system that does not have to go through the thalamus as a second-order synapse in the sensory pathway before it gets to the cerebral cortex Visceral (drives: thirst, hunger, and temperature regulation; endocrine functions) Sympathetic and parasympathetic reactions Hypothalamic regulation over autoimmune system Peripheral autonomic nervous system (ANS) responses that reflect limbic function Emotion: feelings and attitude As seen in this outline, the M (memory, motivation) depicts the drive component of the limbic network. Before learning, an individual must be motivated to learn, to try to succeed at the task, to solve the problem, or to benefit from the environment. Without motivation the brain will not orient itself to the problem and learn. Motivation drives both our cortical structures to develop higher cognitive associations and the motor system to develop procedures or motor programs that will enable us to perform movement with the least energy expenditure and the most efficient patterns available. Once motivated, the individual must be able to pay attention and process the sequential and simultaneous nature of the component parts to be learned, as well as the whole. Thus there is an interlocking dependence among somatosensory mapping of the functional skills124 (cognitive), attention (limbic) necessary for any type of learning, and the sequential, multiple, and simultaneous programming of functional movement (motor). The limbic amygdala and hippocampal structures and their intricate circuitries play a key role in the declarative aspect of memory.125–128 Once this syntactical, intellectual memory is learned and taken out of short-term memory by passing through limbic nuclei, the information is stored in cortical areas and can be retrieved at a later time without limbic involvement.129 The O refers to olfaction, or the incoming sense of smell, which exerts a strong influence on alertness and drive. This is clearly illustrated by the billions of dollars spent annually on perfumes, deodorants, mouthwashes, and soap as well as scents used in stores to increase customers’ desires to purchase. This input tract can be used effectively by therapists who have clients with CNS lesions such as internal capsule and thalamic involvement. The olfactory system synapses within the olfactory bulb and then with the limbic structures and then may go directly to the cerebral cortex without synapsing in the thalamus. Although collaterals do project to the thalamus, unlike all other sensory information, olfaction does not need to use the thalamus as a necessary relay center to access the cortical structures, although many collaterals also project there.56,130 Other senses may not be reaching the cortical levels, and the client may have a sensory-deprived environment. Olfactory sensations, which enter the limbic network, may be used to calm or arouse the client. The specific olfactory input may determine whether the person remains calm or emotionally aroused.131,132 Pleasant odors would be preferable to most people. With the limbic network’s influence on tone production through brain stem modulation, this is one reason aromatherapy causes relaxation and is used by many massage therapists. A comatose, seemingly nonresponsive client may respond to or be highly sensitive to odor.133 The therapist needs to be acutely aware of the responses of these patients because these responses may be autonomic instead of somatomotor and may be reflected in a higher heart rate or an increase in blood pressure. Using noxious stimuli to try to “wake up” a patient in a vegetative state has the possibility of causing negative arousal, fear, withdrawal, or anxiety and an increase in base tone within the motor generators.132 Using this type of input places the patient at level 2 in a “protective state of survival.” Using a pleasant and personal desirable smell will more likely place a client at level 2 “safety.” The former can lead to strong emotions such as anger, whereas the latter often leads to bonding and motivation to learn. Research has shown that retrieval processing and retrieval of memory have a distinctive emotionality when they are linked to odor-evoked memories.134–136 The V represents visceral or autonomic drives. As noted earlier, the hypothalamus is nestled within the limbic network. Thus, regulation of sympathetic and parasympathetic reactions, both of the internal organ systems and the periphery, reflects continuing limbic activity. Obviously, drives such as thirst, hunger, temperature regulation, and sexuality are controlled by this system. Clients demonstrating total lack of inhibitory control over eating or drinking or manifesting very unstable body temperature regulation may be exhibiting signs of hypothalamic-pituitary involvement or direct pathways from hypothalamus to midbrain structures.56 Today, this interaction of the hypothalamus with motor neurons that change or support movement has clearly been established.137 If the sensory input to the client is excessive whether through internal or external feedback, the limbic network may go into an alert, protective mode and will not function at the optimal level, and learning will diminish. The client may withdraw physically or mentally, lose focus or attention, decrease motivation, and become frustrated or even angry. The overload on the reticular system may be the reason for the shutdown of the limbic network and not the limbic network itself. Both are part of the same neuroloop circuitry. All these behaviors may be expressed within the hypothalamic-autonomic system as motor output, no matter where in the loop the dysfunction occurs. Having a functional understanding of the neuroanatomy and their relationships with each other helps therapists unravel some of the mysteries patients present after CNS insult.138,139 The evaluation of this system seems even more critical when a client’s motor control system is locked, with no volitional movement present. Therapists often try to increase motor activity through sensory input; however, they must cautiously avoid indiscriminately bombarding the sensory systems. The limbic network may demonstrate overload while at the same time the spinal motor generators reflect inadequate activation. How a therapist might assess this overload would be to closely monitor the ANS’s responses such as blood pressure, heart rate, internal temperature, and sweating versus observing or measuring muscle tone. Although the somatosensory system and the ANS are different, they are intricately connected. The concept of massively bombarding one system while ignoring the other does not make sense in any learning paradigm, especially from a systems model in which consensus creates the observed behavior. To illustrate this concept, think of an orchestra leader conducting a symphony. It would make no sense for the conductor to ask the string section to play louder if half the brass section got sick. Instead, the conductor would need to quiet the string section and all other sections to allow the brass component to be heard. E relates to emotions, the feelings, attitudes, and beliefs that are unique to that individual. These beliefs include psychosocial attitudes and prejudices, ethnic upbringing, cultural experiences, religious convictions, and concepts of spirituality.120 All these aspects of emotions link especially to the amygdaloid complex of the limbic network and orbitofrontal activity within the frontal lobe.140–142 This is a primary emotional center, and it regulates not only our self-concept but our attitudes and opinions toward our external environment and the people within it. To appreciate the sensory system’s influential interaction with the limbic network directly, the reader need only look at the literature on music and how it interacts with emotions.143,144 Most people can give examples of instances where music has elicited immediate and compelling emotional responses of various types. Pleasant and unpleasant musical stimuli have been found to increase or decrease limbic activity and influence both cognitive and motor responses. Although the neurological mechanisms are not yet well understood, the limbic network seems to be implicated in both “positive” and “negative” emotions in response to musical stimuli.145–148 The clinical implications are huge. Excessive noise, loudspeaker announcements, piped in music, and all the therapists’ voices can affect the CNS of a client. These responses can be highly emotional, cause changes in visceral behavior, and affect striated motor expression. Level of musical consonance or dissonance is just one element of the auditory stimulus that is subjectively experienced by the listener as pleasant or unpleasant. The implications not only that listening to music affects limbic emotional states but that the influence may direct the hypothalamus in regulation of blood flow within the CNS have also been shown.148 With music or sound being just one input system, the therapist must realize that sensory influence from smell, taste, touch, proprioception, and vestibular and organ system dysfunction can lead to potential limbic involvement in all aspects of CNS function and directly affect the emotional stability of the patient. A second self-concept deals with my attitude about my worth or value to society and the world and my role within it.149 Again, this attitude can change with mood, but more often it seems to change with experience. This aspect of client-therapist interaction can be critical to the success of a therapeutic environment. The two following examples illustrate this point, with the focus of bringing perceived roles into the therapeutic setting: Your client is Mrs. S., a 72-year-old woman with a left cerebrovascular accident (CVA). She comes from a low socioeconomic background and was a housekeeper for 40 years for a wealthy family of high social standing. When addressing you (the therapist), she always says “yes, ma’am” or “no, ma’am” and does just what is asked, no more and no less. It may be very hard to empower this client to assume responsibility for self-direction in the therapeutic setting. Her perceived role in life may not be to take responsibility or authority within a setting that may, from her perception, have high social status, such as a medical facility. She also may feel that she does not have the right or the power to assume such responsibilities. Success in the therapeutic setting may be based more on changing her attitudes than on her potential to relearn motor control. That is, the concept of empowerment may play a crucial role in regaining independent functional skill and control over her environment.24,28,31,150–153 Your client is a 24-year-old lumberjack who sustained a closed-head injury during a fall at work. It is now 1 month since his accident, and he is alert, verbal, and angry and has moderate to severe motor control problems. During your initial treatment you note that he responds very well to handling. He seems to flow with your movement, and with your assistance is able to practice a much higher level of motor control within a narrow biomechanical window; although at times he needs your assistance, you release that control whenever possible to empower him to control his body. At the end of therapy he sits back in his chair with much better residual motor function. Then he turns to you (the female therapist) and instead of saying, “That was great,” he says, “You witch, I hate you.” The inconsistency between how his body responded to your handling and his attitude toward you as a person may seem baffling until you realize that he has always perceived himself as a dominant male. Similarly, he perceives women as weak, to be protected, and in need of control. If his attitude toward you cannot be changed to see you in a generic professional role, he will most likely not benefit as much from your clinical skills and guidance as a teacher. Before the accident the patient may have suppressed that verbal response but not tone and body language. After a traumatic brain injury affecting the orbitofrontal system, the inhibition of the behavioral response itself may be lost, further embarrassing the patient emotionally. Preconceived attitudes, social behaviors, and opinions have been learned by filtering the input through the limbic network. If new attitudes and behaviors need to be learned after a neurological insult, the status of the amygdaloid pathways seems crucial. Damage to these limbic structures may prevent learning154; thus, socially maladaptive behavior may persist, making the individual less likely to adapt to the social environment. It is often harder to change learned social behaviors than any other type of learning.155–158 Because our feelings, attitudes, values, and beliefs drive our behaviors through both attention and motor responses, the emotional aspect of the limbic network has great impact on our learning and motor control. If a patient is not motivated and places little value on a motor output, then complacency results and little learning will occur.159–161 On the other hand, if a therapist places an extremely high value on a motor output as a pure expression of motor control without interlocking that control with the patient’s limbic influence, the behavioral response may lead to inconsistency, lack of compliance, and thus lack of motor learning and carryover.159 Similarly, it can cause extreme stress, which even the general public knows causes disease.162 Moore123 considers motivation and memory as part of the MOVE system. Esch and Stefano163 link motivation with reward and help, illustrating how the limbic network learns through repetition and reward. They state that the concept of motivation includes drive and satiation, goal-directed behavior, and incentive. They recognize that these behaviors maintain homeostasis and ensure the survival of the individual and the species. Although the frontal lobe region appears to play an important role in self-control and execution activities, these functions seem to require a close interlocking neuronetwork between cognitive representation within the frontal regions and motivational control provided by limbic and subcortical structures.140,164 An important aspect of motivated behavior is linked to patient- and family-centered therapy.* “The most powerful force in rehabilitation is motivation.”167 These words are strong and reflect the importance of the limbic network in rehabilitation. Motivated behavior is geared toward reinforcement and reward, which are based on both internal and external feedback systems. Repeated experience of reinforcement and reward leads to learning, changed expectancy, changed behavior, and maintained performance.168 Emotional learning, which certainly involves the limbic network, is very hard to unlearn once the behavior has been reinforced over and over.169,170 For that reason, motor behavior that is strongly linked to a negative emotional response might be a very difficult behavior to unlearn. For example, a patient who is willing to stand up and practice transfers just to get the therapist off his back is eliciting a movement sequence that is based on frustration or anger. When that same patient gets home and his spouse asks him to perform the same motor behavior, he may not be able to be successful. The spouse may say, “The therapist said you could.” The patient may respond, “I never did like him!” Thus repetition of motor performance with either the feeling of emotional neutrality or the feeling of success (positive reinforcement) is a critical element in the therapeutic setting. Consistently making the motor task more difficult just when the client feels ready to succeed will tend to decrease positive reinforcement or reward, lessen the client’s motivation to try, and decrease the probability of true independence once the patient leaves the clinical setting. When pressure is placed on therapists to produce changes quickly, repetition and thus long-term learning are often jeopardized, which may have a dramatic effect on the quality of the client’s life and the long-term treatment effects once he or she leaves the medical facility. Motor control theory (see Chapter 4) coincides with limbic research regarding reinforcement. Inherent feedback within a variety of environmental contexts allowing for error with correction leads to greater retention.171 Repetition or the opportunity to practice a task (motor or cognitive) in which the individual desires to succeed will lead to long-term learning.172 Without practice or motivation the chance of successful motor learning is minimal to nonexistent. Positive emotional states may create a limbic environment in which the therapist can link reward and pleasure associations to new motor sequences. Although it is well known that appropriate selections of music can stimulate states of highly pleasant positive affects and physical relaxation, the neurological mechanisms for these effects are not well understood. In an early study by Goldstein173a subjects reported pleasant physical sensations of tingling or “thrills” in response to music listening. After subjects were injected with naloxone, which blocks opiate receptors, thrill scores and tingling sensations were attenuated in some subjects. Although responses to music are highly individualized and this study has not been replicated, it suggests that endorphins may be released under certain music listening conditions that elicit pleasant physical sensations. In a positron emission tomography (PET) study of cerebral blood flow (CBF) changes measured during highly pleasurable “shivers or chills” in response to subject-selected music, Blood and colleagues147 found that as the intensity of the chills increased, CBF increases occurred in the left ventral striatum, dorsomedial midbrain, bilateral insula, right orbitofrontal cortex, thalamus, anterior cingulate cortex, supplementary motor area, and bilateral cerebellum. As the intensity of chills increased, significant CBF decreases were also observed in the right amygdala, left hippocampus and amygdala, and ventral medial prefrontal cortex. The increases found in brain structures associated with reward or pleasant emotions and decreases in areas associated with negative emotional states suggest that music (1) must be carefully selected according to individual preferences and responses, in order to reliably elicit such highly pleasurable experiences as “shivers down the spine” and (2) might be used therapeutically to positively affect limbic activity. Other studies provide additional support for the notion that music may activate limbic and paralimbic areas associated with reward or pleasurable emotions. Brown and colleagues145 conducted a PET study of 10 nonmusicians who listened passively to unfamiliar music, which they later reported had elicited strongly pleasant feelings. Unlike previous studies of music, emotion, and limbic activity, this research design called for subjects to listen passively without engaging in any task such as evaluating affective components during the music. The authors noted that the music stimuli used was musically complex and strongly liked by the subjects. When the CBF during the music was compared with silent rest conditions in the same subjects, activations were seen, as expected, in areas presumed to represent perceptual and cognitive responses to music (primary auditory cortex, auditory association cortex, superior temporal sulcus bilaterally, temporal gyrus of the right hemisphere, in the right superior temporal pole, and adjacent insula). In addition, responses were found in limbic and paralimbic areas, which included the left subcallosal cingulate, the anterior cingulate, left retrosplenial cortex and right hippocampus, and the left nucleus accumbens and cerebellum. The researchers compared these results with those from the earlier studies by members of the same team147,148 and suggest that areas such as the subcallosal cingulate are related to the direct experience of occurrent emotions rather than discriminate processing for emotion and that different areas are specifically activated during the pleasant physical responses known as “chills.” They go on to propose that the superior temporal pole and adjacent insula may serve as a point of bifurcation in neural circuitry for processing music. They also suggest that neurons from that region project to limbic and paralimbic areas involved in emotional processing and to premotor areas possibly involved in discrimination and structural processing of music. Although research has increased our appreciation of the complexity of brain activation by music, much more study is needed to validate a model of limbic network activity in human emotional responses to musical stimuli. Clinically, music can be used to improve mood and increase patient motivation to participate in rehabilitation treatment. Case studies174,175 suggest that music can be used to decrease crying by infants and toddlers during physical therapy treatment. West has participated in both developmental and rehabilitation settings as a music therapist in co-treatment with physical and occupational therapists. The music therapist first does a thorough assessment of the individual’s preferences and responses to music, then provides music selected or composed specifically to provide motivating energy, pleasant associations, and positive affective states to accompany the motor activity. This individualized, live-music approach allows the music therapist to modify the musical elements as needed in the moment, working in a real-time limbic partnership with both the client and the physical or occupational therapist. Music or pleasure sounds can be used to help neutralize or balance the limbic influence on motor expression. Obtaining a limbic-neutral impact is critical before evaluating functional movement in order to accurately determine true motor system involvement. Many types of emotions create motivation, such as pleasure, reward processes, emotions associated with addiction, appreciation of financial benefits, amusement, sadness, humor, happiness, and depression.163,173b,176–179 Some emotions tend to drive learning, whereas others may discourage learning, whether that learning be cognitive or motor. Motivation, alertness, and concentration are critical in motor learning because they determine how well we pay attention to the learning and execution of any motor task. These processes of learning and doing are inevitably intertwined: “We learn as we do, and we do only as well as we have learned.”180 Both motivation (“feeling the need to act”) and concentration (“ability to focus on the task”) are interlinked with the limbic network. The amygdaloid complex with its multitude of afferent and efferent interlinkages is specially adapted for recognizing the significance of a stimulus, and it assigns the emotional aspect of feeling the need to act. These neuroanatomical loops have tremendous connections with the reticular system. Hence, some authors call it the reticulolimbic network.56,157 The interaction of the limbic network and the motor generators of the brain stem and ultimate direct and indirect modulation over the spinal system lead to need-directed and therefore goal-directed motor activity. It also filters out significant from insignificant information by selective processing and storing the significant for memory, learning, and recall. These interconnected neuroloop circuitries reinforce the concept that areas have both specialization and generalization and thus work closely together with other areas of the brain.169,181 Goal-directed or need-directed motor actions are the result of the nervous system structures acting as an interactive system. Within this system (Figure 5-4), all components share responsibilities. The limbic network and its cortical and subcortical components represent the most important level. In response to stimuli from the internal or external environment, the limbic network initiates motor activity out of the emotional aspect of feeling the need to act. This message is relayed to the sensory areas of the cerebral cortex, which could entail any one or all association areas for visual, auditory, olfactory, gustatory, tactile, or proprioceptive input. These areas are located in the prefrontal, occipital, parietal, and temporal lobes, where they analyze and integrate sensory input into an overall strategy of action or a general plan that meets the requirements of the task. Therefore these cortices recognize, select, and prepare to act as a response to relevant sensory cues when a state of arousal is provided by reticular input. The limbic cortex (uncus, parahippocampal gyrus /isthmus, cingulate gyrus, and septal nucleus) has even greater influence over the sensorimotor cortices through the cingulate gyrus, both directly and indirectly through association areas.182–184 The thalamus, cerebellum, and basal ganglia contribute to the production of the specific motor plans. These messages of the general plan are relayed to the projection system. The limbic structures through the cingulate gyrus also have direct connections with the primary motor cortex. These circuits certainly have the potential to assist in driving fine motor activities through corticobulbar and corticospinal tract interactions. The thalamus, cerebellum, basal ganglia, and motor cortices (premotor, supplementary motor, and primary motor) contribute to the production of the specific motor plans.56 Messages regarding the sensory component of the general plan are relayed to the projection system, where they are transformed into refined motor programs. These plans are then projected throughout the motor system to modulate motor generators throughout the brain stem and spinal system.56 Limbic connections with (1) the cerebellum, basal ganglia, and frontal lobe56,185–189 and (2) the motor generator within the brain stem enable further control of limbic instructions over motor control or expression. If the limbic and the cognitive systems decide not to act, goal-driven motor behavior will cease. An individual’s belief (emotional and spiritual) can inhibit even the most basic survival skills, as has been clearly shown in history when individuals with particular religious beliefs were pitted against vicious predators and those people chose not to defend themselves. Within the projection system and motor planning complexes, the specifics are programmed and the tactics are given a strategy. In general, “what” is turned into “how” and “when.” The necessary parameters for coordinated movement are programmed within the motor complex as to intensity, sequencing, and timing to carry out the motor task. These programs, which incorporate upper motor neurons and interneurons, are then sent to the brain stem and spinal motor generators, which in turn, through lower motor neurons, send orders regarding the specific motor tasks to the musculoskeletal system. (See Chapters 3, 4, and 8 for more specific in-depth discussion.) The actions performed by each subsystem within the entire limbic–motor control complex constantly loop back and communicate to all subsystems to allow for adjustments of intensity and duration and to determine whether the plan remains the best choice of responses to an ever-changing three-dimensional world.138,186,187 The limbic network has one more opportunity to modify and control the central pattern generators and control the body and limbs through direct connections to the spinal neuronetwork.110,190–193 That is, the limbic network can alter existing motor plans by modulating those generators up and down or altering specific nuclear clusters and varying the patterns themselves. Therapists as well as the general public see this in sports activities when emotions are high, no matter the emotion itself. Individuals who have excellent motor control over a specific sport may find high-level performance difficult as the stress of competition increases. Having control over emotional variance as well as motor variance with a functional activity is an accurate example of empowerment. Thus, for a therapist to get a true picture of a patient’s motor system’s function, the limbic network should be flowing in a neutral or balanced state without strong emotions of any kind. Generally, that balance seems to reflect itself in a state of safety, trust, and compliance. Once the motor control has been achieved then the therapist must reintroduce various emotional environments during the motor activity to be able to state that the patient is independent. In summary, the limbic complex generates need-directed motor activity and communicates that intent throughout the motor system.110,191,194,l95 This step is vital to normal motor function and thus client care. Clients need the opportunity to analyze correctly both their internal environment (their present and feed-forward motor plans and their emotional state) and the external world around them requiring action on a task. The integration of all this information should produce the most appropriate strategy available to the patient for the current activity. These instructions must be correct, and the system capable of carrying out the motor activity, for effortless, coordinated movement expression to be observed. If the motor system is deficient, lack of adaptability will be observed in the client. If the limbic complex is faulty, the same motor deficits might present themselves. The therapist must differentiate what is truly a motor system problem versus a limbic influence over the motor system problem. Schmidt196 stresses the significance of “knowledge of results feedback” as being the information from the environment that provides the individual with insights into task requirements. This insight helps the motor system correctly select strategies that will successfully initiate and support the appropriate movement for accomplishing the task. This knowledge of results feedback is required for effective motor learning and for forming the correct motor programs for storage.197,198 Brooks69 distinguishes insightful learning, which is programmed and leads to skills when the performer has gained insight into the requirements, from discontinuous movements, which need to be replaced by continuous ones. This process is hastened when clients understand and can demonstrate their understanding of what “they were expected to do.” Improvement of motor skills is possible by using programmed movement in goal-directed behavior. The reader must be cautioned to make sure that the client’s attention is on the goal of the task and not on the components of the movement itself. The motor plan needs programming and practice without constant cognitive overriding. The limbic/frontal system helps drive the motor toward the identified task or abstract representation of a match between the motor planning sequence and the desired outcome. The importance of the goal being self-driven by the patient cannot be overemphasized.* Without knowledge of results, feedback, and insight into the requirements for goal-directed activity, the learning is performing by “rote,” which merely uses repetition without analysis, and meaningful learning or building of effective motor memory in the form of motor holograms will be minimal. Children with cognitive and limbic deficits can learn basic motor skills through repetition of practice, but the insights and ability to transfer that motor learning into other contexts will not be high (see Chapters 12, 13, and 14). Schmidt196 suggests that to elicit the highest level of function within the motor system and to enable insightful learning, therapy programs should be developed around goal-directed activities, which means a strong emotional context. These activities direct the client to analyze the environmental requirements (both internal and external) by placing the client in a situation that forces development of “appropriate strategies.” Goal-directed activities should be functional and thus involve motivation, meaningfulness, and selective attention. Functional and somatosensory retraining uses these concepts as part of the intervention (see Chapters 4 and 9). Specific techniques such as proprioceptive neuromuscular facilitation, neurodevelopmental therapy, the Rood method, and the Feldenkrais method can be incorporated into goal-directed activities in the therapy programs, as can any treatment approach, as long as it identifies those aspects of motor control and learning that lead to retention and future performance and allows the patient to self-correct.196 With insights into the learned skills, clients will be better able to adjust these to meet the specific requirements of different environments and needs, using knowledge of response feedback to guide them. The message then is to design exercise activities or programs that are meaningful and need directed, to motivate clients into insightful goal-directed learning. Thus, understanding the specific goals of the client, patient-centered learning, is critical and will be obtained only by interaction with that client as a person with needs, desires, and anticipated outcomes.201,202 A therapist cannot assume that “someone wants to do something.” The goal of running a bank may seem very different from that of birdwatching in the mountains, yet both may require ambulatory skills. If a client does not wish to return to work, then a friendly smile and the statement, “Hi, I’m your therapist and I’m going to get you up and walking so you can get back to work,” may lead to resistance and decreased motivation. In contrast, a therapist who knows the goal of the client may help him or her become highly motivated to ambulate; that client may be present in the clinic every day to meet the goal of birdwatching in the mountains although never wishing to walk back into the office again.
The limbic system: influence over motor control and learning
The functional relationship of the limbic network to clinical performance
The limbic network’s role in motor control, memory, and learning
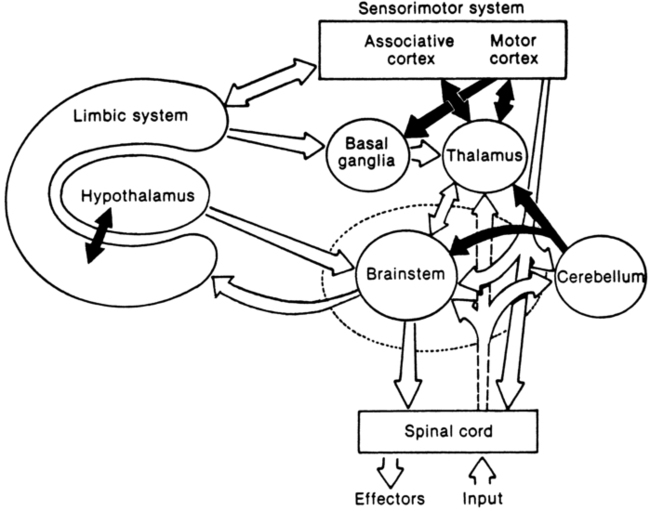
 Divisions and interconnections between the limbic and nonlimbic cortices (sensory and motor areas).
Divisions and interconnections between the limbic and nonlimbic cortices (sensory and motor areas).
The limbic network’s influence on behavior: its relevance to the therapeutic environment
Levels of behavioral hierarchies: where does the limbic network belong?
The limbic network moves us
Limbic network function.
Motivation and reward.
Integration of the limbic network as part of a whole functioning brain
Clinical perspectives
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The limbic system: influence over motor control and learning
Only gold members can continue reading. Log In or Register to continue