The Blatt Capsulodesis
Charles A. Goldfarb
Richard H. Gelberman
Indications and Contraindications
Scapholunate dissociation, the most common cause of carpal instability, results from an injury to the scapholunate interosseous ligament. Classically, the injury results in a loss of the normal relationship between the scaphoid and the lunate, as the scaphoid tends to palmarflex and the lunate tends to dorsiflex (owing to the extension moment of the triquetrum). Whereas an injury to the scapholunate ligament is a prerequisite to scaphoid flexion, other supporting ligaments (e.g., the dorsal radiocarpal, the dorsal intercarpal, the radioscaphocapitate, and the scaphotrapezial), together with the nature of the bony anatomy of the radiocarpal joint, contribute to stability also and determine whether the scaphoid maintains its normal posture or flexes. Scaphoid flexion and scapholunate diastasis that occurs only with wrist motion or provocative maneuvers is termed dynamic instability; an abnormal posture of the scaphoid and lunate at rest is termed static instability. In dynamic instability, the plain radiographs are normal and the diagnosis is made on clinical examination when tenderness is elicited over the scapholunate interosseous ligament and a positive Watson scaphoid shift sign is seen (see below). Another diagnostic aid for dynamic instability is the clenched fist radiograph that may demonstrate scapholunate widening with axial loading. In static instability, plain radiographs are abnormal and the diagnosis is made with any one of the following criteria (Figs. 20-1 and 20-2):
A scapholunate angle of more than 70 degrees, a scapholunate angle more than 15 degrees greater than the contralateral wrist, or a radiolunate angle greater than 10 degrees on the lateral radiograph (a normal scapholunate angle is 47 degrees, normal radiolunate is 0 degrees)
A scapholunate gap of 3 mm or greater on the posteroanterior (PA) radiograph
A decrease in the scaphoid ring to scaphoid proximal pole distance to less than 8 mm on the PA radiograph.
The Blatt dorsal capsulodesis uses a leash of dorsal wrist capsule to tether the distal pole of the scaphoid and prevent excessive scaphoid flexion. (Fig. 20-3A,B) When effective, the painful clunking of the scaphoid against the radius is prevented and the risk of progression of the instability pattern (and, theoretically, the development of arthrosis) may be decreased. The primary indication for dorsal capsulodesis is dynamic scapholunate instability after the failure of nonoperative treatment. Our conservative management protocol includes splinting of the wrist in 20 degrees of extension, activity modification, and oral anti-inflammatory medications. Although we have found that most patients with symptomatic instability ultimately require operative intervention, a 12-week trial of nonoperative management is recommended for all patients with dynamic instability.
Management of static scapholunate dissociation is controversial. We treat an acute injury (<3 weeks old) to the scapholunate ligament with ligamentous repair through a dorsal approach and do not perform a concomitant capsulodesis. Although some authors have recommended dorsal capsulodesis and scapholunate ligament repair for chronic, static deformities (1), we find the dorsal capsulodesis less than optimal in these cases.
Contraindications to the use of dorsal capsulodesis include a static scapholunate dissociation in which a bony reduction cannot be easily obtained, an injury to the scapholunate ligament as part of a larger injury pattern (perilunate injury), and the presence of arthrosis.
 Figure 20-1 In the posteroanterior (PA) radiograph of this static scapholunate instability, the scapholunate gap is abnormal at 4 mL and the ring to proximal pole distance is decreased to 5 mm. |
 Figure 20-2 In a lateral wrist radiograph of the same patient, the scapholunate angle measures 85 degrees, significantly higher than acceptable. |
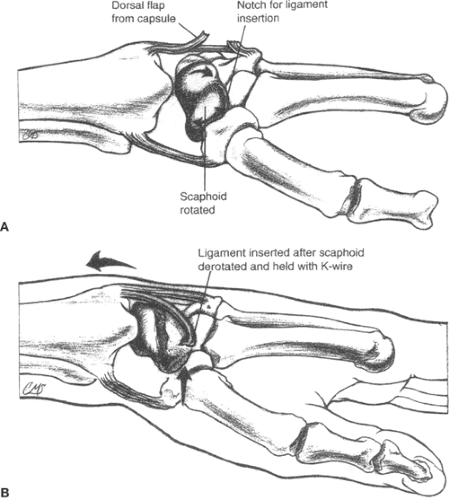 Figure 20-3 A, B: A graphic representation of the concept of dorsal capsulodesis to stabilize the scaphoid from excessive palmar flexion. |
Additionally, an occult dorsal wrist ganglion may present in a similar fashion to dynamic scapholunate instability, with dorsal wrist pain and often with a positive Watson scaphoid shift test. An ultrasound is used to identify the ganglion and these patients may be treated with ganglion excision alone.
Preoperative Planning
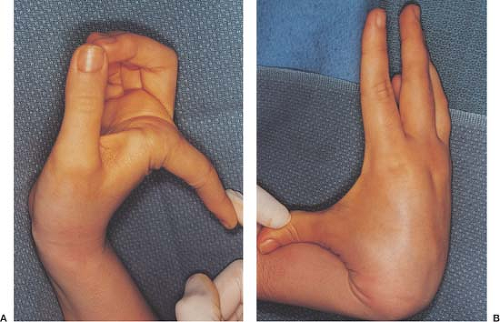
The most important aspect of preoperative planning for dorsal capsulodesis is the accurate diagnosis of dynamic scapholunate instability, based on history, physical examination, and radiographic studies. Patients with dynamic scapholunate instability complain of dorsal wrist pain and clicking or clunking of the wrist with motion. A traumatic incident, usually a fall on an extended wrist, may be recalled. The physical examination includes a global assessment of joint laxity (Fig. 20-4A,B) and a careful examination of the contralateral wrist for asymptomatic instability. Typically, the affected wrist examination reveals dorsal scapholunate interval tenderness and a positive Watson scaphoid shift test.
Perform the Watson scaphoid shift test (Fig. 20-5A,B) with the patient sitting with the involved elbow on the examination table and the forearm in neutral rotation and perpendicular to the table. While seated opposite the patient, place your thumb over the scaphoid tuberosity with the index and long fingers overlying the dorsal distal radius. While applying an axial load and radially deviating the wrist, apply a dorsally directed pressure to the scaphoid tuberosity, palpating for a dorsal clunk and attempting to elicit dorsal wrist pain in the area of the scapholunate interosseous ligament (2,3). The test is positive when a palpable clunk and associated pain along the dorsum of the wrist in the area of the scapholunate interosseous ligament are noted.
Radiographic assessment includes standard PA and lateral radiographs, which, by definition, should be normal for dynamic instability. A stress radiograph, a PA radiograph in neutral with a clenched fist, is also obtained and may demonstrate widening of the scapholunate interval. Cineradiography, arthroscopy, and arthrogram are all more definitive means of confirming a diagnosis. In a patient with dorsal wrist pain localizable to the scapholunate interosseous space, a history of painful clicking, a positive Watson test, normal plain radiographs, and a failed trial of conservative treatment, operative intervention may be undertaken without additional testing.
Surgical Technique
The patient is seen in the preoperative holding area to confirm the operative side and sign the operative site.
Place the patient supine on the operating room table with the affected extremity on a hand table.
Administer a regional anesthetic, place a nonsterile tourniquet, and perform a sterile preparation of the extremity.
After draping, examine the area under anesthesia to confirm the diagnosis.
Palpate and mark the radial styloid and Lister’s tubercle and note the scapholunate interval 1 cm distal to the tubercle.
Mark a 3-cm transverse incision (Fig. 20-6) and incise at the level of the styloid in the dorsal wrist crease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree