Chapter 26 The Assessment and Management of Posterolateral Instability
Introduction
The high congruency of the bony structures forming the elbow, make the elbow an inherently stable joint. The stabilizing system provided by the osseous architecture and the balanced intact musculature which provides dynamic or active joint stability, is supported by strong capsule-ligamentous structures on the lateral and medial side of the elbow joint.1–6 In full flexion and extension of the elbow, the primary stability is provided by the osseous articulation, whereas the capsule-ligamentous stabilizers are the primary stabilizers in all semi-flexed positions, providing maximal stability at 90° of joint flexion.3,5–8
The most common cause of ligamentous injury of the elbow joint resulting in instability is an elbow dislocation. In adults, the elbow joint is the second most commonly dislocated major joint after the shoulder and is the most commonly dislocated joint in the paediatric age group. The incidence of elbow dislocation in the general population is estimated to be 6/100 000.4
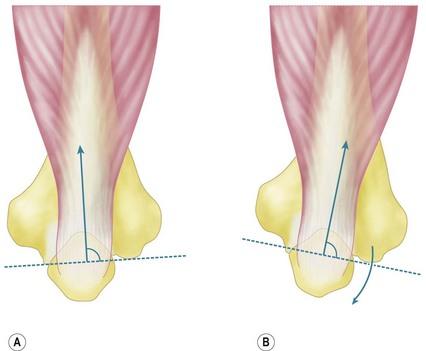
Posttraumatic chronic ligamentous instability can be divided into medial or valgus instability, postero-medial instability and posterolateral rotatory instability (PLRI). As the signs and symptoms of these entities are often subtle, the examiner must have a high index of suspicion and a thorough knowledge of the symptoms and expected findings at physical examination in order to make the diagnosis. Persistent insufficiency of the lateral collateral ligament complex (LCLC) (especially the ulnar part – the lateral ulnar collateral ligament (LUCL)) results in PLRI (Fig. 26.1A). Insufficiency of the medial collateral ligament (MCL), in particular the anterior part or AMCL, results in valgus instability (Fig. 26.1B).
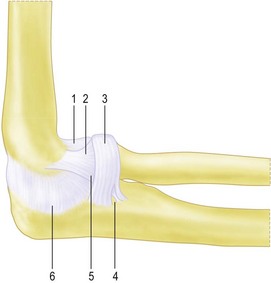
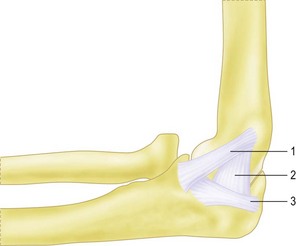
Figure 26.1 (A) The lateral collateral ligament complex (LCLC). This complex consists of:
2.Radial collateral ligament (RCL).
4.Interval between annular ligament and lateral ulnar collateral ligament (LUCL).
(B) The medial collateral ligament complex (MCLC). This complex consists of:
1.Anterior medial collateral ligament (AMCL).
2.Posterior medial collateral ligament (PMCL).
Background/aetiology
During a posterolateral dislocation of the elbow joint, rupture of the ligamentous complex occurs in a circle from lateral to medial, as described by O’Driscoll et al; in stage I, the LUCL is disrupted; in stage II, the other lateral ligamentous structures as well as the anterior and posterior capsule are torn. In stage III disruption of the medial collateral ligament can be partial with disruption of the posterior bundle only (IIIA) or complete (IIIB).4
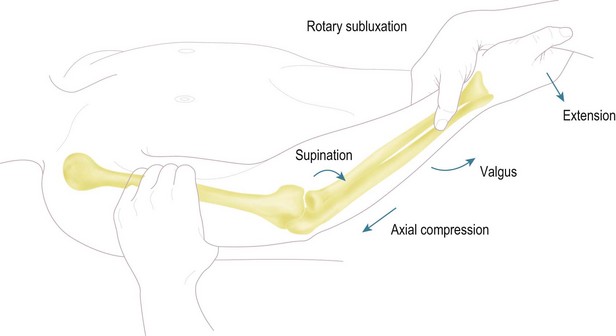
In a cubitus varus deformity the triceps contraction has been hypothesized to result in asymmetrical loading of the joint resulting in attenuation of the LCLC (Fig. 26.2). If surgical reconstruction is considered in these cases of complex instability a LCLC reconstruction alone will not restore stability. A valgus osteotomy to correct the varus deformity, in addition to a LCLC reconstruction, should be considered and is essential if the varus deformity is more than 20°. Experimental data in cadavers have shown increased strain on the LCLC with more than 25° of varus angulation and increased opening of the joint line space with more than 20° of varus angulation. In the preoperative work-up an assessment of the malunion in three directions is mandatory. Evaluation with a computed tomography (CT) scan of the injured and the uninjured complete humerus is necessary to determine the rotational deformity.
During surgery, the deformity is corrected in valgus, flexion or extension and rotation, depending on the preoperative assessment. Finally, iatrogenic injury as a result of surgery to the lateral side of the elbow or repeated steroid injections can result in injury to the LCLC (Table 26.1).
Table 26.1 Aetiology of lateral collateral ligament insufficiency
| Trauma | Postero-lateral dislocation of the elbow joint |
| Fracture dislocation | |
| Elbow subluxation | |
| Sprain/varus injury | |
| Chronic attenuation | Longstanding cubitus varus deformity with or without trauma |
| Longstanding inflammation of the elbow | |
| Chronic crutch users | |
| Iatrogenic | Following lateral elbow surgery, i.e. tennis elbow release or arthrolysis |
| Repeated steroid injections |
Iatrogenic lesions primarily occur after release of the common extensor tendon to treat chronic lateral epicondylitis. The ligament complex is particularly at risk in cases where ‘minimal invasive techniques’ or percutaneous techniques have been used as the surgical procedure. It is of utmost importance that surgeons are aware of the ligamentous anatomy, in order to preserve the ligament during elbow surgery. If transsection of the LCLC occurs during surgery or release of the insertion of the LCLC is necessary during a surgical procedure, the surgeon should repair the ligament as anatomically as possible. The LCLC is the primary capsular-ligamentous stabilizer of the elbow joint to varus and external rotation.3–9
The mean length of the LCLC from its origin to the annular ligament is 20 mm, and the width is approximately 8 mm.10 The insertion point on the lateral epicondyle is at the isometric point for the flexion and extension axis, and therefore the ligament is uniformly taut in the entire flexion axis.2,10 The functional anatomy of the ligament indicates that there is a superior and inferior part to the ligament and only complete division induces clinically significant joint laxity.5,6,8 The ligament complex is covered by the anconeus muscle, the supinator tendon and the musculo-tendinous insertion of the extensor carpi ulnaris and the extensor digitorum.9,10 Cohen and Hastings showed that the musculo-tendinous insertion of the extensor carpi ulnaris and the extensor digitorum covered the ligament and provided an additional stabilizing effect for the LCLC.9
A broad band originates from the undersurface of the lateral epicondyle and inserts fan-shaped into the annular ligament. This band constitutes the LCL and the LUCL. The fibres of the LUCL component, being the most posterior, pass through the annular ligament and insert on the ulna with fibres from the most inferior part of the annular ligament, inconsistently named the accessory collateral ligament.2,8,9,11,12 The insertion on the proximal part of the supinator crest, is separated from the annular ligament by a small triangular space.5,8,11 The annular ligament originates from the anterior and posterior margins of the lesser sigmoid notch and passes around the radial head, maintaining contact between the radial head and the ulna.10 In PLRI, the proximal radioulnar joint is intact. Laxity or avulsion of the ulnar part of the lateral collateral ligament leads to an increase in external rotation of the ulnohumeral joint.5 This increase in external rotation results in a secondary posterior subluxation of the radial head. This secondary subluxation, with an intact proximal radioulnar joint, must be differentiated from isolated posterior head subluxation with disruption of the proximal radioulnar joint and an intact ulnohumeral joint.13
Associated injuries with elbow dislocations are common; radial head and neck fractures occur in 5–10%, avulsions of fragments from the medial or lateral epicondyle occurs in 12% and fractures of the coronoid process occur in 10% of all dislocations. The reverse is also true and fractures around the elbow can be associated with ligamentous injury. Van Riet and Morrey in a study of an American population noted injury to the LCLC in 35 of 88 patients with radial head fractures14 and similar results were also noted in a Dutch study.15 The incidence of associated, ligamentous injuries in radial head fractures is high, especially in Mason type 3 and 4 injuries. The treating physician should be aware of this and should perform a thorough physical examination of the upper limb in every patient with a radial head fracture.
Presentation, investigation and treatment options
Clinical signs and symptoms of patients with an insufficiency of the LCLC vary depending on the severity of the instability, associated injuries such as radial head or coronoid fractures, and activity levels. In rare cases of LCLC insufficiency recurrent frank elbow dislocations occur. However, more often the symptoms and clinical signs of insufficiency are more subtle. It is important therefore, if an accurate diagnosis is to be made, that the surgeon is fully aware of the clinical symptoms and signs of LCLC insufficiency.16,17
Physical examination
The alignment of the elbow joint is examined in the anatomical position with the hands supinated and elbows extended. Axial alignment is assessed with the ‘carrying angle’, which is formed between the humerus and the forearm in the coronal plane. The average carrying angle is 10° for men and 15° for women although much variation exists based on age, race, sex and body weight.18–21
The medial and lateral ligament complexes should be tested in all patients. Pure varus stress does not allow reliable assessment of the lateral ligamentous structures. Several other physical examination manoeuvres have been described to test the LCLC.22 During the clinical examination, which will usually have a normal range of motion, the patient will often describe lateral elbow pain during forced external rotation in the semi-flexed elbow, or during the pivot shift manoeuvre described by O’Driscoll.16 This test involves applying a valgus, supination and axial load force to the elbow. As the elbow is extended, the radial head and ulna sublux from the humerus. During flexion the elbow relocates (Fig. 26.3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree