Chapter 43 Total Elbow Arthroplasty
Background
Although elbow replacements have been undertaken for many years, they were initially only performed for either major trauma or tumour reconstruction. It was not until the 1970s that significant numbers of elbow replacements began to be performed. Many of the early designs had humeral and ulnar components linked by a rigid hinge that resulted in a very high early failure rate. As a consequence later designs incorporated a loose or sloppy hinge rather than a rigid linkage. Current examples include the Coonrad–Morrey, GSB and Discovery prostheses. Parallel to this change a group of prostheses were developed that had no linkage mechanism between the humeral and ulnar components. These became known as ‘unlinked implants’. Examples include the capitellocondylar, Souter–Strathclyde and Kudo. More latterly implants have become modular, allowing them to be inserted as either linked or unlinked devices (Acclaim, Latitude) (Table 43.1).
Table 43.1 Examples of implants currently available
| Unlinked | Linked | Modular |
|---|---|---|
| Capitellocondylar | Coonrad–Morrey | Acclaim |
| Souter–Strathclyde | GSB III | Latitude |
| Kudo | Discovery |
Indications and implant types currently available
When considering elbow joint design it is important to understand constraint, especially as unlinked implants are often referred to as unconstrained devices. The Oxford English Dictionary defines constraint as ‘limitations imposed on motion’. Whilst soft tissue structures, particularly the collateral ligaments, contribute significantly to stability around the normal elbow, there is some inbuilt incongruity of the articular surfaces that allows 6–8° of varus valgus. Any implant design that does not have this inbuilt incongruity is more constrained even if it is unlinked. Indeed such an implant can be more constrained than a linked implant with a sloppy hinge. As might be expected, there is significant variation between implants.1
Due to the high failure rate of the original surface replacements, modern implants have a stem on both the humeral and ulna components. In addition, most components are cemented in place. Humeral fixation can be augmented in a number of ways of which an anterior flange is perhaps the most popular. It is thought that this produces better force transfer across the humerus, although recently this has been disputed by Quenneville et al.2 Others3,4 have used a wedge design for the humeral component, the edges of which sit in both supracondylar ridges and resist rotation forces. In addition implant fixation has been improved by the use of better cementing techniques which include cement restrictors (bone blocks or manufactured devices), bone preparation and pressurized cement insertion.
With regard to ulnar components, all implants must accommodate the normal valgus angulation of the ulnar stem relative to the olecranon fossa. This makes the provision of separate implants for left and right sides essential.5 For most unlinked implants the ulnar component is the site of the high-density polyethylene. This may be cemented directly into bone as in the Souter–Strathclyde prosthesis, although more recent designs frequently incorporate a metal backing.
Implant stem length varies in different prostheses and may affect long-term survival of the arthroplasty. Using the Souter–Strathclyde prosthesis, Trail et al,6 showed that when the 7 cm humeral stem was compared with the 3.5 cm stem, the longer stem had a lower incidence of loosening.
Finally, the long-term outcome of any elbow arthroplasty depends not only on the implant itself but also on the skill of the surgeon. The effect of intraoperative placement and alignment of the components was analysed by Shah et al7 who found that for the Souter–Strathclyde prosthesis correct alignment and positioning of the humeral implant was crucial to its long-term survival. Indeed there was little latitude for malalignment. While this is essential for unlinked implants to avoid the risk of dislocation, it is obviously important that all implants are inserted in a satisfactory and reproducible manner. To this end, many of the newer designs have a full set of instrumentation allowing bone resection to be undertaken in a standard fashion.
Surgical techniques and rehabilitation
A number of surgical approaches for elbow arthroplasty have been described in Chapter 6. The technique utilized, however, generally depends on surgeon preference and particularly training, as well as the type of implant being inserted. The author’s personal preference is a technique that has evolved at Wrightington Hospital over the last 20 years. This is based on a posterior approach, which involves taking down a tongue of triceps.
The operation is performed in a laminar airflow theatre under general anaesthesia and with an inter-scalene block. The patient is placed in the lateral decubitus position with the arm suspended over a gutter (Fig. 43.1). A high tourniquet is applied allowing access to the elbow joint and distal humerus. The patient’s position should not impede the surgeon placing the arm in full extension and flexion during the surgical procedure. Prophylactic antibiotics are administered prior to inflation of the tourniquet in order to reduce the risk of infection.
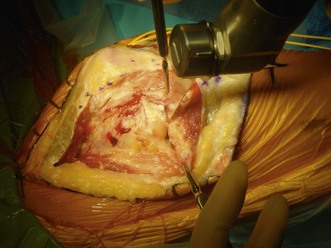
With the triceps exposed, a longitudinal incision is made just to the radial side of the midline again avoiding the tip of the olecranon. The incision is carried distally to expose the radial head (Fig. 43.2), which is routinely excised proximal to the annular ligament. The triceps and its attachment to the olecranon and distal ulna are then reflected as one piece. This is facilitated by using a sharp osteotome, particularly over the tip of the olecranon. The whole flap is then reflected medially exposing the fat pad and dorsal capsule of the elbow joint. Whilst the fat pad is retained, the capsule is excised. The tip of the olecranon is also removed. With further release of the posterior parts of the medial and lateral collateral ligaments, the elbow is dislocated (Fig. 43.3). This is further aided by undertaking a coronoid osteotomy and, if appropriate, releasing the anterior capsule. At the end of this part of the procedure, the only structures intact are the anterior parts of both collateral ligaments. The importance of these structures has been demonstrated in a number of studies.8,9
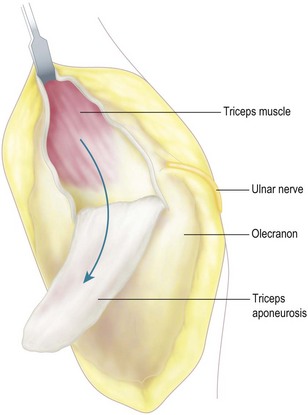
The original surgical approach that I used involved the same skin incision but gained access to the elbow joint by taking down a distally based flap of the triceps tendon (Fig. 43.4). Distally the incisions were extended to release the posterior parts of the medial and lateral collateral ligaments. The dorsal capsule was then incised and the elbow joint exposed. Whilst this approach was used successfully for many years, it undoubtedly resulted in some ongoing weakness of the triceps tendon which is why I no longer use it routinely. The only indication now would be if there was a significant loss of flexion preoperatively and at the end of the procedure lengthening of the triceps tendon was required.
An alternative lateral approach is favoured by some surgeons.10 This is based on a modified Kocher approach. The operation is performed under general anaesthesia with the patient in the lateral position. A tourniquet is used and the patient given prophylactic intravenous antibiotics. Ulnar nerve decompression, if necessary, is undertaken through a separate medial incision.
Ljung et al11 reported a high incidence of ulnar nerve palsy with this approach but there were few incidences of instability.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree