Athletes find they need to stretch the calf muscles before and particularly after activity for around 30 seconds, repeated three times, once a day (Bandy et al. 1997) and maintain dorsiflexion, although stretching before and after exercise has not been shown to necessarily reduce risk of injury (Herbert and Gabriel 2002). Shoe type selection is difficult as there needs to be support to counter the impact and flexibility to allow some compensatory movement (Orendurff et al. 2008).
Flat flexible feet (Figure 23.2)
Again primarily inherent, this foot type requires shoe selection to provide motion control to avoid stress on structures in some activities, but allow enough movement to tolerate longer contact impact in others (Chuckpalwong et al. 2008).
Injuries caused by either overuse or as a result of a structural non-conformity to the sport are similar in that only through significant activity do pre-existing or underlying structural problems usually reveal themselves. The development of an extremely wide choice of shoes, insoles and orthoses means there is the potential to influence the right compensatory combination to reduce injury potential, but also increases the need for more experience and knowledge of sport specifics, shoe construction and supplemental biomechanical device prescription.
Foot injuries can be divided into three anatomical and structural areas:
1. rearfoot
2. midfoot
3. forefoot.
Injuries to the rearfoot
Plantar fasciitis
Buchbinder (2004) maintains plantar fasciitis is not only the most common cause of pain in the inferior heel, but is responsible for approximately 10% of all running related injuries. Plantar fasciitis is inflammation of the plantar fascia, which may radiate into the arch of the foot aggravated by weight bearing and propulsive activity. It is an overuse injury usually causing plantar proximal and medial pain which may radiate distally to the mid-arch. A strain or sometimes rupture with either gradual or sudden overload is quite common, especially in the active sport population.
Plantar fasciitis can be related to a ‘heel spur’, which is a bony exostosis at the attachment of the plantar fascia to the calcaneus. A heel spur is believed to be caused by repetitive stress from the plantar fascia attachment and can be present on the asymptomatic foot; or a painful heel may have no heel spur (Ryan 2007).
Predisposing factors also include: increased body weight, pronation and/or ankle eversion, prolonged periods of standing, reduced ankle dorsiflexion, and high arches. In sport it is often associated with harder training surfaces or increased intensity or duration of training (Huerta et al. 2008).
The lateral plantar nerve passes through the tarsal tunnel between the abductor hallucis muscle and the quadratus planus muscle. It may become compressed causing similar pain under the heel, and sometimes up towards the medial ankle.
Treatment and rehabilitation
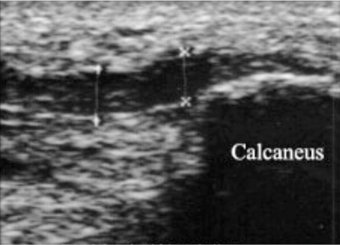
Rest including unloading the foot with supportive taping, and even crutches in the early stages, is essential (Cole et al. 2005). A night splint to hold the foot stretched into dorsiflexion can reduce the overnight tendency to tighten (Figure 23.3). Manual tissue release techniques and needling can be effective to reduce tension in the usually tight tissue. Ultrasound guided (Figure 23.4) needle fasciotomy is a relatively new minimally invasive procedure where a needle is inserted into the plantar fascia to possibly disrupt the fibrous tissue that forms as a result of the chronic inflammation.
A gradual return to loading with incremental strengthening and rehabilitation can be frustrating for the athlete as it may take several weeks to strengthen. Many coaches have found movement drills in sandpits to be beneficial and preventative. After biomechanical evaluation, insoles or orthotics may help reduce stress, but may be too compressive during the acute phase. Injection may be helpful short term (Selman 1994) but must be combined with stretching and biomechanical influence to prevent recurrence. Extracorporeal shock therapy, inducing significant vibratory impact directly to the area, has conflicting research evidence (Buchbinder 2002; Sems et al. 2006).
Heel contusion
Repetitive impact on the heel can cause the fat pad that protects the calcaneus to be pushed up the side of the heel leaving less of a protective layer. Sometimes called ‘policeman’s heel’ it is common in sport requiring repetitive impact on the heel like the hopping foot in triple jump. If managed early it should recover within a few days. If not, and it becomes chronic, it can be a long recovery as continued weight bearing tends to sustain the injury. This is considered to be related to a bursa between the calcaneum and the fat pad (Irving et al. 2007).
Treatment and rehabilitation
Insoles are more effective than heel pads as they dissipate rather than concentrate pressure; plus pads raising the heel without supporting the arch, destabilise the foot, increasing stress on the arch (Gosky et al. 2006). This is particularly important for high arched feet where an unsupported arch leaves the heel and forefoot exposed to more impact stress. Taping the heel can compress the soft tissue under the heel during activity, providing increased protection (Hyland et al. 2006).
Calcaneal stress fracture
A stress fracture can occur in the calcaneum as a result of cumulative impact. It is common in sports like long distance running (Fredricson et al. 2006), particularly with athletes who predominantly heel strike rather than mid to forefoot strike, which tends to be the heavier jogger or slower running athlete. The majority of plantar heel pain is probably diagnosed as plantar fasciitis or as heel spurs. When the history or examination findings are atypical or when routine treatment is ineffective, consideration should be given to atypical causes of heel pain (Webber et al. 2005). Stress fractures of the calcaneus are possibly a frequently unrecognised source of heel pain. In some cases they can continue to go unrecognised because the symptoms of calcaneal stress fracture sometimes improve with treatments aimed at soft tissue injuries. Calcaneal stress fractures can occur in any population of adults and are common among active people, such as running athletes. It is very likely that the incidence of diagnosed calcaneal stress fractures will rise with an increased consideration of their possibility. Commonly (Webber et al. 2005) there is an insidious, gradual onset pain, made worse by weight bearing. Pain is reproduced by squeezing the back of the heel from both sides. X-ray will frequently not show any sign of fracture at all, or until after approximately two weeks.
Treatment and rehabilitation
A stress fracture should be suspected if there is inactive or night pain, and requires rest from impact for 6–8 weeks, often including crutches in the early stages (McRae and Esser 2008). Return to sporting impact must be gradual. Ideally starting with minimal heel weight bearing activities, like hydrotherapy, cycling and rowing; progressing to elliptical trainer and treadmill intervals before running. Conversely it may be more appropriate to run quicker intervals on toes rather than slower runs with more heel impact initially. Appropriate shoes with insoles or orthotics to dissipate impact are advisable.
Nerve entrapment
This can be described as ‘tarsal tunnel syndrome’ or ‘medial calcaneal nerve entrapment’. The two conditions are similar with variable symptoms of pain that can be in the heel, toes or the arch of the foot, and numbness and/or pins and needles may be felt in the sole of the foot. There is usually pain when standing and more when running. ‘Tinel’s test’, tapping the nerve just behind the medial malleolus, is uncomfortably sensitive. Ankle eversion and foot pronation appear to stress and irritate the medial and lateral plantar nerves, causing the ‘tarsal tunnel syndrome’ variation (Kinoshita et al. 2006).
Treatment and rehabilitation
Slow controlled non weight-bearing exercise progressing to weight bearing in positions that do not aggravate; passive mobilisation and manipulation, cryotherapy (ice treatment) or transcutaneous electrical nerve stimulation (TENS) which may reduce sensitivity. Insoles or orthotics to alter the mechanical loading pattern are sometimes beneficial (DiDomenico and Masternick 2006). However, when conservative measures are not successful, surgical decompression (Mullick and Dellon 2008) or excision may result in relief of pain, fortunately with few potential complications
Sever’s disease
This condition which is sometimes called calcaneal apophysitis occurs primarily in active children around the age of 9–14 years (Malanga and Ramirez-Del Toro 2008). Although opinion and poorly conducted retrospective case series make up the majority of evidence on this condition, (Scharfbillig et al. 2008) it is usually associated with a rapid growth spurt combined with repetitive weight bearing, propulsive and braking activity and tight calf muscles. Athletes typically complain of heel pain or soreness that improves with rest and increases with running. There is usually tenderness at the back of the heels, especially if you press in or give it a squeeze from the sides.
Treatment and rehabilitation
Rest from impact and propulsion usually resolves the condition, but this may be slow when the growth of the calcaneum is active. Use of a brace or cast does help, probably by inhibiting activity as well as weight bearing. A biomechanical assessment may indicate potential reasons for increased stress on the heel, which if reduced by insoles or orthoses, may assist recovery (Hendrix 2005). The most consistent difference between normal and Sever’s patients is related to the more fragmented nature of the symptomatic epiphysis, which may suggest a mechanical etiology for that condition (Volpon and de Carvalho Filho 2002). Modified types of training with less impact are therefore usually necessary for prevention or resolution.
Retrocalcaneal bursitis and Haglund’s deformity (Figure 23.5)
Pain at the back of the heel caused by an inflamed bursa which is situated between the Achilles tendon and the calcaneum (Haglund 1972). This is a common condition in athletes, particularly in running related sports, and is often associated with Achilles tendinopathy. A MRI study on Achilles tendonopathy enthesitis found retrocalcaneal bursitis in three-quarters of cases (D’Agostini and Olivieri 2006). The key to successful management is a proper understanding of the anatomy and pathological processes (Solan and Davies 2007). Sensitivity and swelling are especially aggravated when running uphill or on uneven surfaces. Wearing particular shoes that put pressure on the area can aggravate the condition, as can pivoting on the heel when driving.
A bony growth or exostosis can develop at the posterior calcaneum called ‘Haglund’s deformity’. If conservative management fails then surgery may be necessary to repair the Achilles tendon and reduce the exostosis (Stephens 1994).
Treatment and rehabilitation
Insoles or orthotics to alter the calcaneal alignment can reduce irritation from the side of the Achilles that may be causing avulsion stress, as well as diminish pressure and movement that may be causing frictional irritation (Heneghan and Pavlov 1984). Anti-inflammatory medication orally and even topically, as part of the inflammation is superficial, with protective dressing, usually assists recovery, however, injection or even surgery are used in persistent cases.
Achilles tendinopathy (Figure 23.6)
The Achilles tendon may be damaged and inflamed primarily through overloading during the propulsive phase of the gait cycle. It can be injured cumulatively with overtraining without sufficient recovery, or suddenly, for example by increased quality of training on a harder surface (Paavola et al. 2002). It is estimated that it may account for about 10% of all running related pathologies.
The Achilles tendon has a poor blood supply, which is probably why it is slow to recover. Chronic Achilles tendinopathy is a difficult condition to treat because it is difficult to rest, and older athletes tend to be more susceptible.
A primary reason for the pain becoming chronic is that discomfort experienced often reduces significantly with the start of activity. This is probably due to reactive loss of sensitivity, giving the athlete a false impression with pain returning after the activity. A thickening in the tendon, particularly 2–3 cm proximal to the calcaneum may then develop. An extension of the blood supply may develop (Knobloch et al. 2006), which is now considered to be detrimental to recovery. Ohberg and Alfredson (2002) analysed blood flow in painful Achilles tendons and found some evidence that new blood vessels in the tendon were the cause of tendon pain. MRI or ultrasound scans only have moderate correlation with clinical assessment (Khan et al. 2003), indicating accurate assessment is more significant in determining the degree of Achilles pathology and therefore outcome expectation.
Treatment and rehabilitation
Wearing an insole/orthotic (Pope et al. 2009), rather than a heel raise that destabilises, will raise the heel and reduce dorsiflexion and propulsive stress. This should only be temporary during recovery or loss of length and restricted dorsiflexion may occur. Anti-inflammatory medication may assist in the early stages, but it must not be a mechanism just to allow more activity, except in the case of carefully managed rehabilitation exercises like Alfredson’s regime.
Biomechanical causes may be positively influenced by orthotics alongside modifying technique and possibly the training programme. Mobilisation of sub-talar or talo-calcaneal joint eversion may help in improving alignment (Harper 1991) and creating more tolerant stress variability. Taping to support the tendon may assist recovery, and in acute or stubborn cases bracing or a cast can be used initially. Tissue release massage techniques can assist in reducing tightness in the calf complex, especially when the athlete is going through the protective phase (Davidson et al. 1997). Poor clinical evidence supported the use of deep friction massage in a Cochrane review in 2002 showing no obvious benefit, although the reviewers were not evaluating Achilles tendons in particular (Brosseau et al. 2002).
McCrory et al. (1999) concluded that strengthening exercises (see below for specific details) and orthotics to control the degree of rear foot pronation should be utilised for athletes suffering from Achilles tendinopathy. Loss of calcaneal movement, especially eversion, is probably related and needs more research. Corticosteroid injection may be used in chronic situations, however an injection directly into the tendon is not recommended as it may increase the risk of a total rupture. Rehabilitation is essential otherwise the condition is likely to return with increased loading. Wallmann’s (2000) and Alfredson et al. (1998) regimes are now used widely but there is some debate as to whether the exercises are strengthening or reflect a specific stretching programme directed at the structures (Allison and Purdam 2009).
Wallmann’s regime
Starting with a daily 5–10 minute warm-up of gentle cardiovascular exercise, preferably non-weight bearing, such as cycling. This is followed by a basic calf raise exercise using body weight on the floor, progressed by increasing the load and speed of the eccentric lowering.
The exercise should feel hard, but not painful. If the workout feels the same or easier the next day, then increase to level two difficulty on the next day. Progress until the athlete can achieve level five, which may take weeks to months.
Level 1: Straight leg heel raise with the uninjured leg. Then put the toes of the injured leg down and lower both legs slowly over 5 seconds ×10 repetitions ×3 sets with 30 seconds recovery (this remains the same for all the levels).
Increase the lowering speed to 2 seconds, and to 1 second as discomfort allows (this remains the same for all levels).
Progress to 20 degrees bent knee heel raise, to load the Soleus more.
Level 2: Progress to both legs for lowering and raising.
Level 3: Progress to the uninjured leg alone during the raising phase and the injured leg alone lowering.
Level 4: Progress to both legs during the raising phase and the injured leg alone lowering.
Level 5: Finally, lowering and raising only with the injured leg.
Alfredson’s regime (Figure 23.7)
Twice a day for 12 weeks.
Calf raise with the forefoot placed on a step. The athlete shifts body weight pushing up on the uninjured leg and lowers down on the injured leg, slowly and in control, e.g. 5 seconds up and 10 down. Three sets ×15 repetitions of straight-leg calf raise and then the same bent-leg. Progress the eccentric loading by adding weights to a back-pack or a calf-raise resistance machine over the 12 weeks.
Alfredson progresses by increased loading rather than speed and emphasises eccentric lowering through a full range of movement. This means that Wallmann’s regime may be more appropriate for faster, lighter shorter contact, and Alfredson’s more powerful and longer contact progression. There is also current ongoing research between indicating that Wallmann’s exercises in inner range are better for distal enthisopathy, rather than Alfredson’s which have the outer range stretch element. Alfredson’s research compared two groups. One group had surgery, while the other group used the twelve week programme. Both groups were able to return to normal activity afterwards with the same level of pain relief. This strongly indicated that a progressive emphasis on eccentric loading programme is a very effective alternative to surgery.
In summary, if you look after this injury early enough and rehabilitate the tendon properly you should make a good recovery. Investigators have evaluated the close correlation between good clinical results with eccentric training (Niesen-Vertommen et al. 1992) and a marked reduction in neovascularisation of the tendon (Ohberg et al. 2004; Knobloch 2007). Magnussen et al. (2009) found eccentric exercises still have the most evidence of effectiveness in treatment of midportion achilles tendinopathy Evidence for the role of heel pads, heparin injection, and peritendinous steroid injections is weak. As research continues (Almekinders and Temple 1998), newer approaches are being developed including the use of glyceryl trinitrate (GTN) patches (Paoloni et al. 2004) and the direct or indirect transfer of genes for platelet-derived growth factor and other growth factors that modulate responses to healing and promote type I collagen growth in the tendon (Maffulli et al. 2002).
Achilles tendon rupture (Figure 23.8)
Most individuals with Achilles tendon rupture have had prior tendinopathy (Cetti et al. 2003). The Achilles tendon can partially tear or totally rupture. A total rupture is more common in recreational older athletes.
Sometimes occurring following a history of inflammation, the classic description is of a sudden sharp pain with a distinct bang as if something has hit the back of the leg. Surprisingly, there may not be as much subsequent pain as expected. Movement is not as painful due to there not being a connection, and although limping, it is still possible to walk with other lesser plantarflexing muscles. There may be a palpable gap in the tendon usually with significant swelling and a positive result with Thomson’s calf squeeze test resulting in loss of foot plantarflexion (Figure 23.9).
Treatment and rehabilitation
It is recommended that the sooner operated on to suture the ends together; the more chance you have of making a full recovery. The reported surgical success rates in surgery vary between 75–100% (Paavola et al. 2002). Progressive plastering without surgery has been used to good effect but tends not to be advocated as there is evidence of a higher re-rupture rate. However, there is a school of thought that believes the differences in rehabilitation used with the two methods may be significant and more research is needed.
Athletes are usually out of competition for 6–12 months, depending on rehabilitation accuracy, motivation and the type of sport (Maffulli and Ajis 2008). Progressive rehabilitation is essential for maximum recovery. Starting with non- and partial weight-bearing exercise using hydrotherapy, cycling, etc., progressing to weight bearing, propulsive and finally explosive activity (Figure 23.1).
Table 23.1 Achilles rupture rehabilitation guide (copyright Allen JW 2009)
Peroneal tendon injuries
Athletes with peroneal tendon dislocation typically present with acute pain and swelling behind the lateral malleolus (Brandes and Smith 2000). These symptoms are caused by a dorsiflexion-inversion stress injury of the ankle that pulls the peroneal retinaculum off the lateral malleolus (Slater 2007). Athletes usually complain of snapping and sudden sharp pain when changing direction or pushing forward with subsequent loss of eversion strength. Problems arising with the peroneal tendons may be tenosynovitis or tendonopathy. The os perineum, a sesamoid bone that may be present within the peroneus longus tendon at about the level of the calcaneo-cuboid joint, may be involved with the degenerative process or as a singular disorder being fractured or fragmented.
On physical examination, there is usually tenderness to palpation along the course of the peroneal tendons, often with swelling. A provocative test for peroneal pathology is to have the athletes foot hanging in a relaxed position with the knee flexed at 90 degrees. Slight pressure is applied to the peroneal tendons posterior to the fibula. The patient is then asked to dorsiflex and evert the foot against resistance. Pain may be elicited, or the tendons may be felt to sublux.
Treatment and rehabilitation
Treatment depends on the type of peroneal tendon injury. A cast or splint may be used to immobilise the foot and ankle and allow the injury to heal (van Zoest et al. 2007). Oral and topical anti-inflammatory medication may be used to reduce swelling and pain. As symptoms improve, exercises can be added to strengthen the muscles and improve range of motion and particularly balance. A brace may initially be supportive for a short while, or during activities requiring repetitive ankle movement, or may be an option to allow more activity when a patient is not a candidate for surgery.
In some cases, surgery may be needed to repair the tendon or tendons and perhaps the supporting structures of the foot (Heckman et al. 2008). The foot and ankle surgeon will determine the most appropriate procedure for the patient’s condition and lifestyle. After surgery, progressive rehabilitation is still essential.
Injuries to the middle of the foot
Midfoot stress fractures
Stress fractures occur as a result of prolonged repeated loads on the foot in the navicular, talus and metatarsals, usually the second, third and fourth (Snyder et al. 2006). Long distance runners are particularly susceptible to this type of injury and experience pain in the affected bone during and when established, after exercise when resting and even pain at night. The nature of the running process, especially with an increased forefoot loading may help to explain the incidence of stress fractures of the metatarsals under fatiguing loading conditions (Weist et al. 2004). There may be palpable tenderness and swelling at the specific point of the injury, but not always.
The navicular bone is subject to one of the most common stress fractures seen in athletes, especially those involved in sprinting and higher foot impact sports like high jump. It presents with a poorly localised midfoot ache particularly during and after activity. Pain resolves with rest but soon returns with resumed activity. It is usually sensitive to direct pressure on the navicular, and can be picked up with a bone scan, CT or MRI, but may not be evident on X-ray.
The talus is more susceptible to developing a stress fracture in activities where the ankle is repeatedly everted and plantarflexed as in footballers changing direction and jumping athletes. Surgery to remove the lateral process of the talus bone is sometimes done, which can speed up the healing and rehabilitation process. There tends to be a gradual onset pain on the outside of the ankle with palpable tenderness and sometimes swelling over the sinus tarsi.
The sinus tarsi is a small osseous canal which runs into the ankle under the talus bone and can become inflamed, leading to discomfort anterior to the lateral malleolus (Frey et al. 1999), Sinus tarsi syndrome can be caused from overuse in conjunction with poor foot biomechanics usually associated with a past ankle inversion sprain (Breitenseher et al. 1997). Running a curve or bend on an athletics track makes the left foot painful. Passive inversion of the subtalar joint elicits pain. An anaesthetic injection into the sinus tarsi will confirm the diagnosis by relieving symptoms.
Treatment and rehabilitation
Treatment for stress fractures is initially very light to non-weight bearing with crutches and possibly immobilisation in a boot or cast for several weeks until the palpable tenderness disappears (Dugan and Weber 2007). Insoles or orthotics, which support and change the line of stress though the foot, are prudent (Finestone et al. 1999). Gradual progressive loading over several weeks, depending on the intensity of the sport back towards full activity is essential. It is important to mobilise the stiff ankle, subtalar and midtarsal joints. Increase in dorsiflexion by controlled lunging exercises and hydrotherapy helps unload pressure on the midfoot. Oral analgesics, as required, are considered preferable to anti-inflammatories, as they may inhibit repair (Harder and An 2003).
Midfoot tendinopathy
The extensor tendons on the dorsum of the foot can become inflamed causing pain and swelling, especially when the tendons are passively stretched. Inflammation of tibialis anterior is the most common and extensor digitorum is the least. Shoes that are laced too tight, putting increased pressure on the top of the foot, can cause pain and swelling on the dorsum of the foot. It is usually exacerbated by running related sports, particularly by repeated braking and hills, where the extensors lift the foot, or downhill where they work eccentrically to slow the foot (Scott et al. 2005). It can also be triggered by a change in training regime, terrain or slippery surfaces. There is always the possibility of an underlying metatarsal stress fracture indicated by resting and night pain, or when the forefoot is passively deviated.
Flexor tendinopathy of flexor digitorum longus and the flexor hallucis longus can also occur in propulsive and repetitive jumping sports like basketball. With peroneal tendinopathy the peronius brevis and longus assists plantarflexion and eversion. Its tendon attaches to the fifth metatarsal on the lateral aspect of the foot and may become very tight in distance runners.
There may be swelling on the outside of the ankle or heel and pain is directly activity related, especially with sports requiring stability and sideways movement like raquet sports or movement on uneven ground and slopes. Apart from palpable pain, as the tendons are quite superficial, pain is exacerbated by passive invertion and dorsiflexion, and resisted eversion and plantarflexion.
Recent studies have indicated that the causes of tendinopathy may not be as simple as was once thought (Almekinders et al. 2003). Causal factors may include overuse, inflexibility, and equipment problems, but tendon degeneration and biomechanical considerations should be included. More research is needed to determine the significance of stress-shielding and compression in tendinopathy. This finding may significantly alter the approach in both prevention and treatment through exercise therapy. Current biomechanical studies indicate that certain joint positions are more likely to place tensile stress on the area of the tendon commonly affected by tendinopathy (Almekinders et al. 2003).
Treatment and rehabilitation
Rest, reducing aggravating movement is effective as it is primarily an overuse injury. A rehabilitation schedule is essential to strengthen the extensor muscles and stretch the antagonistic calf muscles. Anti-inflammatory medication tends to be very effective, even topical application, as the tendons are very superficial (Forslund et al. 2003). If it becomes established a steroid injection into the area is usually effective.
Tibialis posterior syndrome
The tibialis posterior muscle comes from the posterior tibia and its tendon passes behind the medial malleolus, passing under the foot to help support the medial arch. With cumulative impact, inflammation may occur around the posterior medial malleolus and under the foot where the tendon attaches, with pain as the tendon slides in the sheath (tenosynovitis) during exercise. The syndrome is usually associated with an increase in weight bearing ankle evertion and foot pronation. Athletes with this condition may present with plano-valgus (flattened arch) deformity and often play sports with sudden stop-start or push-off activity, such as soccer, football, and basketball. Patients typically complain of pain inferior to the medial malleolus and decreased range of movement.
Treatment and rehabilitation
Rest for a few of weeks may resolve acute episodes but support by insole or orthotic may be necessary longer term (Kulig et al. 2009). Steroid injection into the tendon sheath or immobilising in a brace or cast can be beneficial. Operation is sometimes necessary to repair a ruptured tibialis posterior tendon as it is essential in supporting the arch of the foot.
Tarsal coalition
This is a congenital fusion of either the calcaneo-navicular or talo-calcaneal joints. It usually affects adolescents as the joints between the bones consolidate. This may cause decreased range of motion in the rearfoot resulting in compensatory pain in the midfoot after weight bearing training and often becomes more obvious after an ankle sprain when the pain does not improve. An X-ray can show an osseous coalition but an MRI may be needed to demonstrate a fibrous one.
Treatment and rehabilitation
The goal of non-surgical treatment of tarsal coalition is to relieve the symptoms and reduce the motion at the affected joint. Treatment and rehabilitation depends on the severity of the condition and the response to treatment (Saxena and Erickson 2003). Sometimes the foot is immobilised to give the affected area a rest. Anaesthetic injection into the leg may be used to relax spasm and is often performed before immobilisation. The foot may benefit from being placed in a boot to immobilise, and crutches to reduce weight on the foot. Management primarily to mobilise the joints around the painful complex, alongside orthotic devices to distribute the weight away from the joint, limiting motion at the joint, may relieve pain.
Non-steroidal anti-inflammatory drugs may be helpful in reducing the pain and inflammation. If symptoms are not adequately relieved with non-surgical treatment, surgery could involve removal of the abnormal connection, or arthrodesis (permanent fusion) of the joint. The surgeon will determine the best surgical approach based on the patient’s age, condition, arthritic changes, and activity level (Saxena and Erickson 2003).
Midtarsal joint sprain
The midtarsal joint consists of the calcaneo-cuboid and talo-navicular joints. A sprain of these joints is more likely to be seen in sport with landing impact like gymnastics, or uneven surfaces and change of direction like football. Calcaneo-cuboid injury presents with pain and swelling on the lateral dorsum of the foot often occuring in association with an ankle sprain. Passive inversion of the foot is uncomfortable. X-ray should ideally rule out a fracture.
Treatment and rehabilitation
Taping the foot, and longer term insoles or orthotics, help support the joint recovery (Willems et al. 2005). Exercises to improve and maintain dorsiflexion are important but may have to be patiently employed because of impingement discomfort. If symptoms persist, a steroid injection may aid recovery.
Sometimes after a severe ankle injury there may also be a fracture of the anterior process of the calcaneum. Combined active, and especially passive plantarflexion and eversion is painful. Treatment is similar to that of the calcaneo-cuboid sprain but with a longer period of reduced weight bearing and immobilisation, and surgery may be considered.
Cuboid syndrome
Particularly following an ankle inversion sprain, the peroneus longus may have excessively pulled on the cuboid, causing it to sublux (partially dislocate) resulting in pain when weight bearing on the outside of the foot. The mechanism is often associated with peroneal tendinopathy which should also be treated. It is involved with locking the foot for strength during various stages of the gait cycle. Any instability or dysfunction around the cuboid inhibits functional stability in the foot during propulsion. Athletes with cuboid syndrome will tend to evert and pronate more. They will avoid forcefully pushing off with the foot. Lateral, side-to-side sports, such as tennis or squash, place the greatest strain on this area.
Treatment and rehabilitation
There is some debate (Patterson 2006) whether the cuboid can or needs to be passively manipulated back into position. Non weight bearing hydrotherapy and swimming can be very beneficial, especially in the early stages. Taping to alter the mechanical stress and support the mid-foot may be beneficial for pain relief and recovery (Patterson 2006). Trimming a 0.5 cm thick felt pad approximately 2cm square and taping it under the cuboid may help to support. This is the area under the lateral border of the foot, just behind the base of the fifth metatarsal. Insoles and orthotics may not be tolerated unless relatively soft and flexible.
Lisfranc’s fracture/dislocation
This injury to the tarso-metatarsal joints in the foot may be associated with midfoot sprain. If left untreated it may have significant consequences. It presents with midfoot pain and difficulty weight bearing, swelling on the dorsum. Passive plantarflexion causes pain, especially if rotated at the same time. Lisfranc is often missed, even with an X-ray, which is more definitive in a weight bearing position. MRI or bone scan is necessary to confirm the diagnosis.
Treatment and rehabilitation
A plaster cast with a toe plate extending under the toes is applied below the knee to immobilise the joint. Sometimes the bones require fixing with pins or wires. Surgical reduction of the bones is required if there is displacement, with immobilisation for several weeks followed by hydrotherapy and rehabilitation exercises to restore movement and stability (Latterman et al. 2007). Orthoses may be used to correct the intrinsic alignment of the foot and support the second metatarsal base.
Injuries to the forefoot
Metatarsal injuries
Metatarsalgia is an inflammatory condition which occurs in the joints between the metatarsals and phalanges (MTP joints), usually in the second, third or fourth MTP joints. It usually presents with gradual onset forefoot pain, exacerbated by weight bearing (Cohen 2007). Inferior palpation pressure, or flexion, of the MTP joint elicits pain. Sometimes the metatarsal head (MTP) descends or ‘drops’ causing focal weight bearing pressure. A high arched semi-rigid foot with tight extensor tendons of the toes may increase the potential for metatarsalgia. A short first metatarsal causing increased compensatory pressure through the second metatarsal is called Morton’s metatarsalgia. X-ray may show a degree of joint degeneration, which will reduce improvement outcomes.
Treatment and rehabilitation
Anti-inflammatory medication may be prescribed to reduce pain and inflammation, but should only be a short term temporary measure. Material, insoles or orthotics to protect and dissipate pressure can be applied (Kang et al. 2006). Anti-inflammatory or ‘lubricating’ (Pons et al. 2007) injection into the joint has been successful in chronic cases (Courtney and Doherty 2005).
Neural signs
The metatarsal bones sometimes appear to compress the nerve between the metatarsal bones causing it to be painful or sensory loss particularly between the 3rd and 4th metatarsals. This may be caused by a benign mass (neuroma) on the plantar digital nerve between the toes. Narrow, close fitting shoes, like sprinting spikes, sometimes appear to compress the nerve between the metatarsals. These symptoms are particularly prevalent in sports where there is repeated twisting on the ball of the foot such as golf and squash (Nunan and Giesy 1997). Pain is induced by squeezing the forefoot or pressing between the metatarsals on the dorsal aspect.
Treatment and rehabilitation
A ‘metatarsal pad’ which elevates and spreads the metatarsals may reduce pressure on the nerve (Kang et al. 2006). These can be incorporated into an orthotics device. Circumferential taping of the foot, although compressive may relieve pain and pressure on the nerve by altering active posture and reducing mechanical compression. There is little evidence to suggest specific foot exercises influence symptoms (Headlee et al. 2008). Decompression operation has been successful in stubborn cases.
Metatarsal fractures (Figure 23.10)
The metatarsals can be fractured through direct impact from, for example solid ground or football studs (Reeder et al. 1996). If the bones are not displaced then a short cast or boot should be fitted for the first three weeks. After six weeks the foot should be X-rayed again to ensure it has healed before a gradual return to sport can start.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree