Whilst it is certainly possible to damage one of these joints in isolation and it is true to say that the TCJ is implicated in the majority of lateral ankle sprains (Hertel 2002), concomitant STJ sprains may be present in as many as 80% of people presenting to sports medicine clinics with a lateral ankle sprain (Meyer et al. 1986). This behoves us to become adept at assessing all the structures in the ankle.
Stability of the ankle complex
The bony architecture of the ankle is partially responsible for joint stability but only in certain situations. The medial and lateral malleoli prove a certain degree of side-to-side stability and in full weight bearing, all ligaments are in a relaxed state and so it is the congruency of the talo-crual joint that is all-important. The ankle is least stable in plantarflexion (the loose packed position) and so it comes as no surprise that this is the position most widely implicated in acute ankle injuries.
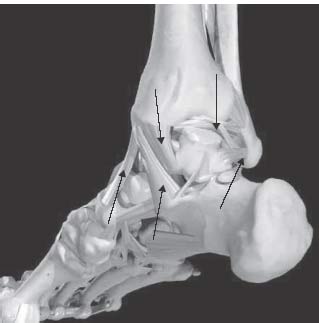
There are several ligaments that provide support to the ankle complex. The major ones are listed in Table 22.1 and illustrated in Figures 22.3 and 22.4.
Table 22.1 Ankle ligaments
Dynamic stability of the ankle complex is provided by the peroneal muscle group, in particular the peroneus brevis and longus. The action of these muscles has been shown to be anticipatory, preparing the ankle to accept body weight at foot strike (Konradsen and Hojsgaard 1993). In fact, it is the loss of the pre-emptive function of the peroneals that is thought to be one of the sequelae of CAI, leading to the foot accepting load in a more plantarflexed and inverted position. The load-to-failure point of the peroneal tendons is thought to be greater than that of the ATFL and equal to the CFL (Attarian et al. 1985).
History of acute injury
Mechanisms of ankle injury
As with all injury assessment, determining the mechanism of injury and the position of the ankle at the time of injury is particularly important when trying to deduce the injured structures(s). The most commonly reported method of spraining the lateral ligaments is when the ankle is “rolled” into plantarflexion and inversion (Wolfe et al. 2001). This is a common occurrence in sport such as when landing from a jump onto an opponent’s shoe in basketball or when reaching for a wide backhand volley in tennis. In these situations, forefoot contact often precedes calcaneal contact, leading to a plantarflexion moment on the talus, thrusting its narrow body between the malleoli, and exposing the lateral ligaments to a stretching force that may exceed its tensile strength (Ritchie 2001). Whilst it is possible to sustain an isolated CFL injury, it is infrequent. It may occur in an incident that involves inversion in dorsiflexion or external rotation when fully weight bearing. This mechanism may also injure the syndesmosis or the talar dome. A combined ATFL and CFL injury is said to occur in 20% of ankle sprain cases (Brostrom 1964). PTFL injuries are usually found in the severely injured ankle where both the ATFL and the CFL have been injured as well. An isolated PTFL lesion is exceptional. The sequence of ligament rupture under inversion stresses are:
Should the inversion stress continue, the ankle complex may dislocate or fracture (Safran et al. 1999).
It is also possible to injure the deltoid ligament on the medial side of the ankle when the weight of the body is forced over an everted foot. Given the high forces that are required to do this however, the injury is infrequent and a lateral malleolus fracture or syndesmosis injury should be excluded in this instance.
Onset of pain
The most important thing to exclude in an acute ankle injury is the presence of a fracture. It is for this reason that the Ottawa Ankle Rules were formed (see below). It is possible for an athlete to sustain an ankle ligament sprain and not notice it at the time (particularly in a combat or collision sport where there may be a strong stress-induced analgesia response) although it is more common for any injury to be accompanied by immediate pain. An ankle fracture will almost invariably not allow the athlete to put any weight on it at all whereas a sprain may allow weight bearing but may get worse as it is continued. The athlete may recall a ‘pop’ or a ‘crack’ at the time of injury but not too much importance should be placed on these sensations, as they do not necessarily relate to the extent of injury.
Area of pain
Determining the area of pain can be particularly helpful when determining the injured structure because many of the ligaments are quite superficial and can therefore be located with ease. It is often useful to ask the athlete to “point with one finger” where it is most painful. The most frequent area for pain is around the antero-lateral ankle. The medial aspect of the ankle may be painful if there was an eversion force that injured the medial ligament complex although it is also not uncommon for it to be painful following an inversion injury if there was some medial joint compression causing some bone bruising. The pain from syndesmosis and talar dome injuries tends to be more centrally located, deeper and more diffuse. Ankle fractures tend to be exquisitely painful on palpation. The most common sites of ankle fractures are the distal fibula and the 5th metatarsal. These sites should be carefully examined (see the Ottawa Ankle Rules, below). Whilst the site, extent and intensity of pain, swelling and bruising can be a useful early indicator of the location and extent of damage, injury severity is more reliably judged by the degree of disability following the incident (how much the ankle can be actively moved, if weight bearing is possible).
Radiographic investigations and the Ottawa Ankle Rules
In the majority of cases, imaging of the acutely injured ankle is not necessary, as it does not alter the management of the athlete. There are some key exceptions, however, and these mainly revolve around the need to exclude an ankle fracture. In 1992, the Ottawa Ankle Rules (OAR) were published, which provide clinicians with guidance regarding referring an injured ankle for radiographic investigation (Stiell et al. 1992). According to these rules, it is only necessary to seek an X-ray of an injured ankle in those patients with:
- pain along the posterior edge of the distal 6cm of the fibula (including the tip of the malleolus); or
- an inability to walk more than four steps either immediately or at a subsequent closer assessment within 10 days; or
- pain at the base of the 5th metatarsal.
Should the patient present with any of these signs, they should be referred for an X-ray with anteroposterior (AP), lateral and mortise views. In the mortise view, the talus should be equidistant between the malleoli before a syndesmosis disruption can be excluded (Lynch 2002). Implementation of the OAR have resulted in a dramatic reduction in the number of x-rays taken with no reduction in the detection of ankle fractures (Leddy et al. 1998).
Other investigations such as magnetic resonance imaging (MRI), computerised tomography (CT) and ultrasongraphy (US) are typically unnecessary in the acutely injured ankle because usually they do not change clinical management, which is primarily based on symptoms, although they may be helpful in excluding an osteochondral lesion/talar dome fracture. Down the line, should the athlete’s progress not be as swift as expected, these imaging techniques may be employed. CT is best for imaging osteochondral injuries, whereas US is the preferred technique for the imaging of tendon pathology (Shalabi et al. 2007). US imaging is growing in popularity due to the fact that it can provide dynamic imaging of the foot and ankle, and in particular the soft tissues. For example, it is possible to view the flexor hallucis longus tendon slide round the medial malleolus and through the fibro-osseous tunnel as the ankle moves through its range of motion in the sagittal plane. This has the advantage of the athlete being able to interact with the ultrasonogropher or radiologist and they can demonstrate the movement and indeed the stage of the movement that provokes their pain. This is particularly useful when the athlete has a functional, rather than just an anatomical or structural pathology. At this stage, MRI and CT scans are still limited to static imaging.
Physical examination
Like every joint, the ankle should be examined in sequence. Table 22.2 details the specific areas to be examined.
Table 22.2 Areas of examination
| Test | Purpose of test/looking for | Notes |
| Observation | Swelling, bruising, deformations, alterations in weight bearing | Performed in supine, standing and walking if able |
| Active and resisted movements | Range of motion, quantity and location of pain | Examine PF, DF, inversion, eversion, heel raise |
| Passive movements | Range of motion, quantity and location of pain, end feel | Examine PF, DF, inversion and eversion + overpressure |
| Stress tests | Examines integrity of ligaments. Looking for amount of ROM and pain | Compare to the opposite side |
| Functional tests | Examines the ability of the ankle to cope with integrated tasks such as walking, running and changing directions, jumping and hopping. | Compare to the opposite side if appropriate and look for antalgic movement patterns |
| Palpation | Specific tenderness and swelling | Palpate each structure (see Table 22.3) to see if it hurts, rather than touch where it hurts and then try to determine the structure |
Stress tests
Manual stress tests are often used in the clinical setting to determine the type and extent of ankle ligament injury. The two most common stress tests used for the ankle are the talar tilt test and the anterior draw test.
Anterior Draw Test
This test assesses the anterior translation of the talus with respect to the tibia. It is best performed with the patient sitting up with their legs over the edge of the bed in order to relax the gastrocnemius. The tibia is stabilised with one hand and the other hand grasps the talus and draws it forward in the sagittal plane. A positive test is said to be one where there is greater anterior displacement of the foot with respect to the lower leg when compared to the uninjured side. It has been stated that sagittal plane displacement of greater than 3mm is indicative of an ATFL lesion (Anderson et al. 1952) although like many manual stress tests, the results remain largely subjective and should therefore be used as a guide only. It can also frequently provide false negative results if there is guarding of the ankle due to pain or a thickened fat pad at the posterior calcaneal tuberosity (Johnson and Markolf 1983).
Talar tilt test
The talar tilt (TT) test is used to assess anterolateral rotation of the ankle joint, a movement that is normally restrained by a combination of the ATFL and the CFL. The TT test is performed with the ankle in slight plantarflexion, the tibia and fibula held stable. The calcaneus and talus is grasped with the other hand and “tilted” into inversion. This is then compared to the uninjured side with a talar tilt of greater than 15° when compared to the uninjured side has been correlated with a dual ATFL and CFL strain (Gaebler et al. 1997) although there is a wide range of values for both injured and uninjured ankles reported in the literature which makes interpretation difficult (Frost and Amendola 1999).
The current consensus of opinion is steered towards functional, non-operative treatment, irrespective of the amount of ligamentous laxity demonstrated on stress testing. As a consequence, the treatment of the injured ankle is contingent on the functional status of the ankle and so the exact degree of ligamentous laxity may indeed be moot.
Palpation of structures
Palpation of the ankle after an injury can be especially useful when trying to localise an injury to a structure. A good habit to get into is to systematically palpate structures in order and see if this elicits pain. This is better and more reliable than going straight for where it is sore and then working backwards to deduce exactly what it is that is sore underneath your finger. This will help minimise injured structures not being detected. The order of palpation should be as shown in Table 22.3.
On field assessment of the injured ankle
The key thing to note is the position of the ankle at the point of injury. If the ankle was in a fully weight bearing position when it was rolled, the chances are there is more extensive damage and the player is unlikely to be able to continue playing. It is important to check the un-injured ankle to determine what is “normal” and thus comparison of end feel can be made more authoritatively. If the player has an immediate effusion or bruising and/or is unable to weight bear, they should be removed from the field. If the decision is made to allow the player to continue playing, they should be observed to ensure that he is able to run freely, change directions and decelerate rapidly. If they cannot perform these tasks, there is a likelihood of a more serious injury and should be taken from the field for a more thorough assessment and immediate management.
Table 22.3 Order of palpation
| Structure | Location |
| Distal fibula | Along the posterior edge of the fibula from 6cm above the tip of the fibula. If there is marked tenderness, the athlete should be referred for an X-ray to exclude a fracture. |
| Tip of the lateral malleolus | At the furthermost tip of the fibula to help determine the presence of an avulsion fracture |
| ATFL | From the lateral malleolus down to the talar neck (best done in plantarflexion and inversion) |
| CFL | From the lateral malleolus vertically down to the calcaneus (best done in inversion) |
| PTFL | From the back of the lateral malleolus across to the posterior midline |
| Peroneal tendons | Posterior to the lateral malleolus to the base of the 5th metatarsal (peroneus brevis) and underneath the foot to the medial cuneiform and great toe (peroneus longus) |
| Base of 5th metatarsal | Lateral aspect of the 5th metatarsal base to assess for avulsion of the peroneus brevis |
| Deltoid ligament | In a fan shape extending down from the medial malleolus to the navicular, sustentaculum tali and talus |
| Sustentaculum tali | A bony ridge inferior and slightly anterior to the distal end of the medial malleolus |
| Sinus tarsi | A ‘cavity’ or tunnel located anterior and inferior to the lateral malleolus leading to the subtalar joint |
| Anterior tibiotalar joint line | Best assessed in with the ankle at rest in plantarflexion |
| Talar dome | Slightly inferior to the tibial plafond when the foot is plantar flexed to 45° |
| Anterior inferior tibiofibular ligament | Anterior border of the distal fibula shaft obliquely up to the tibia to assess for the ‘high ankle sprain’ |
| Flexor hallucis longus tendon | Posterior to the medial malleolus and it courses down through the talus’ fibro-osseous tunnel |
| Posterior ankle recess | Posterior ankle between the malleoli and deep to the achilles tendon. Palpate from the calcaneus up to the talus. |
An on-pitch assessment may need to be limited to range of motion (ROM), a couple of stress tests and ability to weight bear. In a clinical setting however, a full assessment should be conducted in order to be more diagnostically precise.
Grading of ankle ligament injury severity
Grading an injury to the lateral ankle ligaments remains a controversial topic because, by-and-large, grading scales are subjective and hard to validate. The three main scales used to grade severity are listed, below:
1. Grading based on number of ligaments injured (ie, a 1,2 or 3 ligament injury). The downfall of this method is that it does not assess to what extent each ligament is injured.
2. Traditional grading based on the extent of structural damage. A grade I injury exhibits microscopic unfurling of the crimped pattern of the ligament without any macroscopic damage. A grade II injury has macroscopic stretching without ligament rupture. A grade III injury is a complete rupture. The downfall of this method is that it is almost impossible to validate in the clinical setting.
3. Clinical judgement grading based on functional ability. In this method, a grade I injury is assessed as involving no or minimal functional loss, no extra joint ROM, little or no pain, swelling or bruising. A grade II injury is where the patient’s ankle ROM is reduced although accessory movement testing reveals extra joint movement but a firm end-feel, moderate pain over the injured ligament, swelling and bruising. A grade III injury implies complete rupture where there is no longer an end-feel on accessory movement testing, overall joint motion is markedly reduced, there is marked swelling and bruising and function has been lost.
Syndesmosis strains
The ankle syndesmosis is composed of the anterior inferior tibiofibular ligament (AITFL), the posterior inferior tibiofibular ligament (PITFL) and the interosseous membrane. The mechanism of injury is forced external rotation of the weight bearing foot or forced plantarflexion such as rolling over the front of the ankle. Injuries to the syndesmosis have historically been underdiagnosed and are a significant source of chronic ankle pain in the athlete. Like other ankle ligament sprains, injuries to the syndesmosis are often graded in terms of amount of damage sustained with a Grade I indicating AITFL stretch, Grade II indicating AITFL partial tear and Grade III indicating complete AITFL rupture (O’Donoghue 1984). The AITFL is tender on palpation, particularly when it is stressed with the external rotation stress test. For this test, the athlete is seated with their legs overhanging the couch, hips and knees flexed to 90 degrees. The lower limb is stabilised with one hand whilst the other hand dorsiflexes and externally rotates the foot. A grade I-II injury should be immobilised in a walking boot until pain free (typically up to 2 weeks) and needs to be followed by a progressive active rehabilitation programme. A weightbearing X-ray that demonstrates widening of the mortise may require a surgical opinion with a view to internal fixation. Following surgical fixation of a grade III syndesmosis strain, an athlete may be back to athletic competition in around six weeks following a progressive rehabilitation programme (Taylor et al. 2007).
Other causes of anterior ankle pain
Anterior impingement
Anterior impingement occurs when either anterioraly located hypertrophied soft tissue, boney exostosis on the talus or tibia, or loose body limits tibio-talar dorsiflexion. The athlete complains of persistent pain at the front of the ankle, particularly when lunging. It is also commonly seen in football in the non-dominant kicking leg. It may be caused by repeated loading at the extremes of dorsiflexion as seen in football or ballet. It is often seen after a lateral ankle sprain where there may be arthrokinematic changes that limit the posterior glide of the talus in the mortise (Hubbard and Hertel 2006). There may be tenderness on palpation of the anterior joint line and in advanced cases, it may be possible to feel a boney spur. Manual therapy to restore normal accessory talus motion and anti-inflammatory medications/modalities are often helpful and a period of rest from loaded dorsiflexion activities is recommended. Tape can be applied to limit the extent of talo-crual dorsiflexion.
Sinus tarsi syndrome
The sinus tarsi is a small tunnel that is located near the talar neck and the calcaneus at the antero-lateral aspect of the ankle, slightly antero-inferior to the lateral malleolus. The sinus tarsi is densely packed with synovial tissue that is easily inflamed. In the majority of cases, the athlete will have a history of at least one ankle sprain and present complaining of diffuse pain slightly below and anterior to the ATFL (Oloff et al. 2001). They may describe pain when walking on uneven ground, jumping or hopping to the side of the injury, landing from a jump or running off-line. Manual therapy of the subtalar joint can be very effective and whilst frequently the athlete will receive great benefit from a corticosteroid injection into the sinus, a proprioceptive, strength and biomechanical rehabilitation programme is imperative to correct the underlying causes of the pathology.
Osteochondral lesions of the talar dome
Osteochondral defects (OCD) of the talar dome are commonly thought to be due to impact of the talar dome as it shears across the tibial plafond as either a single trauma or as a result of repetitive plantarflexion + inversion ankle sprains. A large fracture of the chondral surface can be diagnosed at the time of injury but in many cases they are a diagnosis of exclusion as the athlete complains of recalcitrant, deep and diffuse anterior ankle pain that, despite appropriate conservative rehabilitation, lasts much longer than would be expected for a “normal” ankle sprain. Talar dome injuries can be tested clinically by palpating the talar dome (best located just distal to the tibial plafond when the ankle is plantar flexed). They are best diagnosed with an MRI scan (Mosher 2006) but CT scanning may be required as an adjunct to determine the extent of the chondral surface damage and, dependent on the extent of the lesion, may need surgical stabilisation, after which a comprehensive and extensive rehabilitation programme is necessary.
Lateral ankle pain
Peroneal tendinopathy
Peroneal tendinopathy is usually an overuse injury and is one of the most common causes of non-traumatic lateral ankle pain. The athlete will usually present with an insidious onset of lateral ankle pain, often located either posterior to the lateral malleolus, at the base of the 5th metatarsal.
A retrospective review of 40 patients who underwent peroneal tendon repair for peroneal tendon tears demonstrated that the peroneus brevis was by far the most commonly implicated tendon (88% of cases) with the rest being made up of peroneus longus tears. In 37% of cases there was a combined brevis and longus tear. The average age of the patient was 42 years and the most commonly reported mechanism of injury was a lateral ankle sprain (Dombek et al. 2003). These findings are consistent with those reported by (Saxena and Cassidy 2003).
Treatment of peroneal tendinopathy will depend on whether the pathology is acute and proliferative or chronic and degenerative. Both will require a period of rest from aggravating activities and biomechanical correction with footwear analysis and potentially orthotic insertion. Soft tissue therapy is useful to reduce muscle tone in the peroneals and gastro-soleus complex but there is some evidence to suggest that aggressive stretching of a pathological tendon is not advisable. Whilst strengthening of the peroneals is vital in both the acute and degenerative condition, the more chronic the situation, the more likely it is to respond to eccentric loading (Alfredson and Cook 2007).
Iselin’s disease
Iselin’s disease is a traction apophysitis of the peroneus brevis at its attachment onto the base of the 5th metatarsal. It is found in adolescents, particularly those with a prominent 5th metatarsal that participates in sports that require sudden changes in direction such as football, lacrosse and cross country running. Treatment for Iselin’s disease is always conservative and may involve rest from provocative activities, anti-inflammatory interventions and medications followed by a progressive rehabilitation programme.
Posterior ankle pain
Posterior ankle impingement (PAI) syndrome
The posterior aspect of the ankle is a common site of pain in the athlete who participates in activities that requires extremes of talo-crual plantarflexion such as taekwondo, ballet, running and football. PAI is labelled as a “syndrome” because it is an umbrella term that is used to describe pain anywhere in the posterior region of the ankle joint. There are, however, a number of factors that can contribute to this condition. The athlete will commonly report pain upon plantarflexion, particularly if it is forced. PAI can arise from overuse or traumatically.
The structures in this area of the ankle that can be compressed and thus cause pain are:
- os trigonum (an unfused part of the back of the talus, present in 10–15% of the population).
- thickened posterior joint capsule or PTFL
- enlarged posterior talar process or distal tibial osteophyte
- posterior joint synovitis
- flexor hallucis longus tendon (Lee et al. 2008a)
In the overuse scenario, repeated forced plantarflexion (such as kicking in martial arts, downhill running or standing “en pointe” in ballet) gradually increases the normal range of motion of talo-crual joint plantarflexion, thereby reducing the “clearance distance” between the talus and the tibia at the end of range. If this space is further compromised by any or a combination of the above factors a compressive pathology may result.
Traumatic hyperplantarflexion can result in a fracture of the posterior talar process or traumatic posterior joint synovitis. Post-traumatic calcification of the joint capsule can occur as a late consequence of a plantarflexion plus inversion ankle sprain.
The athlete will usually describe a pain at the back of the ankle that they confuse with the Achilles tendon. Palpation of the Achilles tendon, however, is usually unremarkable although palpation of the posterior aspect of the talus will usually reproduce their pain. The pain is usually aggravated by forced plantar flexion. In the painful position, a medial glide on the calcaneus will usually compress the medial structures and a lateral glide will compress the lateral structures, helping to differentially diagnose between posteromedial and posterolateral impingement.
Rehabilitation should address any contributory talo-crual, mid foot and sub-talar joint hypomobility, hypertonic or tight FHL, triceps surae and peroneals and improving calf muscle and intrinsic muscle endurance. This is in addition to correcting any biomechanical/ alignment issues. A posterior recess steroid injection will often be required followed by 7–10 days of avoidance of plantarflexed positions. Occasionally, surgical excision of any structural abnormalities/loose bodies may be required (Lee et al. 2008b).
Medial ankle pain
Deltoid ligament sprain
The most commonly reported mechanism of injury to the deltoid ligament is when the athlete has their foot planted on the ground in a pronated position and then falls outward, placing a large abduction force on the ligament (Lynch 2002). Given the amount of force required to injure the deltoid ligament, there is a high probability of injury to associated structures. For this reason, it is reasonable to expect rehabilitation to be a much lengthier process than for a lateral ankle sprain, although the principles of injury management are very similar.
Flexor hallucis longus pathology
FHL tenosynovitis is an important cause of posteromedial ankle pain. It is particularly common in ballet dancers and kicking athletes due to the extraordinary range of motion that the tendon must travel from a fully dorsiflexed position to a fully plantar flexed one. The athlete will often complain of posterior ankle pain on landing from a jump or when striking a kick/ball impact. It can be differentially diagnosed by medially gliding the calcaneus whilst in end range talo-crual plantarflexion. Also, passive extension of the great toe whilst the patient is in a weight-bearing lunge position will draw the tendon or a thickened and low muscle belly through the fibro-osseous tunnel of the talus, reproducing their pain. This is often referred to as stenosing tenosynovitis (Hamilton et al. 1996). A steroid injection may be useful in the short term to reduce any inflammatory component but the athlete will also need assessment and rehabilitation of any biomechanical abnormalities when they are in a plantar flexed position. Frequently, if the calcaneus is abducted (known as ‘sickling out’) when a heel raise is performed, compression of the FHL will occur and re-education of this movement is required. Should conservative measures fail, surgical intervention may be required.
Tibialis posterior pathology
Tibialis posterior tendon injury is classically an entity of overuse and is characterised by medial ankle pain may track down to its insertion on the navicular tubercle (although it does also have distal attachments onto the cuboid, all three cuneiforms, the plantar calcaneonavicular (spring) ligament and the 2nd and 4th metatarsals). The function of the tibialis posterior is to invert the subtalar and midfoot joints and to help stabilise the medial longitudinal arch. It can become subjected to an overuse injury in the athlete with excessive subtalar joint pronation but is also susceptible to direct trauma. Resisted inversion will often be weak and painful and the tendon may be painful on palpation. MRI or USS is helpful in confirming the diagnosis and rehabilitation usually involves rest, anti-inflammatory modalities (particularly if a traumatic incident), eccentric strengthening and biomechanical correction (often involving tape of podiatric involvement).
Tarsal tunnel syndrome
The tarsal tunnel is a fibro-osseous tunnel formed by the flexor retinaculum as it arises from the medial malleolus and attached to the medial aspect of the calcaneus and onto part of the abductor hallucis longus fascia. Tarsal tunnel syndrome is a painful condition involving entrapment of the posterior tibial nerve in the tarsal tunnel and is characterised by a burning pain in the toes, plantar aspect of the foot or around the tarsal tunnel itself which is worsened by load-bearing (Kinoshita et al. 2006). Occasionally there may be a positive Tinel’s sign but may also require nerve conduction studies and/or MRI. Conservative treatment involves rest, orthotic or tape intervention to reduce excessive STJ pronation and sometimes, steroid injection. Should it fail to resolve, surgical decompression may be indicated.
Stress fractures in the ankle complex
Stress fractures involving the ankle complex are not common but it is important that they are not missed in an assessment. Table 22.4 outlines the more common sites of stress fractures.
Table 22.4 Common sites of stress fractures
| Site | Predominantly seen in | Characteristics |
| Medial malleolus | Distance runners | Persistent medial ankle pain that is aggravated by cyclical load-bearing. |
| Navicular | Distance runners and jumping athletes | Poorly localised antero-medial pain. Requires strict adherence to a NWB protocol. |
| Posterolateral talus | Track and field athletes | Lateral ankle pain aggravated by running and jumping. Secondary to excessive plantarflexion and subtalar joint instability. |
| Calcaneus | Distance runners and jumping athletes | Gradual onset of heel pain made worse by weightbearing. Pain may be reproduced by squeezing the posterior aspect of the calcaneus. |
Treatment of a stress fracture in the ankle will most often require non-weight bearing or sometimes surgical internal fixation. Following this, a period of rehabilitation will be required as will correction of any of the factors that contributed to the problem in the first place, such as faulty lower limb biomechanics, technique faults, excessive training load, metabolic or nutritional factors.
Acute treatment and rehabilitation of the lateral ankle sprain
Following an ankle sprain, it is necessary to embark upon a comprehensive and progressive rehabilitation programme. A recent study by Aiken and colleagues (2008) demonstrated that although there was a natural recovery of strength and dorsiflexion ROM within 1 month following a grade I or II ankle sprain, more sensitive measures of ankle performance demonstrated ongoing deficits in those patients that did not receive rehabilitation intervention. The authors suggested that the ongoing disability following an ankle sprain in people who received only standard emergency care provided evidence of the need for more comprehensive rehabilitation plan. This result has been augmented by a study which demonstrated the superiority of a structured 4-week rehabilitation programme compared to a non-intervention control group on postural control and lower limb function on individuals with chronic ankle instability (Hale et al. 2007). A comprehensive rehabilitation aims to control pain and swelling, restore full joint ROM and kinematics, proprioceptive function, muscle strength and functional performance.
Acute management
The principles of acute ankle injury management are similar to those of other joints, namely to protect the joint, and to reduce pain and effusion. Protecting the joint primarily involves preventing further damage. This may involve removal from the field of play, or reducing weight bearing with crutches. Severe ankle sprains may benefit from short-term immobilisation in an Aircast boot in order to facilitate an optimal repairing environment (Lamb et al. 2009).
The use of cryotherapy is widely practised in the acute management of acute soft tissue injuries. The purported benefits of this are the early control of oedema and haemorrhage from damaged vessels, as well as pain relief. Whilst a theoretical argument can be made to support these claims, as yet there is very little substantive proof that the use of cryotherapy improves clinical outcomes following ankle or other soft tissue injury (Collins 2008). The most common method of cryotherapy is applying crushed ice directly to the injured area although plunging the injured ankle into a bucket of iced water is potentially more effective as it combines both the reduced temperature and the compression provided by the water required to restrict vessel diameter and thereby reduce plasma leakage from the vessels. The cooling effect of the ice also helps to reduce pain and may potentially lower cell metabolism, thereby reducing the hypoxia that can lead to cell death. In the first 48 hours, immersing the ankle into an ice bath should be for a maximum of 20 minutes (intermittently) but should be encouraged every 2 hours. In between times, a horseshoe fabricated from felt or foam can be placed around the malleolus and secured with a compressive bandage. Anti-inflammatory medications are discouraged initially because the inflammatory process is necessary for the healing process to commence but may be commenced after 48 hours to ensure that the inflammatory process is not excessive, in particular, to control the collateral damage that may be caused by excessive neutrophil-mediated activity. Recently, there has been some encouraging signs that anti-inflammatory medications, either taken orally or applied topically can be safely consumed/applied and that there is a corresponding decrease in pain and improvements in short-term ankle function (Banning 2008; Bleakley et al. 2008).
Restoration of joint ROM and kinematics
Full weight bearing should be encouraged as soon as possible so long as the gait pattern is not antalgic. This may necessitate an initial period of partial weight bearing with crutches or walking in a pool (to reduce loading). Manual therapy to restore normal talo-crual kinematics and motion at the subtalar and midtarsal joints can be beneficial. It has been suggested that there may be a positional fault at the inferior tibio-fibualr joint following an acute ankle sprain (Kavanagh 1999) and this may need to be assessed and corrected with mobilisations. Active mobilisations should be commenced as soon as is comfortable and this may involve the use of a stationary bike or cross-trainer, hourly range of motion exercises and lunging (particularly in a bucket of iced water).
Proprioceptive retraining
Ankle injuries can disrupt the body’s neuromuscular feedforward and feedback mechanisms, which may be displayed as reduced proprioception. Proprioception is the internally generated afferent information arising from peripheral areas of the body that contributes to postural control and joint stability. It is made up of joint position sense, kinaesthesia and resistance/force sense (Riemann and Lephart 2002). There is strong evidence that people with chronically unstable ankles demonstrate proprioceptive deficits whether it be in errors in detecting ankle positions prior to ground contact (Konradsen 2002), failure to accurately replicate passively positioned joint angles (Willems et al. 2002), or an inability to accurately set appropriate muscle force levels to provide joint stability prior to landing from a jump (Docherty and Miller 2002; Docherty and Arnold 2008). It seems that these proprioceptive deficits impair the athlete’s ability to prepare the ankle to accept and transfer load in challenging athletic tasks such as changing directions and landing from a jump.
There is no overwhelming argument for a definitive cause of such proprioceptive deficits although alterations in gamma-motoneuron activity affecting muscle spindle sensitivity and reducing the “dynamic defence system” of the ankle are thought to predispose the athlete to repeated bouts of instability (Hertel 2002). Indeed, a recent study showed that proprioceptive training was more effective than orthotics or strength training in reducing the rates of ankle sprains in male soccer players (Mohammadi 2007).
Given these proprioceptive deficits are noted in the chronically unstable ankle, it is important to commence proprioceptive training very early on in the rehabilitation programme. Initially this may involve single leg standing and can be made more challenging by performing this with eyes closed and on less stable surfaces such as a trampoline. Wobble boards are useful as is performing the star excursion balance test (SEBT). The SEBT is a dynamic lower limb reaching test that has been shown to be sensitive in detecting subjects with chronic ankle instability (Olmsted et al. 2002). It involves standing on the ground with the affected foot and reaching as far as possible to touch but not weight-bear on eight diagonal lines positioned 45 degrees from each other in a star shape. Essentially, any activity that challenges the body’s proprioceptive system is useful and the more input the system receives the better. There are several variables that can be adapted to make the tasks more challenging (see Table 22.5 for examples).
Table 22.5 Examples of proprioceptive drills and their progressions
| Variable | Example starting exercise | Example progression |
| Surface |
|
|
| Speed |
|
|
| Sight |
|
|
| Direction |
|
|
| Attention |
|
|
| Decision making |
|
|
| Energy levels |
|
|
The proprioceptive programme should be progressive, fun, challenging, functional and goal-orientated towards the sport-specific demands. Additionally, as healing progresses, the stress that the ankle is put under during these proprioceptive drills needs to be increased to include jumping, hopping, turning and cutting tasks. There are no specific rules about progressing the drills but each of the variables (above) should be taken into consideration. It may be that an athlete has no problems with any of them but their ankle feels unstable when they are fatigued. In this case, this is the variable that needs to be concentrated on. The athlete is allowed back to competition once they can demonstrate that they can complete the requisite parts of their sports-specific proprioceptive tasks during rehabilitation.
Muscle strengthening
All directions of motion should be considered when prescribing exercises for muscle strengthening and conditioning around the ankle. This may involve the use of elastic tubing or weighted cables. The ankle should be stressed both concentrically and eccentrically. As pain permits the ankle’s range of motion to improve, it is important to strengthen into the new range. This will involve working into progressively more plantarflexion and inversion. Interestingly, the current prevailing thought is that whilst strength is an important consideration during ankle rehabilitation, deficits in ankle strength are not highly correlated with chronic ankle instability (Kaminski 2006) although recently it has been found that there may be a deficit in eccentric plantar flexion strength in subjects with functional ankle instability (Fox et al. 2008). Therefore, towards the later stages of a rehabilitation programme, it is advisable that eccentric strengthening is included. Additionally, it has recently been reported there may also be a deficit in knee flexion and knee extension average torque values in subjects with a history of ankle sprains, indicating that proximal neuromuscular adaptations should be assessed and appropriately managed (Gribble and Robinson 2009). The clinical significance of these findings is that muscle strength should be assessed but not be used as the only return to sport benchmark. It is also important to note that if the athlete is having to take an extended period of time out from their sport due to this injury, it is vital that their cardiovascular system and total body strength work is not neglected (these should be maintained, if not improved during the rehabilitative process).
Functional retraining
Once the athlete can demonstrate that they have a return of full ankle ROM and have appropriate levels of muscle strength, fatigue resistance and proprioception (as determined by the SEBT), they can progress to more functional, sports-specific tasks. This will involve a careful analysis of the requirements of the sport and the impacts it will have on the ankle. For example, for a basketballer, their rehabilitation programme will need to progress from jumping on the spot, to jumping for distance and height, landing in a contest for the ball as well as sudden deceleration and changing of direction when running. For a squash player, there may be more of an emphasis on lunging and rapid pivoting on the foot. Frequently, the athlete will require the application of tape to support the ankle when returning to more vigorous activities. Dependent on the structures that require supporting/protecting, this will often involve positioning the ankle in dorsiflexion (or at least neutral) and eversion, and the application of a combination of anchors, stirrups, calcaneal slings, heel locks, figure 6s and sometimes syndesmosis strips. Taping has been shown to restrict the amount of ankle inversion (Arnold and Docherty 2004) but the benefit is likely to be largely proprioceptive or even placebo (Sawkins et al. 2007). Whilst there are no high-quality studies on how long taping should be used for, clinical experience dictates that it should be used for as long as the athlete finds it beneficial. Nonetheless, the athlete should be counselled that it is probably better not to develop a reliance on taping in case for some reason or other taping is not possible down the track. Ankle braces are commonly used as a prophylactic aid to prevent ankle inversion injuries but they may in fact disrupt balance in non-injured athletes (Hardy et al. 2008).
The appendix to this chapter is a booklet that can be given to athletes on the day of their acute ankle sprain. It is, by no means, meant as a recipe, nor is it exhaustive. What it does provide, however, is a logical, progressive pathway upon which an athlete can be led so that they complete all the tasks required in a rehabilitation programme. There is room for adaptation to include sport-specific drills as required. An outcome measure (such as the Foot and Ankle Score, the Standardised Orthopaedic Assessment Tool or the Chronic Ankle Instability Scale) can be given at the start and at the conclusion of the programme so that the athlete can gauge their progress.
Risk factors for ankle sprains
Several factors have been proposed as risks to ankle sprains over the years. One recent published study suggested that slower running speed, poor cardiorespiratory endurance, impaired joint position sense and increased postural sway, decreased tibialis anterior strength, decreased dorsiflexion ROM and increased activity of the gastro-soleus complex were associated with an increased risk of ankle inversion sprains in males (Willems et al. 2005). A slightly more recent study has stated that a decrease in ankle dorsiflexion ROM is strongly associated with an increased risk for ankle sprains (de Noronha et al. 2006). Given the high rates of chronic ankle instability (see below), a previous ankle sprain is perhaps the most potent predictor of an ankle sprain. All these variables should be taken into account if designing a screening programme for the identification of ankle sprains or pre-disposers.
Chronic ankle instability
The rate of recurrence of an ankle sprain has been reported to be as high as 80% (Yeung et al. 1994) and yet the reasons why this rate is so high are still somewhat mysterious. Chronic ankle instability (CAI) is the term used to describe the occurrence of repeated bouts of instability leading to numerous ankle sprains (Hertel 2002). It has been estimated that CAI occurs in 30–40% of individuals who suffer first time ankle sprains but the occurrence of residual symptoms and decreased function are reported to be much higher (Hertel 2006). CAI gives rise to repeated complaints of pain, swelling, giving way, and degenerative joint disease. Interestingly, it appears that CAI is independent of the severity of the original injury and of the treatment received (Kaminski and Hartsell 2002). It is unclear why some individuals go on to suffer CAI. The mechanism of recurrent ankle sprains is not thought to be dramatically different to that of an initial sprain. Clearly, there is no such thing as a simple ankle sprain.
Ankle instability can be due to mechanical causes or functional causes. Mechanical Ankle Instability (MAI) refers to repeated episodes of ‘giving way’ due to structural abnormalities within the ankle complex. This can be due to:
- pathological ligamentous laxity
- athrokinematic abnormalities (such as restricted posterior talar glide in the mortise that limits the ankle’s ability to reach a fully dorsiflexed (i.e. close-packed) position)
- synovial inflammation and degenerative joint changes (such as degenerative osteochondral lesions).
Functional Ankle Instability (FAI) is said to occur when there are repeated episodes of ‘giving-way’ without a specific mechanical cause (Kaminski and Hartsell 2002). FAI is a complex matrix of contributing factors that may include:
- impaired proprioception (joint position sense, kinaesthesia and joint resistance sense) (Hertel 2002)
- muscle weakness and arthrogenic muscle inhibition
- altered postural equilibrium sense (Riemann 2002)
- reduction in preparatory muscle activity to stabilise the ankle prior to ground contact (Hertel 2006)
It appears that CAI may be the product of an interaction between MAI and FAI although despite burgeoning research into this area, the precise nature and interaction of all the contributing factors is still unclear (Kaminski and Hartsell 2002). An interesting area of current research is concentrating on the possibilities that delayed trunk reflexes may predispose an individual to CAI. It seems that central nervous system adaptations in the manner of delayed stabilisation times are found in individuals with FAI, which is a finding somewhat akin to those found in individuals with low back pain (Marshall et al. 2009). A deeper appreciation of the features of CAI will help provide the sports clinician with a framework to structure a comprehensive rehabilitation plan aiming at not just the management of the acute ankle sprain but also the avoidance of the potential chronic sequelae. Certainly, a four-week rehabilitation plan designed to address the strength, range of motion, neuromuscular control and functional deficits seen in patients with CAI has been shown to be beneficial in reversing these trends (Hale et al. 2007) although as yet there have not been enough in the way of longitudinal studies undertaken to determine the long-term effect of such interventional strategies on recurrence rates.
Ankle injury prevention
There are many interventions that are purported to be beneficial in the prevention of ankle injuries. It follows that only the modifiable risk factors for ankle injuries could be prevented. Clearly, a past history of ankle sprains, the biggest risk factor, cannot be modified. A high body mass index is another variable that has been identified as a risk factor for non-contact ankle sprains (Gomez et al. 1998). It has not been conclusively proven why this is the case but it has been theorised that it may be due to an inability to control the body during dynamic movements. It follows that an all-encompassing ankle injury prevention programme should address this variable.
A reasonably well-conducted study by McHugh and colleagues in 2007 found that foam balance mat training for five minutes per day during the pre-season and two times per week during the season was effective in eliminating the risk of non-contact ankle sprains in high body mass high school American Football athletes (McHugh et al. 2007). This study was based on previous findings that have demonstrated the effectiveness of single leg ankle disc training in reducing the prevalence of ankle injuries (Bahr et al. 1997).
Whole body vibration is often used in gymnasiums and in some professional sports settings and is marketed as being very good for increasing lower limb proprioceptive awareness. It is unclear if this claim can be proven, and as yet it is unsubstantiated in a high quality study. Indeed, a recent study has shown that it is not protective against ankle inversion sprains (Melnyk et al. 2009).
It is unclear if prophylactic ankle taping or bracing is effective in preventing ankle injuries. Both Sitler and Horodyski (1995) and Surve et al., (1994) reported excellent reductions in ankle sprains using tape and braces, but McHugh et al. (2007) found no difference in American footballers.
There are, therefore, no clear-cut strategies that are guaranteed to prevent ankle sprains. It probably makes sense to ensure that some ankle stabiliser “activation” strategies are employed prior to athletic activity. This may involve practising landing strategies off a height and off-line (activities such as hopping into diagonally opposed hoops placed on the ground), pre-activation of the peroneal muscles with resistance tubing and single leg loading on balance disc/unstable surfaces. The integration of landing strategy training may also assist with the prevention/reduction of knee injuries (see Chapter 21).
Case study
Assessment
History
Allan, a 21year-old semi-professional footballer, presents with right ankle sprain, sustained 24 hours ago during training. The injury mechanism was a plantarflexion-inversion trauma when he landed awkwardly following a jumping drill. He felt pain immediately around the lateral ankle region but was able to limp unaided to the sidelines where he applied ice immediately.
He has ‘turned’ his right ankle on several occasions in the past three years, once every three months on average. Mostly these incidents are trivial in nature and not accompanied by any significant dysfunction although he has had to miss about five games in total over the past three years due to ankle sprains.
Allan’s first ankle sprain occurred almost four years ago when he slipped on a rock when fishing. He was unable to play sport properly for about two months following this original incident. No specific diagnosis was made at the time although he remembers it being markedly swollen and he could not run for about a month. He reports his ankles as feeling “weak” since then but has not seen a clinician about it before. He generally does not tape his ankle although does occasionally borrow his brother’s ankle brace.
He has no other injury or medical history, does not smoke and is generally fit and well.
Observations
Allan was able to limp into the clinic unaided but his gait was clearly antalgic. Walking with more weight through his right leg increased his distress. There was a marked effusion around the lateral ankle that extended into the postero-lateral gutter. Some bruising was evident distal to the lateral malleolus.
Area of pain
Allan was asked to point with one finger to his area of pain. He indicated a moderately large area around the antero-lateral ankle. The therapist then gently passively plantarflexed and inverted his ankle and he was able to more precisely locate the pain around the area of the ATFL.
Active movements
The most painful movement directions were PF+Inv, a combined movement that is known to stress the ATFL. He was unable to actively lunge due to pain on weight bearing. Resisted eversion was moderately painful indicating that the peroneal tendons may have been implicated by a traction-type force. Knee and hip ROM were full and pain free.
Passive movements
Corresponding with the active movements, PF+inv was painful. Eversion and DF were pain free. Knee and hip ROM were full and pain free.
Stress tests
Anterior draw was painful and showed and increased excursion although the amount of swelling precluded a definitive grading. Talar tilt test showed no increase in movement.
Functional tests
Due to the fact that this was an acute injury and Allan was struggling to perform the most basic of tasks, walking, functional tests were not considered to be appropriate although a note was made to assess these as his status improved. A knee-to-wall measurement was taken however as a objective benchmark. This was shown to be 0.5cm, compared with 9cm on the uninjured left side.
Palpation
Palpation of the ATFL reproduced Allan’s pain. His distal fibula was non-painful, as was the base of the 5th metatarsal. These findings along with the fact that he could walk into the clinic meant that the need for immediate radiological investigations was negated.
Analysis
It was concluded that Allan had sustained an acute ATFL injury. Whilst the clinician was unable to assess the degree of laxity in the ATFL, it was decided that he was functioning as a Grade III injury. Given Allan’s past history of ankle sprains, it was concluded that this was an acute episode of CAI.
Management (days 1–3)
Initially, the priority for management was to protect the injured area and limit an excessive inflammatory reaction. Consequently the interventions were:
- Educating Allan regarding the diagnosis, the pain mechanisms involved, the plan for treatment and the likely prognosis. It was also important that he be educated regarding CAI and the need to rehabilitate fully in order to reduce the risk of further injuries.
- RICE regimen. This comprised iced water immersion for 20 minutes and after every 5 minutes he was encouraged to perform 10 forward leans with the ankle immersed in the water. Following this an elasticised compressive bandage with a padded felt “horse shoe” was applied around the lateral malleolus to ensure uniform compression around the injured area.
- Basic balance exercises were prescribed.
- He was provided with a set of elbow crutches and instructed to only put as much weight through his injured side as was pain free. The motto of “it is preferable to walk well with an aid than poorly without”. He was instructed in the safe usage of crutches on the flat and on stairs.
Assessment (day 3)
Allan had improved greatly over the course of the two days following the injury. He was now able to walk well without the aid of crutches. The ankle was swollen although much less than 48 hours previously. He still had pain when the ankle was plantarflexed had not attempted to jog. His functional status was reclassified to grade II.
Management (days 4–7)
The aims for management now moved to being about functional restoration. Allan had access to a local gymnasium that contained a pool and so he was allowed to walk in the pool as a means of gait re-education. It was also the ideal environment to commence lunging and provided a challenging environment for balance re-training.
Resistive hip strengthening as well as pelvic control and functional balance work was commenced during this period. Manual therapy was concentrating on normalising muscle tone around the ankle complex and ensuring normal talo-crual joint accessory mobility. He was given a home exercise programme that was to be completed twice daily.
Assessment (day 8)
At the beginning of week 2, Allan’s pain was absent during all ADLs and he was able to jog in a straight line. Additionally, whilst there was still some swelling evident around the lateral aspect of his ankle, the postero-lateral gutter had cleared and bruising was no longer evident. His knee-to-wall measurement was 6cm. He was considered to have a functional grade I+ strain by this stage.
Management (days 8–14)
Week two’s programme showed a progressive increase in lower limb load, both statically and dynamically. There was a gradual increase in gait speed from walking to jogging, initially in straight lines and then in gentle curves. Some agility work was introduced using ladders and other proprioceptive drills. He was asked to monitor his symptoms (pain and swelling) after each session and if there was an increase in symptoms, he was not allowed to progress to the next day’s programme. Towards the end of the week, he was able to complete slalom agility courses at up to 80% speed. He was permitted to return to non-competitive, sub-threshold football training. He was a winger and so a running speed programme was given to him by the coach and he was permitted to re-commence striking a non-moving ball over progressively longer distances.
Manual therapy continued throughout this week and by day 14, talo-crual joint mechanics had been restored. By day 14, he was considered to have a grade I strain. This was because he was still getting a small amount of swelling following the second loading session of the day.
Assessment (day15)
Allan had regained full physiological and accessory movement of his ankle complex by this stage. There was approximately 2–3mm of extra anterior draw. It was unable to be ascertained whether this was due to the most recent injury or was pre-existing.
Management (days 15–21)
The aims of the 3rd week of the programme were to integrate specific functional tasks into his rehabilitation. He was joining in with training drills and specific emphasis was placed on tackling, jumping/hopping, and deceleration drills. Additionally, specific gluteal strength-endurance tasks were included and high-level proprioceptive drills were performed. He completed a full training session on day 17 without any latent pain or refractory swelling. He played a competitive cup match at day 22.
Ongoing management
Given that Allan had a long history of ankle sprains, resisted ankle strengthening work as well as proprioceptive drills focusing on landing mechanics (for example, hopping onto a wobble board/landing from a step into a sandpit) were continued three times per week for the next two months.
The programme that Allan followed is included in the Appendix.
Appendix – 21-day ankle sprain rehabilitation booklet
21 day balance protocol following acute ankle sprains
booklet contents
1. acute management information
 assessment
assessment
 ice
ice
 compression
compression
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree