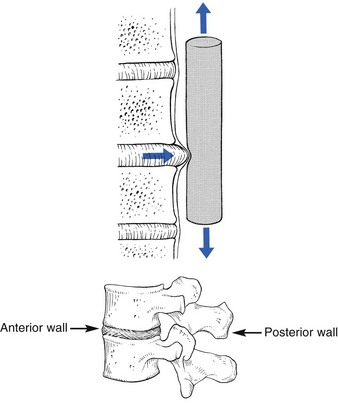
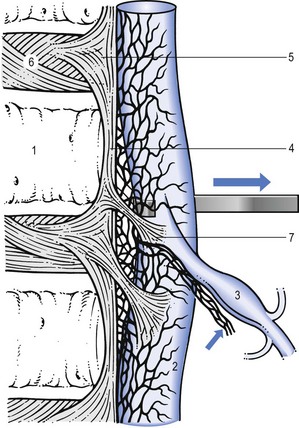
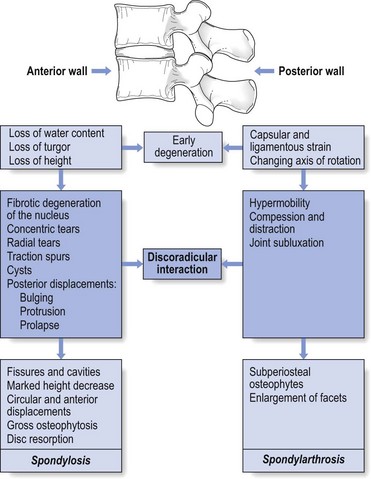
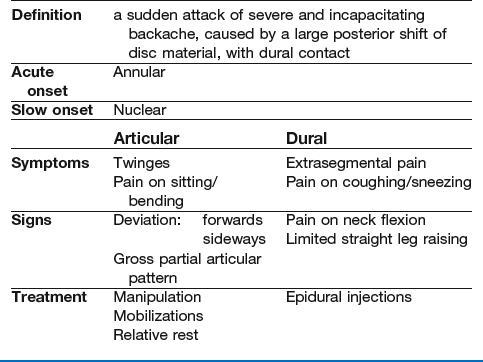
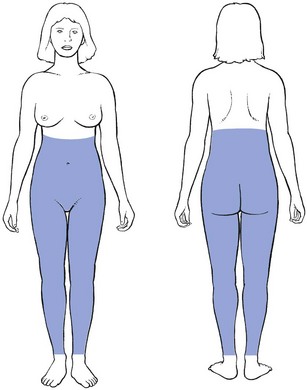
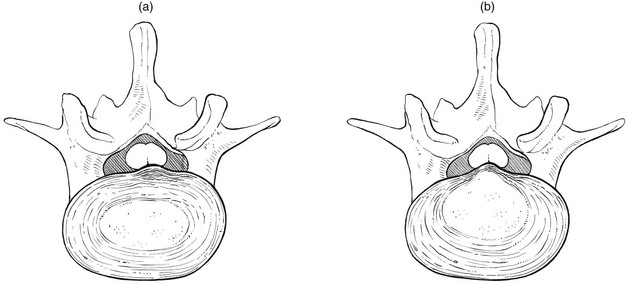
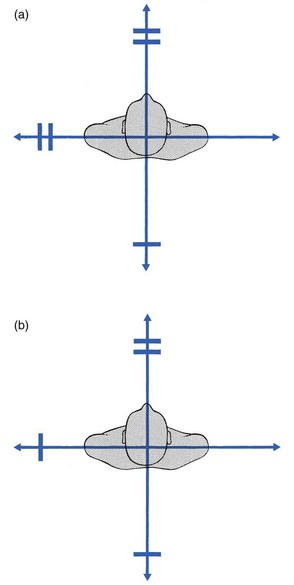
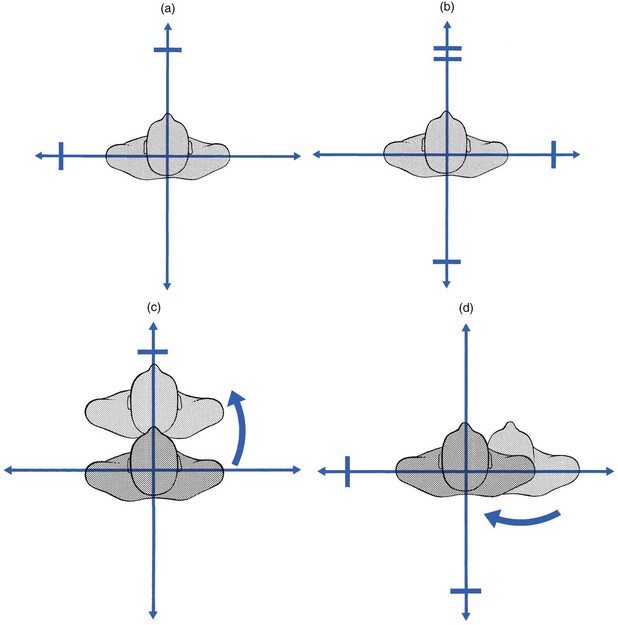
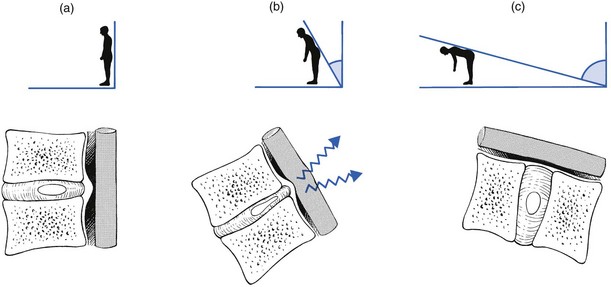
33 The dural concept was first defined by James Cyriax in 1945.1 His hypothesis was that lumbago and backache originate when a subluxated fragment of disc tissue impinges on the sensitive dura mater. This concept – lumbar pain may be of dural origin – is based on two premises: • Disc degeneration and disc displacements are of themselves painless events. • The dura mater is sensitive and translates deformations of the posterior border of the disc into pain. • Data obtained from postmortem studies show the existence of large, symptomless disc protrusions in almost 40% of the cadavers.2 • Several controlled studies have failed to show a relationship between radiological changes seen in disc degeneration and the existence of clinical syndromes.3–5 • Myelograms in asymptomatic patients show defects in 37% of cases,6 and the incidence of asymptomatic disc herniations demonstrated by computed tomography (CT) in subjects over 40 years of age is more than 50%.7 • Recent magnetic resonance imaging (MRI) studies8–11 have demonstrated anew the high incidence of disc degeneration and displacement in an asymptomatic group of patients. One of the most striking clinical features to support the pain-mediating role of the dura is the chronological evolution from backache to sciatica. Almost every instance of sciatica starts with a period of central or unilateral backache, but once leg pain supervenes, the backache usually disappears. Since the work by Mixter and Barr,12 it has been widely accepted that most radicular pain is caused by a disc protrusion compressing the dural investment around the nerve root and, if this is so, it is logical to argue that the earlier backache was brought about by the same disc lesion. If sciatica is referred pain from the dural sleeve, by analogy the prior backache must have originated from the dura mater. Sciatic pain is thus only the final stage of a progression. A small posterior protrusion, bulging out of the intervertebral joint, lifts the posterior longitudinal ligament, touches the dura mater and causes backache. Kept under control by the posterior ligament, the bulge can recede, resulting in spontaneous recovery, or stay unaltered, causing chronic backache. If it increases, however, the counterpressure exerted by the stretched posterior longitudinal ligament pushes it laterally. No longer subject to any resistance, it immediately swells and compresses the nerve root. At the same time, pressure against the dural tube is released and backache ceases (see p. 459). Another proof of the role of the dura in lumbar pain syndromes is the effect of diagnostic local anaesthesia. A weak solution of procaine, induced via the sacral hiatus into the epidural space, and thus forced between the dural tube and the boundaries of the neural canal, causes contact anaesthesia of the dura mater (see p. 556). Because procaine 0.5% is too weak to penetrate the ligaments or the dural membrane, it acts as a surface anaesthetic, thus only desensitizing the structures with which it comes into contact. If the patient had backache before the injection, and anaesthesia affords temporary relief of symptoms and signs, the dura is most likely to be the source of pain. In all cases of acute lumbago and in most cases of acute or recurrent backache, epidural local anaesthesia immediately abates the pain, thus strongly suggesting a dural origin. During the last few decades, numerous neuroanatomical studies have shown that the ventral half of the dura mater is supplied by small branches of the sinuvertebral nerve.13,14 Immunohistochemical studies further demonstrate a significant number of free nerve endings in the dura that contain substance P, calcitonin gene-related peptides and other neurotransmitters contributing to nociception.15,16 The original concept was quite simple: a subluxated (but of itself painless) component of the disc impinges on the dura or the dural sleeves of the nerve roots. These pain-sensitive structures translate the anatomical changes into back pain or root pain, respectively (Fig. 33.1). However, recent anatomical and biochemical studies have slightly changed this original concept: • The outer border of the disc is innervated. Although earlier anatomical studies demonstrated the disc to be totally deprived of innervation,17 more recent research could detect sparse nerve fibres and free nerve endings in the three outer lamellae of the annulus fibrosus,18–20 penetrating to a maximum depth of 0.9 mm into the annulus. This means that, except at the surface, a normal intervertebral disc remains almost without innervation. • Dura mater attachments exist between the anterior part of the dura and the posterior longitudinal ligament (Fig. 33.2). Recent anatomical and MRI studies have demonstrated that the dura mater is not totally disconnected from the vertebral column but also attached to the posterior longitudinal ligament by connective tissue, consisting of ventral and lateral fibrous bands.21–24 Although these ligaments are sufficient to allow for displacement of the dural sac during movement, they could act to place traction on the dural sac in the event of nuclear bulge or herniation.25 • Pain is not only mechanical: inflammatory mechanisms are also involved. Apart from being stimulated mechanically, nociceptors in dura mater may also be activated chemically. An increasing number of experimental studies suggest that disc lesions and/or displacements may induce sufficient chemical changes to irritate the dura mater and to elicit dural pain.26–31 • Articular signs and symptoms are those that are related to the mechanical behaviour of the disc: certain postures and movements create biomechanical changes, which force the protrusion against the dura mater. • Dural signs and symptoms are those that are related to the increase of dural irritation: traction exerted from a distance (straight leg raising and neck flexion) pulls on the inflamed dura or, via the dural ligaments, on the posterior longitudinal ligament or outer annular rim. Also, a sudden increase in spinal fluid pressure pushes the dura against the protrusion (painful coughing and sneezing). One of the factors involved in the dural concept is a subluxated portion of the disc and so the biomechanical conditions to allow such a displacement must be present. First, there must be some degeneration of the disc, leading to weakness of the annular fibres and to radiating fissures. These changes are present very early in the degeneration cycle and, for a number of biomechanical and biochemical reasons, occur most frequently at the rear side of the disc. Second, repeated wear and tear, together with shearing forces and slight decrease of disc height, creates some ligamentous laxity which results in an instability of the whole ‘motion segment’. Third, through enzymatic depolymerization of macromolecules in the disc, the oncotic pressure temporarily rises.32 This means that during a particular period of life (between the ages of 20 and 50 years), the osmotic pressure within the nucleus pulposus increases. Raised intradiscal pressure together with increased segmental laxity is the perfect foundation for disc displacement. A kyphosis imposed on such a predisposed intervertebral joint not only increases the intradiscal pressure but also tends to shift disc material backwards in the direction of the convexity.33 The intensity of the contact between disc and dura determines whether lumbago or backache will result. When the protrusion is more posterolateral, the dural investment and the content of the nerve root, rather than the dural tube, are compressed, with the symptomatic outcome of root pain. Further degeneration of the disc results in its ‘deflation’ and a decline of intradiscal pressure. Decrease in disc height leads to reactive changes at the intervertebral joint and at the posterior structures, which stiffen and stabilize the segment and so diminish the tendency for disc displacements during the later stages of ageing of the spine (Fig. 33.3). The most striking example of a discodural interaction is acute lumbago – a sudden attack of severe and incapacitating backache, with obvious limitation of movement, together with gross dural signs and symptoms, summarized in Box 33.1. The patient states that, during some trivial activity, a sudden ‘snap’ was felt and agonizing pain in the back immediately followed. Very often, this acute event has occurred during a simple movement: coming up after bending, rising from a chair or picking up a light object. Initially, the pain is central and spreads bilaterally over the lower lumbar area and the buttocks. Later, it often tends to radiate more and more unilaterally. Although centralized in the lumbar and/or gluteal area, it spreads to the groin and abdomen, downwards to one or both legs as far as the ankles, or upwards in the trunk as far as the inferior aspect of the scapulae (Fig. 33.4). An attack of acute annular lumbago is caused by posterior subluxation of part of the annular rim, pressing the posterior longitudinal ligament against the dura mater (Fig. 33.5a). It is obvious that a history of sudden pain, immediately followed by a ‘locking’ in flexion, indicates some internal derangement, just as a sudden pain in the knee, followed by inability to straighten it, indicates subluxation of a meniscus. The dural extrasegmental reference of the pain, together with pain on coughing and sneezing, implicates the dura mater and therefore excludes locking of the posterior facet joints. In displacement at the back of the intervertebral joint, the lumbar spine is held in flexion because extension squeezes the protrusion, which in turn increases the painful pressure on the dura. In order to keep the protrusion away from the dura and as immobile as possible, the patient adopts a flexed position. Muscle spasm prevents any further movement at the lumbar spine. The pain, although equally incapacitating, does not appear suddenly but gradually increases over the course of a number of hours or days. Alternatively, after heavy work involving much stooping and lifting or sitting for an unusual length of time in an uncomfortable position, slight backache is felt but is initially regarded as trivial. However, by the next morning the backache is sufficiently severe to make getting out of bed impossible. The pain radiates in a way that is typical of dural involvement (see Fig. 33.4). The patient is immobilized in flexion or side flexion and every attempt to straighten the back is followed by an agonizing twinge in the lumbar area and the buttocks. Sometimes even simple neck flexion is impossible or coughing or sneezing creates a twinge. As in an attack of annular lumbago, the patient has to go to bed to cope with the pain. As a rule the pain eases after a few days or weeks. In gradually increasing lumbago, the protrusion presumably consists of soft and pulpy nuclear material, oozing slowly backwards. This typically happens during the maintenance of a kyphotic posture (sitting, bending or lifting). The displaced nuclear material gradually presses more and more against the outermost layers of the annulus and the posterior longitudinal ligament and makes them protrude (Fig. 33.5b). This provokes dural irritation, resulting in the typical dural pain in lumbar area, buttocks and limbs. During clinical examination the following are important. Deviation towards flexion is noted and the sacrospinalis muscles are seen and felt to be in contraction to maintain the adaptive posture. Because the flexed position places the upper trunk in front of the centre of gravity, the muscles contract to prevent further forward toppling. Lumbago is not caused by muscle spasm – as was maintained by some authorities for many years36 – but is the result of a disorder at the posterior aspect of the intervertebral joint. A lateral shift associated with acute lumbago is a common clinical event, undoubtedly associated with a disc protrusion.37 The lateral shift can be either towards the dominant side of pain (ipsilateral) or away from the side of the pain (contralateral). The majority of affected patients have a contralateral shift.38 Occasionally, the shift may change from side to side, which has been termed an alternating scoliosis. The lateral shift is explained as avoidance of compression or irritation of the dura mater, either actively or reflexively through muscle spasm.39,40 As a rule, extension is considerably limited (Fig. 33.6) on account of the posterior displacement of the disc causing a block at the back of the joint. In lumbago, neck flexion often hurts in the lower back, which proves the involvement of the dura mater in the origin of the pain41 (see p. 502). We have discussed the evidence that SLR is a dural sign (see p. 427) and, just as neck flexion stretches the dura from above, so SLR stretches it from below. A lesion resulting in such a gross discodural interaction as acute lumbago, therefore, must influence SLR. Acute lumbago with full and painless SLR should make the clinician reluctant to accept the diagnosis of a displaced disc. If the acute pain in the back is so severe that the patient cannot move out of bed, but dural symptoms and signs – including a positive SLR – are absent, gross bony lesions such as osteomyelitis or metastases should be considered (see Ch. 39). Lumbago usually causes bilateral limitation of SLR: because the bulge and the dura mater both lie centrally, raising both legs pulls on the dura equally. In unilateral lumbago there will often be more limitation of SLR on the painful side. Occasionally this may be reversed, when the crossed SLR phenomenon is present (see p. 498). The degree of limitation of SLR is an indication of the intensity of the discodural interaction.42 In hyperacute lumbago, any attempt to move the straight leg upwards results in considerable pain, whereas in more moderate lumbago the SLR is limited at 45–60°. During recovery, when the reduction is almost complete, SLR will probably only be painful at the end of range or show a painful arc at mid-range. The progress of SLR is therefore a very sensitive clinical index in following the position of the protrusion during manipulation. Neither muscle weakness nor cutaneous analgesia is present in cases of acute lumbago. Because protrusion is more or less central, nerve roots are not involved. Care should be taken, however, not to miss a compression of the fourth sacral root. Because it lies centrally, partly protected by the posterior longitudinal ligament, a central protrusion can endanger it, especially if the protrusion overstretches the ligament. Physical findings are non-existent and the diagnosis is made entirely on the history. If pain deep in the sacral area, pain and paraesthesia in the penis, vagina or rectum, numbness in the saddle area or problems with continence are mentioned, damage to the fourth sacral root should be considered and the patient immediately referred for further assessment.43 A fourth sacral lesion occurs at a level proximal to the posterior ganglion and permanent interference with bladder function can result if decompression is not carried out.44 Therefore its onset, however slight, is an indication for laminectomy. Cyriax45 (his p. 284) recommends operation even when bladder function is returning after the attack of lumbago, because there is no guarantee that lasting incontinence may not follow the next attack. With, without or despite treatment, most cases of acute lumbago recover spontaneously and completely within 2–6 weeks (Dixon46; Chöler, cited by Nachemson47; Spitzer48). The tension in the posterior longitudinal ligament exerts counterpressure on the bulge, which moves gradually anteriorly, until compression of the dura mater ceases and symptoms disappear. However, as cartilage has little tendency to reunite, a fragment that has moved backwards once will sooner or later move again, which implies that, although complete recovery after an attack of acute lumbago is the rule, recurrences are to be anticipated.49 Alternatively, the lumbago disappears but there is simultaneous onset of root pain. As has already been discussed (see p. 442), the protrusion has moved from the centre to one side. Most cases of acute lumbago recover without treatment. MacNab put it well when he remarked that ‘The physician must constantly remind himself that even if he elected to treat the patient by rubbing peanut butter on each buttock, in the balance of probabilities, the patient would get well fairly quickly.’50 However, keeping the intradiscal pressure as low as possible will, of course, ease symptoms and hasten the reduction of the bulge. It is therefore wise to adopt the supine lying position from time to time, with the knees and the hips flexed to a right angle51; this decreases the load on the disc to about 30 kPa52 (the ‘psoas position’; Fig. 33.7). It is also sensible to avoid movements and positions that cause high intradiscal pressures, such as sitting or bending (Nachemson53: p. 708). Standard textbooks almost unanimously recommend bed rest as the first line of treatment for acute lumbago.54,55 However, it has never been proven that complete and continuous bed rest decreases the time of recovery. In a comparative trial, statistically significant differences between bed rest, early mobilization and no treatment have not been found, although results tended to favour early mobilization.56 Others have reported little difference between mobilization and rest,57 and 2 days in bed was found to be even better than 7 days; put the other way around, 7 days in bed was more harmful than 2 days.58,59 Also, a recent Cochrane review concluded that there is no difference in effect between advice to stay in bed and advice to stay active.60 Therefore bed rest is only necessary if bed is the only place where the patient is comfortable. If, after a couple of days, walking around is possible without a considerable increase in pain, such a regime should be followed. Furthermore, a patient should never be forced to stay in bed against his or her will. In nuclear types of acute lumbago, classic manipulative reduction usually fails. A slow onset of symptoms usually indicates that the protrusion is too soft to be pushed back. Manipulation is also apt to fail in lateral deviation away from the painful side. A good alternative, then, is a sustained manual stretching technique. Positioning the patient in increasing but still comfortable lordosis (McKenzie technique) is another alternative in treating acute nuclear lumbago.61,62 Although effective in chronic nuclear backache, where the dural symptoms are much milder, traction should never be used in acute nuclear lumbago. Experience shows that, if traction is applied on a patient who mentions the presence of ‘twinges’, considerable worsening of the condition for several days may be expected. The reason for this is not completely understood. Presumably the size of the bulge increases when the hydrostatic and osmotic conditions within the disc change during traction (see p. 420). If the lumbago is really hyperacute, which means that the dural symptoms are so intense that repeated and agonizing twinges force the patient to lie motionless, any attempt at manipulative reduction is unthinkable. It is obvious that manipulation cannot be done when the patient can hardly move or when it takes some minutes to roll from a prone to supine-lying position on the examination couch. In these cases, the only alternative to several weeks of bed rest is epidural local anaesthesia, which affords immediate and complete relief of symptoms over 1 or 2 hours. Curiously enough, and although the anaesthesia only works for 2 hours, there is lasting relief from the next day on. The injection probably has some long-term effect on the inflamed dura, rendering it less sensitive. Once the immobilizing twinges have been abolished, the patient is capable of getting up and travelling for manipulative reduction of the residual displacement. This combination of epidural local anaesthesia and manipulation is rapidly successful in nearly all cases of hyperacute lumbago.63 About 80% of all cases of low back pain relate directly to the intervertebral discs.64 Discodural backache presents a typical complex of symptoms and signs, both articular and dural. The mechanism of pain and dysfunction is exactly the same as described in lumbago, but the signs and symptoms are less acute because the discodural interaction is more moderate. Depending on which part of the dura is irritated, the pain is central or unilateral or shifts in location.65 Shifting pain is a common history and indicates that the lesion has moved from one side of the intervertebral joint to the other. Shifting pain in the back is one of the most characteristic phenomena in discodural backache. An alternating ache in the buttock, however, suggests sacroiliac arthritis rather than a disc problem (see Ch. 41). The localization of pain not only varies according to the site of compression of the dural tube but is also determined by the intensity of the stimulation. One of the rules of referred pain is that the stronger the stimulus, the further the pain will be referred. This has some practical bearings when it comes to evaluation of therapy: when the pain has originally been located in a buttock but, during a manipulative session, tends towards the centre and becomes paravertebral, this implies that the pain stimulus has been reduced and discodural contact is now less pronounced than it was. ‘Centralization’ of the pain is thus a good predictor of a successful outcome.66,67 The reverse change – pain moving more and more distally – indicates that the situation has worsened. Relation between posture/movement and pain is also important. In minor disc lesions, the ache probably depends entirely on the level of exertion. Any work involving stooping, lifting or sitting for too long is followed by pain, which may, however, be almost or completely absent at rest. In more advanced instances, particular positions are very painful or even impossible. It is obvious that contact will increase in positions and activities that increase intradiscal pressure and thus discodural contact. Bending forwards and lifting result in higher pressure than standing erect. To most patients with backache, walking around is more comfortable than sitting, because the latter imposes more load on the disc.68 Sitting without support causes yet more load and consequently more pain than does sitting with a reclined back rest.53 A paradoxical symptom complex is sometimes encountered. The dynamics of the disc, described above (see p. 420), suggest that intradiscal pressure should decrease and any bulge become less prominent when the patient lies down. Yet some patients have more pain during and after bed rest, wake during the night and have to get out of bed before dawn. The explanation is probably an increase in swelling when the external load diminishes. Diurnal changes in disc hydration and pressure have been demonstrated both in vitro69 and in vivo,70,71 and it is estimated that around 25% of the disc fluid is expressed and re-absorbed during each diurnal cycle.72 A small posterior bulge that becomes more hydrated swells to increase dural contact. This phenomenon is also mirrored in the diurnal changes in the range of the SLR; comparison of the range of SLR after recumbency and after 2 hours erect shows an increase in range of 10% or more.73 The characteristics of discodural pain are summarized in Box 33.2. A partial articular pattern is present on the four active movements. The degree of limitation is unequal in different directions (Fig. 33.8); if there is no limitation, some movements are painful at their extremes and some not. All these findings are typical of internal derangement – some movements increase the annular or nuclear bulge, so increasing dural contact, while others reduce it. Usually this is unequally limited (Fig. 33.8a). Alternatively there is pain at the end of one side flexion only, the other being full-range and painless. If side flexion away from the pain is the more difficult to achieve, manipulative reduction will almost certainly succeed, but in the reverse situation quick and lasting relief by manipulation is more uncertain. Sometimes there is a painful arc (Fig. 33.8d): momentary pain is experienced on moving the trunk from one side to the other. The arc may be quite extensive and is only overcome with considerable effort. Therefore the patient should be encouraged to continue movement and not stop the moment pain is felt; otherwise, the presence of an arc could be missed. Sometimes both side flexions are full and painless. This does not eliminate a disc protrusion but probably indicates that it is too small and too centrally localized to come in contact with the dura during side flexions. Only extension or flexion will then influence the pain and asymmetry is probably only shown by some momentary deviation, a painful arc during flexion or unilateral localization. Frequently, a painful arc is encountered, with a transient pain somewhere at mid-range (Fig. 33.8c, d). Alternatively, slight deviation may be seen at the midpoint of flexion. Careful observation is needed to detect this visible arc, of which the patient is usually unaware. A painful arc during flexion can be associated with a partial articular pattern but it can also be an isolated finding. It always means that a small fragment of disc tissue impinges momentarily against the dura mater. At the beginning of flexion, an increase in both intradiscal pressure and convexity of the posterior aspect of the intervertebral joint provokes discodural contact (Fig. 33.9). Flexion beyond the horizontal imposes more distraction than compression on the intervertebral joint. The backward pressure on the disc then decreases and is replaced by a more centripetal force on the disc, which is supported by the tightening of the posterior longitudinal ligament. The small posterior displacement is then removed from contact with the dura and pain ceases. It is extremely difficult to predict the natural history and therefore unwise to tell the patient that backache will very soon abate. Although it is true that most episodes are self-limiting,74 the disability often becomes chronic.75 Though an acute bout shows some tendency to spontaneous cure,76 recent research shows that the course of back pain is merely episodic, with repeated recurrences following an acute episode.77–79 A substantial minority of patients may not even experience resolution of their pain and disability, and suffer for years from chronic lower lumbar pain.80–83 One possible explanation for this type of backache is ‘bruising’ of the dura mater.84 The acute lumbago has induced inflammation of the dura mater. Although the disc displacement has receded after some time, the dura has remained inflamed, which results in continuous pain. Obviously this type of backache – chronic pain unaltered by posture or exertion and with a negative clinical examination – can also exist as the result of pain referred to the back from other (visceral) structures. This nocturnal backache often occurs in middle-aged people. It is best explained by an increase in intradiscal oncotic pressure at an early stage of degeneration. When the external load is diminished in the horizontal position, there is a considerable increase in water content. Expansion forces the disc against the pain-sensitive dura. Resumption of the upright position raises the hydrostatic pressure, water is extruded and the disc deflates, which alleviates the tension on the dura mater so that pain disappears.72 Because the pain is of dural origin, epidural injection is the treatment of choice and succeeds in about 70% of cases.63 Should the injection fail, ligamentous sclerosis is used, in order to stabilize the lower lumbar segments. Before specific treatment is given, a few questions must be answered: • Is the backache caused by an activity-related spinal disorder? • If this is the case, is the disorder a discodural interaction or not? When there is a clear combination of both articular and dural symptoms and signs, the answer is obvious. In moderate discodural backache, however, when the patient presents with articular signs only, it may be more difficult to make a certain diagnosis of internal derangement. However, a partial articular pattern always indicates a disc lesion, except in a few cases (see Ch. 39). A deviation, whether in the upright position or in flexion, signifies a protrusion. Also, the presence of a painful arc, whether during side or forward flexion, is the sign of a small posterior bulge. • What is the level of the lesion and what is the size and composition of the bulge? • Is the subluxated fragment an acute and occasional event, or does the patient have recurrent attacks of backache? How long does the disability last? Does the pain disappear completely between bouts or is there a continuous ache? • What is the degree of pain and how much is the dura inflamed? • What attitude does the patient have towards the problem? • Does the patient want to get better? Is there any compensation claim or does the patient show clear evidence of psychological disorder? (see online chapter Psychogenic pain). • Reduction of the displacement • Desensitization of the dura (in acute or gross inflammation of the dura, it is sometimes better to desensitize it in order to abate the pain instead of trying to move the disc back into place). If the displacement is annular, the treatment of choice is manipulative reduction. A nuclear displacement is an indication for sustained traction. Although the two techniques are, to some extent, interchangeable, some protrusions prove irreducible by traction, yet reducible by manipulation and vice versa. It is obvious that a protrusion composed of hard annular material will respond better to manipulation but that a soft nuclear bulge requires traction. Cyriax said45: ‘You can hit a nail with a hammer, but treacle must be sucked.’ If sufficient data on the onset of the complaints cannot be obtained and the choice of treatment is in doubt, manipulation should be tried first. If it fails, the patient should attend for traction from the next day on. If considerable improvement is achieved by manipulation but, despite further attempts, a residual displacement cannot be reduced, traction should be substituted so as to complete the process. The simple and easy-to-learn manipulation measures are usually speedily effective. Overall, acute backache is relieved by one session of manipulation in 46–57% of patients.85,86 As a rule, small annular displacements are cured by a single manipulative session. In larger protrusions, 2–4 sessions may be required. When the patient presents with a marked lateral deviation, up to four manipulation sessions are sometimes needed. Manipulation is successful after a small number of sessions or not at all. Hence, if the patient does not improve almost immediately and lastingly, it is unwise to continue treatment and daily traction should be used instead.
The dural concept
Hypothesis
Clinical evidence for insensibility of the disc
Clinical evidence for sensibility of the dura mater
The mechanism of dural pain is dual
The dural concept in the natural history of the ageing disc
Clinical syndromes
Lumbago
History
Annular lumbago
Nuclear lumbago
Clinical examination
Inspection
Spinal movements
Extension
Dural tests
Neck flexion
Straight leg raising (SLR)
Tests of conduction
Natural history
Treatment
Nuclear lumbago
Hyperacute lumbago
Backache
History
Clinical examination
Spinal movements
Side flexion
Painful arc
Natural history of discodural backache
Particular types of backache
Bruised dura
Nocturnal or morning backache
Treatment
Reduction
Manipulation