The Athlete’s Wrist
CASE PRESENTATION
A 16-year-old varsity lacrosse player re-presents for persistent wrist pain on her dominant right side. Initially the pain arose with stick handling when in her attack position. Now discomfort was occurring when opening jars, doors, and carrying her books in school. Initial treatment included a strengthening therapy program starting 6 weeks ago. She now has equivalent pinch-and-grip strength compared to her contralateral side. Her exam reveals pain with supination beyond 30 degrees, ulnocarpal compression pain, and an asymmetric click with rotatory stress. She is symmetrically moderately ligamentously lax with scapholunate, lunotriquetral, and midcarpal stress testing. Radiographs reveal symmetric neutral ulnar variance.
CLINICAL QUESTIONS
What conditions and injuries give rise to sports-related wrist pain?
What are the differential diagnosis and work-up for chronic wrist pain?
How often is surgical intervention necessary?
How are triangular fibrocartilage complex (TFCC) tears classified?
Which types of tears are most common in adolescents?
What are the results of TFCC repair in children and adolescents?
How are scapholunate ligament tears classified?
Which patients are at risk for chondral injuries?
Is arthroscopic debridement of partial ligament tears and/or chondromalacia successful?
THE FUNDAMENTALS
Etiology and Epidemiology
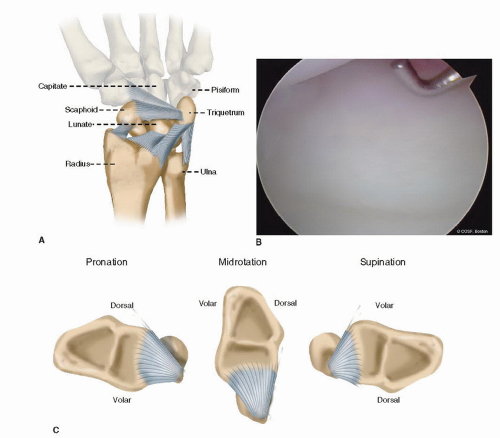
Soft tissue stability of the wrist is conferred by intra-articular intercarpal, radiocarpal, and ulnocarpal ligaments as well as distal radioulnar ligaments and the TFCC.1 The proximal carpal row (scaphoid, lunate, triquetrum) is interconnected by scapholunate and lunotriquetral ligaments. The scapholunate ligament has three portions: dorsal, proximal, and palmar. The dorsal portion is the main stabilizer between the scaphoid and lunate, while the palmar portion of the lunotriquetral ligament is the main stabilizer between those two carpal bones. Carpal instability can be dynamic, with normal radiographs, or static, in which the carpal gap and malalignment can be seen on plain radiographs. Both static and dynamic instabilities can cause pain with activity.
The TFCC helps to stabilize the ulnar side of the wrist and the distal radioulnar joint (DRUJ). It consists of an articular disc, meniscal homologue, volar and dorsal radioulnar ligaments, ulnocarpal (ulnolunate and ulnotriquetral) ligaments, and deep surface of the extensor carpi ulnaris (ECU) sheath. It extends from the medial radius above the sigmoid notch to the base of the ulnar styloid (Figure 42-1). The vascularity of the TFCC is from the periphery, similar to a knee meniscus. As ulnar variance becomes more positive, axial load through the ulnocarpal joint, and stress on the TFCC, increases. The volar distal radioulnar ligaments and the TFCC prevent dorsal displacement and are most taut in pronation. Conversely, the dorsal distal radioulnar ligaments and the TFCC prevent volar displacement and are taut in supination.
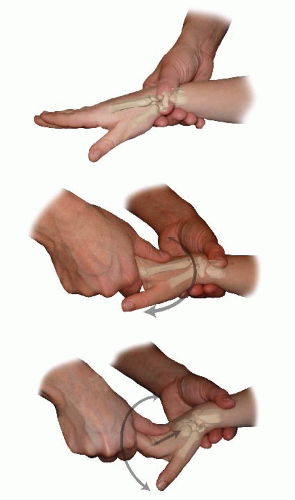
Clinical Evaluation (Figure 42-2)
Golf is a game in which you yell “fore,” shoot six, and write down five.
—Paul Harvey
The spectrum of sports-related adolescent wrist pain is broad2, 3 and 4 and includes, among others, overuse syndromes, stress fractures (see Chapter 39)5,6 (Figure 42-3), wrist sprains, muscle imbalance, ganglia, hyperlaxity, dorsal impaction,7 pain syndromes, inflammatory processes, and specific chondral and ligamentous injuries.8, 9, 10, 11 and 12 All patients should have plain radiographs as a part of clinical evaluation. Obviously, distal wrist and ulna, carpal (particularly scaphoid), and metacarpal fractures are a major part of wrist-area injuries in sports. Evaluation and care of fracture dislocations are covered in Chapters 34 and 35.
Pain is often diffuse (see Coach’s Corner). The opposite nonpainful wrist is used for comparison in all aspects of the physical exam. It is often best to start there, so the patient knows what you are going to do and establishes some trust. Specific locations (such as the ulnocarpal joint) can be diagnostic for anatomic injury (such as a TFCC tear). The presence of skin dystrophy and/or muscle atrophy is assessed before physical palpation or testing. Scaphoid, scapholunate, lunotriquetral, ulnocarpal, distal radioulnar, and volar radiocarpal joint areas are palpated in sequence. Palpation for ganglia in the usual locations (dorsal scapholunate, volar radiocarpal) is performed. Standard resistive strength (intrinsic and extrinsic), sensibility (light touch and two-point discrimination), and range-of-motion (passive and active) testing are performed on each patient to check for neuropathy, tenosynovitis,13 tendinopathy, and muscle injuries.14 Provocative testing for asymmetric ligamentous instability is necessary. Watson scapholunate shift, Lichtman midcarpal shift, lunotriquetral ballottement and shear, and ulnocarpal compression with forearm rotation are standard aspects of the exam. The presence of asymmetric clicking
or clunking, particularly when it reproduces the patient’s pain, guides diagnosis. Injection of local anesthesia in the maximum pain area can be helpful, but many adolescents are resistant to needles. Ultrasound imaging of a mass can distinguish ganglia.
or clunking, particularly when it reproduces the patient’s pain, guides diagnosis. Injection of local anesthesia in the maximum pain area can be helpful, but many adolescents are resistant to needles. Ultrasound imaging of a mass can distinguish ganglia.
Radiographs are obtained to assess for abnormalities such as physeal stress fractures (gymnast’s wrist),15 Kienbock’s avascular necrosis of lunate, unhealed fractures (scaphoid nonunion, hook of hamate nonunion,16 ulnar styloid nonunions and associated TFCC tears), carpal coalitions, and inflammatory arthritis, among others. Treatment is appropriately applied with each condition with a positive radiograph. With normal radiographs and a nonspecific exam, which is common, you are quickly at the crossroads of starting with the three R’s (reassurance, rest, and rehabilitation) or proceeding directly to an magnetic resonance imaging (MRI) scan or wrist arthroscopy. Unless the exam is specific for an anatomic injury, we always start with rehabilitation. Approximately 80% of our highly specialized referral practice fits that pattern and can still be successfully treated with resistive strengthening. It is rare we use casting for these patients but often use intermittent splinting programs. We use strengthening not only as treatment but also as a part of our evaluation. Grip-and-pinch strength on both sides is monitored by a therapist during intrinsic and extrinsic strengthening (elastic bands and therapeutic putty) with the wrist stabilized in neutral position. We stress the value of a home program that incorporates multiple sessions a day with weekly supervised care. We reassure them that there is a difference between “hurt” and “harm” and that we want them to work through the “hurting” pain without fear of causing permanent damage.
If all goes well, by 6 weeks the patient will demonstrate marked reduction in pain and near-normal strength. By 12 weeks, the problem is often resolved. If the problem persists, you then have to decide on more thorough musculoskeletal evaluation and treatment or referral to a pain specialist or nontraditional caregiver. The use of MRI scans can be diagnostic but also confusing depending on the threshold of signal abnormality the radiologist uses to make a reading.17, 18 and 19 At our center, there are many more false negatives than false positives. The improving sequences narrow the gap of specificity and sensitivity but also make it imperative that we keep pace with the changing technology. The addition of arthrographic iodinated contrast material expands the diagnostic accuracy but, again, involves needles. In the remaining subset of patients with persistent problems, MRI scans often enable us, the patient, and the family to move definitively to surgery or away from orthopaedic interventions.
Surgical Indications
A limited number of adolescent patients presenting for evaluation of sports-related nonosseous wrist pain need surgery. As noted above, most can be treated with the three R’s: reassurance, rest, and rehabilitation. However, there are athletes with focal soft tissue and cartilaginous disorders that benefit from surgery. These include (1) scapholunate and lunotriquetral ligament tears;20 (2) chondral impaction injuries; (3) TFCC tears; (4) an unstable DRUJ;
(5) arthroscopy for diagnostic dilemmas;21 and (6) rare, chronic tendinopathies. In addition, resection of the terminal branch of the posterior interosseous nerve at its insertion into the wrist can be a part of surgical management for chronic, recurrent conditions.
(5) arthroscopy for diagnostic dilemmas;21 and (6) rare, chronic tendinopathies. In addition, resection of the terminal branch of the posterior interosseous nerve at its insertion into the wrist can be a part of surgical management for chronic, recurrent conditions.
SURGICAL PROCEDURES
Do you know what my favorite part of the game is? The opportunity to play.
—Mike Singletary
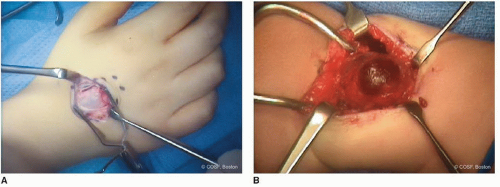
• Ganglion Excision (Figure 42-4)
A dorsal ganglion, whether small or large, can cause symptoms with wrist arc of motion, especially dorsal impaction. However, not all ganglia are symptomatic. They can be associated with carpal instability, so excision alone may not resolve symptoms. They can be excised open or arthroscopically. An open procedure is performed through a transverse incision over the dorsal ganglion. The origin of the ganglion is typically the scapholunate ligament. The dorsal veins and extensor tendons are protected with dissection. Circumferential dissection requires care not to rupture the ganglion before isolation of the stalk. Failure to remove the stalk is an invitation to recurrence. A square or circumferential dorsal capsulectomy is performed, incorporating the ganglion stalk. Some have advocated an inside-out removal of the stalk by opening the ganglion and following the stalk from the inside down to the origin. This is an open adaptation of the arthroscopic technique. After capsulectomy and stalk removal, the area of origin is debrided with a minirongeur and cauterized without impairing ligament integrity. The tourniquet is deflated to inspect for any bleeding. After local anesthesia injection and layered closure with absorbable suture, we usually immobilize in a bivalved cast or splint for 2 weeks followed by unrestricted activity. Stiffness and loss of strength are usually not a problem with these children. If they are ligamentously lax, we have them do a supervised strengthening program to eliminate that element of their pain as well.
Osterman and Raphael reported the arthroscopic removal of dorsal ganglia, and many now follow this technique.22 There may be cosmetic and rehabilitation benefits, especially in adults. Recurrence rates now appear to be similar, <5%.23




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree