Key principles of subjective history taking
The key aspects of assessing an elbow are: “active listening”, ensuring we take a logical subjective history of the onset of the problem and to guide the history taking but to avoid interrupting the client’s flow of information. Prompts may be along the lines of:
- What brings you to see me today?
- What do you think I can do to help you?
- When did it happen?
Can the client recall how it happened? Did they “fall on an outstretched hand”, commonly abbreviated to FOOSH. It is a constructive way of addressing taking a history if one includes a reflective practice approach and clearly identifies needs (Cole 2005). The goal of reflective practice is to help practitioners to continually improve their practice by identifying what they do well and what areas need improvement (Cross 2004; Hilliard 2006).
It is important to establish “informed consent” for the examination as well as treatment. Some questioning may be misinterpreted as being “personal” and all aspects of the assessment need to be clearly explained and the client given the opportunity to ask questions to clarify anything that they do not understand. Flory and Emanuel (2004) completed a systematic review on informed consent, comprehension or understanding and found that enhanced consent forms had limited success. They recommended that having a team member to spend time talking on a one-to-one basis seemed to be the best way of improving understanding. Lidz, Applebaum and Meisel (1988) discussed two different ways in which informed consent can be implemented. The “event” model treats informed consent as a procedure to be performed once in each treatment course, which must cover all legal elements at that time. The “process” model, in contrast tries to integrate informing the patient into the continuing dialogue between clinician and client that is a routine part of both diagnosis and treatment and has more benefits as a model to work on.
If they cannot recall an injury, was there a change in their training pattern? Had they undertaken any repetitive DIY type activities? Alternatively was there a prolonged pressure applied? How would they describe their symptoms? Did they occur straight away? Has the behaviour of the symptoms changed? Since the onset of symptoms are they “the same”, “better” or worse”? This gives the clinician a guide as to the type of problem. Is it an acute trauma or an overuse/overload problem? Is it a pressure/impingement problem?
From the behaviour and pattern of the symptoms the clinician can get an idea of the stage of healing, from the descriptions the client uses the clinician can start to make some hypotheses by recognising, with reflection on clinical experience, “patterns” and also to localise the tissue most likely to be involved so that their objective testing part of the examination can be appropriate, logical and targeted at localising the target tissue for management. It is essential that the clinician “reflects” on what is being said and clarifies any potential misunderstanding.
Assessment is a dynamic process and it is important that we do not jump to hasty conclusions without first gathering sufficient evidence, reviewing it, in the light of previous experience and “pattern recognition” and clarifying with the client any areas of confusion. It is important that the clinician is clear about the demands of the client’s occupation and sport and to work with the coach if appropriate.
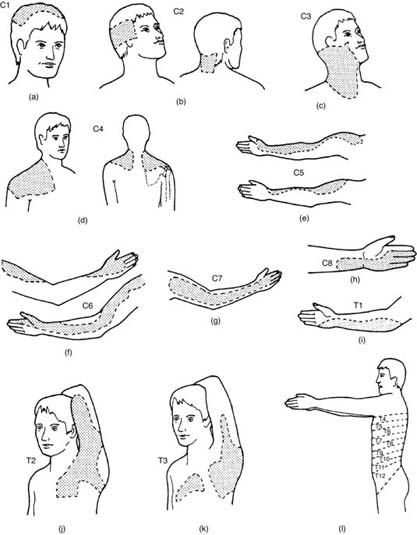
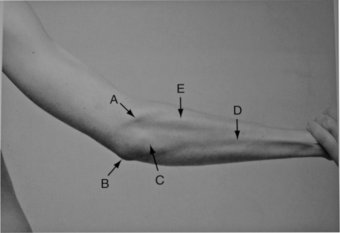
It is absolutely essential to have a good knowledge of applied anatomy of the joint (Figures 18.2–18.5) and supporting soft tissues (Figures 18.6 and 18.7) as well as a working knowledge of “referred pain” from, for example, the cervical and thoracic spine, an applied knowledge of peripheral nerve pathways and muscles supplied by them and therefore affected by a block to nerve supply. Also, it is important to have a knowledge of dermatomes (areas of skin supplied by peripheral nerves), an awareness of variations in dermatomes and also anomalies in dermatomes, which link to a wider and more consolidated knowledge of referred pain (Figure 18.8).
Figure 18.2 Medial view of the elbow. Kuntzman, A.J., Tortora G.J. (2010) Anatomy and Physiology for the Manual Therapies. New Jersey, Wiley.
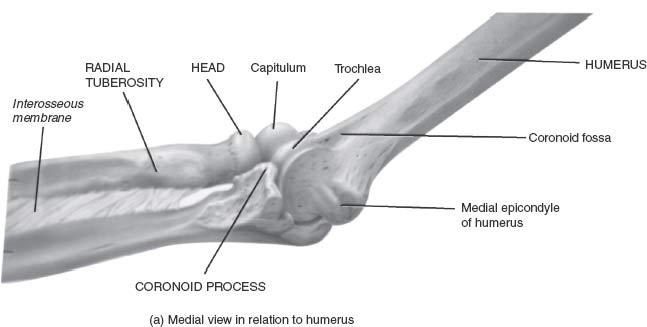
Figure 18.3 Bony landmarks – frontal view. A = Trochlea; B = Capitulum; C = Medial epicondyle; D = lateral supracondylar ridge; E = Radial head; F = Radial neck G = coronoid process. Harris, P.F., Ranson, C. (2008) Atlas of Living and surface Anatomy for Sports Medicine; London, Churchilll Livingston.

Figure 18.4 Bony landmarks – posterior view. A = Subcutaneous surface of olecranon; B = Lateral epicondyle of humerus; C = Medial epicondyle; D = Site of triceps tendon attachment; E = Olecranon fossa. Harris, P.F., Ranson, C. (2008) Atlas of Living and surface Anatomy for Sports Medicine; London, Churchilll Livingston.

Figure 18.5 Bony landmarks – lateral view. A = Olecranon; B = Trochlea notch; C = Lateral epicondyle; D = Lateral Supracondylar ridge; E = Radial neck.
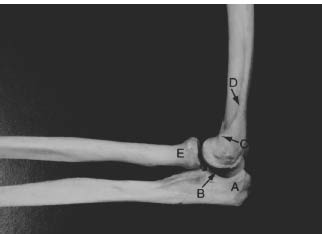
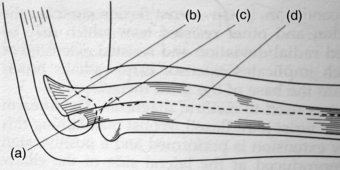
Figure 18.6 Anatomical landmarks – anterior view. A = Biceps brachii; B = Biceps tendon; C- = biceps aponeurosis (passing medially over common flexor tendon); D = Medial epicondyle; E = Olecranon tip; F = Brachioradialis.
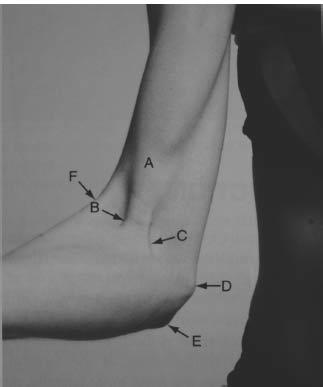
Figure 18.7 Anatomical landmarks – posterior view. A = Lateral epicondyle with common extensor tendon; B = medial epicondyle; C = Subcutaneous surface of olecranon; D = posterior subcutaneous border of Ulna; E = Extensor Carpi Ulnaris.
It is essential, to have an awareness of the variations of “normal” in terms of: range of movement, (ROM) is it within the normal limits or is it hyper-mobile/excessive motion? Is it stiff/limited in some way and if so, is that due to pain, apprehension, swelling, protective spasm. Application of these principals will facilitate a differential diagnosis.
Key principles of objective examination
Observation
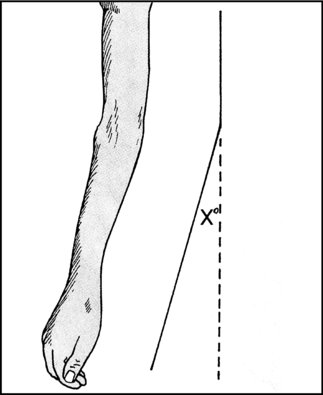
Ideally a general observation is made of the client without the patient being aware, for example as they enter the reception area. The three key points to observe are: face, posture and gait. The face may indicate pain or lack of sleep. In terms of posture, there is an increased “carrying angle” in females (to clear the hips) than in males. The client may be protectively, “guarding” their elbow, they may be hypermobile (see Figure 18.9), or have a reduced arm swing.
Inspection
This should be completed with the client appropriately undressed so that the affected areas may be observed in a good light. The focus should be on: bony deformity, colour changes, muscle wasting or swelling.
The inspection would be completed after a thorough subjective history has been taken and reflected on so that a clinically reasoned approach may be taken as to what to test objectively and why it is being tested. Clinicians may add in additional tests but is essential to have a clear basic examination that is both logical and systematic. The approach taken by Society of Orthopaedic Medicine (SOM), which is based on the work of the late Dr James Cyriax is a good basic assessment approach. Additional tests can be added in as relevant to enhance clinical reasoning
If there has been a fall, there may well be an obvious visible distortion of the bones/joint following an injury, which may well indicate either a fracture or dislocation. Likewise there may be bruising evident or redness indicating inflammation. It is unusual to see muscle wasting in an acute injury as it often relates either to disuse or develops with a more chronic condition. Muscle wasting may also be an indication of neurological involvement. This may be due to reflex muscle inhibition associated with an effusion at the joint. The presence of swelling is indicative of inflammation from either overuse or trauma.
Palpation for: heat, swelling and synovial thickening
It is essential to establish “signs of activity” at this stage indicating presence of inflammation, using the back of the hand and comparing the symptom free side to the symptomatic side. Synovial thickening has a distinctive “boggy” feel and is relatively common in rheumatoid arthritis, particularly at the wrist (Figure 18.10), knee and ankle.
Establish state at rest
The symptoms at rest must be clarified prior to any objective testing requiring movement of joints and muscles. A baseline is established by asking an open question avoiding the use of the word “pain”, to avoid leading the patient. An example may be “How are you feeling now?” Once this has been established it makes comparison of the state at rest with any potential change of symptoms on movement easier to clinically reason. It is helpful to use terms such as: same, better or worse. It may be also useful to utilise a 10-point Likart scale where the patient can draw a line, with “0” being symptom-free and “10” being worse symptoms they can imagine. A constructive suggestion may be to use a printed “smiley” face above the “0” on the scale and a “sad” face above the “10”, on the scale, has a visual impact and helps the client to focus on giving accurate feedback to the rehabilitator.
Examination by application of selective tension
James Cyriax, developed a systematic approach to objective assessment, which is termed “applying selective tension” (Cyriax 1982; Cyriax and Cyriax 1983; Kesson and Atkins 2005). This means to apply: active,passive and resisted movements appropriately. Table 18.2 may clarify the application of selective tension.
Table 18.2 Applying selective tension
| Active | Passive | Resisted |
Active movements assess the range of movement, the pain experienced by the client, strength in the client’s muscle groups and it shows the willingness of the client to move and quality of that movement. The elbow is not an “emotional” joint, i.e. the reported signs and symptoms are normally specific and can be localised easily by the client. Unlike the cervical spine or shoulder that may have a more complex subjective history. Normal active movement of the elbow joint is:
(Loudon 2008) | Passive movements test the inert structures, e.g. joint capsules and ligaments. Passive movements test pain, range and “end-feel”. There are three normal “end-feels” to passive movement testing:
| Resisted movement tests are used in order to test the contractile structures e.g. muscle, tendon. This is the minimum that would be appropriate depending on the experience and the clinical reasoning of the clinician. |
| The possible responses to resisted muscle testing are: Normal response strong and painfree Contractile lesion strong and painful Neurological weakness weak but painfree Partial rupture (or suspected more serious pathology, e.g. fracture or tumour) weak and painful Claudication/provocation of an overuseinjury painful on repetition Psychological component/serious pathology “juddering”/exaggerated response | ||
With the latter response the clinician must heed the warning “beware the bizarre but consistent patient”!
Some clinicians will always start with active range of motion as it provides a guide to a client’s “willingness” to move, the quality of movement and, more importantly, it is a movement within the control of the client at an early stage of the assessment procedure.
Elbow and radioulnar joints
Provocative tests for epicondylitis
These are:
- resisted wrist extension for tennis elbow
- resisted wrist flexion for golfers elbow
An additional test to be aware of if one suspects a peripheral nerve involvement is Tinel’s test. A positive response reproduces the client’s symptoms over the involved nerve sensory distribution. For the ulnar nerve, gently tap along the area where it is most superficial, where it travels along the groove between the olecranon and the medial epicondyle.
Novak et al. (1994) investigated provocative testing for cubital tunnel syndrome and found that this test had 0.70 sensitivity and 0.98 specificity. They had a sample of 32 patients with cubital tunnel syndrome (mean age 46, age range 24–81). Those with a previous history of nerve symptoms were excluded. In the test group 31 of the 32 had a positive Tinel’s sign. The tester performed 4–6 taps over the ulnar nerve just proximal to cubital tunnel. Significant differences (p< 0.0001) between the group with cubital tunnel syndrome and the control group were found for all positive tests. In summary, this test accurately identifies the likelihood of cubital tunnel syndrome, given a positive test.
Within 30 seconds, the highest sensitivity, specificity and positive predictive value were found in the combined test. Within 60 seconds only the sensitivity for the pressure provocation and elbow flexion test increased to 0.98 in those subjects with cubital tunnel syndrome. The combined pressure and flexion test was performed by placing the subject’s elbow in maximum flexion and whilst in this position pressure was placed on the ulnar nerve just proximal to the cubital tunnel. Subject symptom response was recorded at both 30 and 60 seconds. The clinical provocative evaluation techniques have been extrapolated to the cubital tunnel syndrome, although statistical verification of these tests is lacking (Buehler and Thayer 1988; Rayan 1992; Rayan, Jenson and Duke 1992).
The test has been adapted to gently tap over the mid-point of the flexor retinaculum at the wrist, which may reproduce tingling over the median nerve distribution consistent with carpal tunnel syndrome. If these tests are positive the client may be referred on for nerve conduction study tests prior to consideration of surgical decompression of the affected nerve.
Palpation to confirm the lesion site
This is assuming there is nothing in the subjective history to suggest referred pain from the cervical spine. For example, altered sensation, “tingling”, numbness and reduced or absent reflexes. The rehabilitator would then palpate for the exact site of the lesion (Figure 18.11).
Acute elbow injuries
Muscle lesions
Minor muscle tears commonly occur in muscles bellies around the elbow. Muscles likely to be involved extensor group presenting as tennis elbow on the lateral aspect. The pronator teres muscle may be tender 2–3cm distal to the medial epicondyle as a variation of the flexor group presenting as golfers elbow.
Assessment of involvement is by application of selective tissue tension. Pain is reported on resisted muscle contraction and involvement is confirmed by palpation. There is a good response to local transverse friction massage. If it is the muscle belly, the client is positioned with the muscle supported comfortably with the muscle in a shortened position. The transverse friction massage is performed at 90 degrees to the alignment of the muscle fibres. The application of gentle transverse friction massage applied in the initial inflammatory phase that may increase the rate of phagocytosis (Evans 1980). It is useful to apply the technique in the first days following injury provided the grade is appropriate for the stage of healing and the irritability of the tissue, and it avoids disruption to healing and increased bleeding (Kesson and Atkins 2005). This would normally decrease the pain and increase the range of movement. The increase in range should be followed up with exercise in the pain free range of movement.
Tendon ruptures
Acute avulsions of triceps or biceps are rare. Triceps tends to be affected more commonly with excessive deceleration force as in a fall. Biceps tendon is more associated with weight lifting activities. Acute ruptures of either require surgical repair.
Pulled elbow
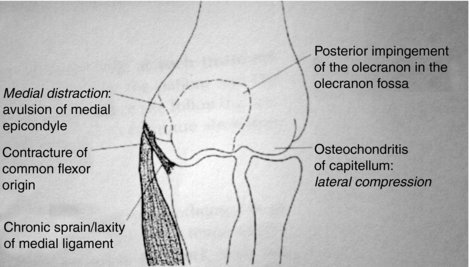
This occurs quite frequently in the under 5s (often accompanied by a guilty and upset parent) as the most common mechanism is when a parent snatches the hand of a child misbehaving at the edge of a pavement, or when parents “swing” their child in play between them. Pitching in baseball, serving in tennis, spiking in volleyball, passing in American football and launching in javelin throwing can all produce elbow pathology by forceful valgus stress (usually during high velocity eccentric loading during the terminal deceleration of the limb), with medial stretching, lateral compression and posterior impingement. With the exception of baseball, there are few prospective cohort studies on the epidemiological trends of childhood elbow injuries in other sports. Delineating injury patterns to the elbow in children can be challenging, given the cartilaginous composition of the distal humerus and the multiple secondary ossification centres that appear and unite with the epiphysis at defined ages (Magra et al. 2007).
The joint at such a young age is lax. It is prone to recurrent injury if the annular ligament is subjected to repeated over-stretching (Illingworth 1975). The radial head easily slides from beneath the orbicular ligament, the child immediately complains of pain and there is a noticeable limit of supination. There is normally a spontaneous recovery if the arm is rested in a sling for 48 hours. It may be reduced by forced supination while pushing the radius in a proximal direction, by forced radial deviation of the hand (McRae 2003; Kesson and Atkins 2005).
In children and adolescents, the epiphyseal plate is weaker than the surrounding ligaments, predisposing them to epiphyseal plate injuries. On the other hand, post-pubescent or skeletally mature athletes are more prone to tendinous or ligamentous injury. Injuries may cause significant impact on the athlete, parents and healthcare system. (Magra 2007)
Fractures/dislocations
It is essential that fractures of the elbow region are diagnosed early and managed appropriately as the complication rate is higher than with fractures close to other joints. Unstable/displaced fractures should be promptly referred for surgical orthopaedic intervention. However, when the articular or cortical surface has less than 2mm of vertical or horizontal displacement, the fracture may be regarded as stable and as such treated conservatively (Shapiro and Wang 1995).
Over vigorous rehabilitation can be an issue with the elbow. Remember, safety of the client is paramount, “first do no harm!” A clear understanding of the applied anatomy and appropriate application of graded rehabilitation should result in there being no problem. Awareness and caution is essential in the musculoskeletal management of the elbow. It is therefore essential that the clinician has an awareness of myositis ossificans, which is a condition that may occur after supracondylar fractures and dislocations of the elbow.
Myositis ossificans/Hetertopic ossification
Myositis ossificans is a calcification which occurs within the haematoma that forms in the brachialis muscle covering the anterior aspect of the elbow joint. It is often attributed to inappropriate vigorous exercise after a supracondylar fracture or dislocation of the elbow. Gentle active, grade A exercise should always be within the painfree range of available movement. The ideal situation is to prevent it happening by avoiding over vigorous exercise. If it occurs it presents as a mechanical block to flexion with an abnormal “hard “ end feel where the normal end feel to end of range flexion should be “soft”. If it is discovered at an early stage and the joint is given complete rest this minimises the mass of calcified material formed in the muscle. In established cases it may be surgically excised after the lesion has appeared dormant for many months so that the range of flexion may be restored.
Often the terms are used interchangeably. However for accuracy, hetertophic ossification simply refers to the formation of trabecula bone outside the skeleton where as myositis ossificans is the specific pathology. So the first is a sign of the other. Kumar and colleagues (2009) describe the difference clearly in the authoritative text Robbins and Cotran Pathological Basis of Disease. Myositis ossificans is distinguished from other fibroblastic proliferations by the presence of metaplastic bone. It usually develops in athletic adolescents and young adults, and follows an episode of trauma in more than 50% of cases. The lesion typically arises in the musculature of the proximal extremities. The clinical findings are related to its stage of development; in the early phase, the involved area is swollen and painful, and within several weeks it becomes more circumscribed and firm. Eventually, it evolves into a painless, hard, well-demarcated mass.
Posterior dislocation
Posterior dislocation is often associated with a fracture of the coronoid process radial head and is probably the most serious acute injury to the elbow. The most common mechanism of injury is in contact sports.
Impairment of the vascular supply to the forearm is a major complication. The assessment of pulses distal to the dislocation is essential. Urgent reduction of the dislocation is required if pulses are absent. Reduction is normally relatively easy to do if it is done quickly before the onset of protective muscle spasm. The elbow is held in 45 degrees of flexion, the clinician applies longitudinal traction by applying a firm grip to the anterior aspect of the humerus. There is often an audible “clunk” when reduction occurs. However, surgical intervention is required as a matter of urgency if post reduction vascular impairment persists. A post reduction X-ray is advised and also assessing the stability of the collateral ligaments.
Undisplaced fractures of the radial head or small fractures of the coronoid process require conservative treatment in a supportive sling for 2–3 weeks.
A common complication is loss of extension following elbow dislocation. Ross et al. (1999) found that immediate active grade A mobilisation (in the pain-free range of movement) has been shown to result in less restriction of elbow extension with increase in instability of the elbow joint. Surrounding muscles should also be strengthened, statically initially then progress through range with a graduated progression in resistance. It is important that rehabilitation is carried out with care as myositis ossificans/heterotopic ossification may occur with over vigorous exercise
Supracondylar fractures
These are more common in children than adults. The mechanism is normally from a fall on an outstretched hand (FOOSH, as it is often written in notes). These fractures should be considered an orthopaedic emergency. They tend to have a high rate of neurovascular complications as they are rotationally unstable. The initial short-term management is closed reduction with pins. The arm is placed in a splint. The pins are removed after a 4–6 weeks. There is not normally any problems with recovery in children.
In an older population, Robinson et al. (2003) found the overall incidence of distal humeral fractures in adults was 5.7 cases per 100,000 per year, with an almost equal male to female ratio. There was a bimodal age distribution, with simple falls being the most common overall cause of fracture, and the majority of the fractures were extra-articular (AO/OTA type A) or complete articular fractures (AO/OTA type C). The risk of complications during treatment was generally low in most patients, and the majority healed their fractures uneventfully. Overall, 90.6% of fractures united within 12 weeks and just under half of the remaining 9.4% patients with union complications healed without requiring further operative intervention by 24 weeks. The risk of union complications was higher following high-energy injuries, open fractures, and non-operative treatment. Although the AO/OTA classification was not predictive of union complications, the low transcondylar (type A2.3 and A3) and simple intercondylar fracture (type C1.3) configuration had a greater risk of union complications than the high subtype. The rate of infection, myositis ossificans, and other implant-related complications were higher following operative treatment of type C fractures than type A and B fractures. They concluded that the epidemiology of a consecutive unselected series of adult distal humeral fractures is defined in this study. The majority of these fractures are best treated surgically by rigid open reduction and internal fixation, except for low Type A and C fractures, which have a higher risk of union complications. The role of total elbow arthroplasty to treat these more complex injuries requires further evaluation.
Radial head fracture
This is the most common fracture around the elbow. They are classified into types 1–4 and the mechanism is normally from a fall on an outstretched hand. Type 1 are “non” or minimally displaced. They respond to early aspiration, splinting (removable) active grade “A” (pain-free) mobilisation and normally are healed in 6–8 weeks. Type 2 are displaced fractures and respond to surgical intervention. Type 3 are managed by surgical excision. Type 4 are fractures in the presence of a dislocation and always require surgical treatment as they can be very unstable.
Olecranon fractures
The mechanism is normally from a fall on an outstretched hand. If it is stable the client should be able to extend the arm and lift it against gravity. Management would be 2–3 weeks in a splint then active grade “A” (pain-free ROM) mobilisation. If it is unstable open-reduction with internal fixation is required. In this instance active mobilisation can start within a week of surgery.
Fracture of the radius and ulna
The mechanism of injury to the forearm bones is a fall on an outstretched hand It is usually clinically obvious. X-rays should be taken for a post reduction comparison.
Two types of dislocation occur: the Monteggia injury, which is a fractured ulna with dislocated head of the radius at the elbow joint, and the Galeazzi injury, which is a fractured radius with dislocated head of the ulna at the wrist joint.
In the adult, perfect reduction by an orthopaedic surgeon for internal fixation of the radial and ulnar fracture is required in order to return to sport. Depending on the accuracy of reduction, either a cast or support is required post-operatively for 8–10 weeks. Monteggia and Galeazzi injuries are often displaced and should be referred to an orthopaedic surgeon for reduction. However, an isolated fracture of the ulna may be treated conservatively by the use of an above elbow cast in mid-pronation for 8 weeks.
In children, angulations of less than 10 degrees are considered acceptable. The favoured position for immobilisation is in pronation, although in proximal radial fractures and also in Smith’s fractures at the wrist, the forearm should extend above the elbow and leave the metacarpophalangeal joints free.
Stress fracture
Stress fractures are a result of overload, overtraining or insufficient rest. Brukner et al. (1999) studied sportspeople (baseball, tennis and swimming) sustaining this type of fracture; they found that the key element of musculoskeletal management was rest primarily. It must also include correction of any predisposing factors and a multi-disciplinary approach to the correction of any faulty technique.
Overuse injuries to elbow and forearm
Tennis elbow/lateral epicondylitis/extensor tendinopathy
“Tennis elbow” is a traditional term. It is a common condition arising in the sporting context from overload in racquet sports. Overload in occupational and domestic settings that include repeated grasping movements particularly middle-aged DIY enthusiasts (Hutson 1990). It is a frequently reported condition, which is characterised by pain over the lateral epicondyle of the humerus and aggravation of the pain on resisted dorsiflexion of the wrist (Verhaar 1994). The incidence in general practice surgeries is about 4–7 per 1,000 patients per year (Kivi 1983). There is an annual incidence of 1–3% in the general population (Allander 1974; Chard and Hazelman 1989; Verhaar 1994). If left untreated, the complaint is estimated to last from 6 months to 2 years (Cyriax 1936; Bailey 1957; Binder et al. 1985; Hudak et al. 1996). (See Figure 18.12 for the possible sites of tennis elbow.)
Historically has been a difficult condition to manage with a wide range of procedures and management protocols advocated (Reid and Kushner 1993; Noteboom et al. 1994; Caldwell and Safran 1995; Putham and Cohen 1999; Jones and Rivett 2005). In general management is prolonged and long-term outcomes questionable.
When it is clinically indicated the mobilisation with movement (MWM) for tennis elbow as described by Mulligan (1999) is a simple but effective means of treating this condition. However, an indication for use is determined by trial application of the technique. The reasons for selection of a MWM for treatment were:
- immediate abolishment of pain during the trial/testing
- previous experience and knowledge of efficacy of the technique
- potential for integration into a home management programme.
(Mulligan 1999)
Struijs et al. (2001) conducted a systematic review of orthotic devices for tennis elbow. This study was done in Amsterdam as 21% of clients with lateral epicondylitis were prescribed an orthotic device as a treatment strategy (Verhaar 1992). They concluded that no definitive conclusions could be drawn concerning effectiveness of orthotic devices for lateral epicondylitis. They reported that no functional outcome measures such as the Pain Free Function Questionnaire were reported (Stratford et al. 1987). They recommended a set of valid and reliable outcome measures be included in management and also the cost effectiveness of a relatively inexpensive orthotic device as a treatment strategy, or as an addition to any other conventional treatment, since the use of orthotic devices may reduce costs of sick leave by reduction of the pain experienced during activities. Better designed and well conducted RCTs of sufficient power are warranted.
The pathological process is a degeneration of the ECRB tendon at the extensor origin of the lateral epicondyle. The mechanism of injury is multi-factorial. The key contributing factors being: “overuse”; a heavy racquet or too small grip; a recent change of racquet or too tight a grip between shots; muscle imbalance and loss of flexibility; poor blood supply of the 1–2 cm of the distal attachment of ECRB; and repeated excessive loading leading to degenerative changes in the tendon. If there is continued use there will be microscopic tearing and scarring within the tendon (Regan et al. 1992). This is a mechanical process primarily and as such it should be described as a tendonosis (Nirshel 1992) or tendinopathy rather than tendonitis. Histiologically, there is an invasion of fibroblasts and vascular granulation tissue, which is known as angiofibroplastic hyperplasia (Brukner and Khan 2002).
With any overuse injury, “relative rest” is required; that is, maintain active full range of motion but limit the “aggravating” activity.
In view of the pathology, the treatment of lateral epicondylitis with corticosteroid injection is controversial (Labelle et al. 1992; Cameron 1995; Assendelft et al. 1996; Hay et al. 1999). It is accepted that in most cases this is degenerative rather than inflammatory. However, with correction of predisposing factors and appropriate staged rehabilitation injection is rarely required.
In a randomised controlled trial in Australia (Bisset et al. 2006) researchers found physiotherapy combining elbow manipulation and active exercise had a superior benefit in the first 6 weeks to corticosteroid injections after 6 weeks providing a reasonable alternative to injections in the mid to long term. The significant short-term benefits of corticosteroid injection are paradoxically reversed after 6 weeks, with high recurrence rates, implying that this treatment should be used with caution in tennis elbow. (See case study at the end of this chapter.)
Other common injuries
This section covers the following injuries: posterior impingement syndromes, thrower’s elbow, stress fracture of olecranon, entrapement of the posterior interosseous nerve (PIN) and radial tunnel syndrome
Posterior impingement of the olecranon fossa, valgus stress to the medial structures of the elbow joint and compression injuries to the radiohumeral joint are all linked to repeated high velocity throwing, for example shot putting (Figure 18.13).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree