Chapter 16 The Management Options for Adult Distal Humeral Fractures
Introduction
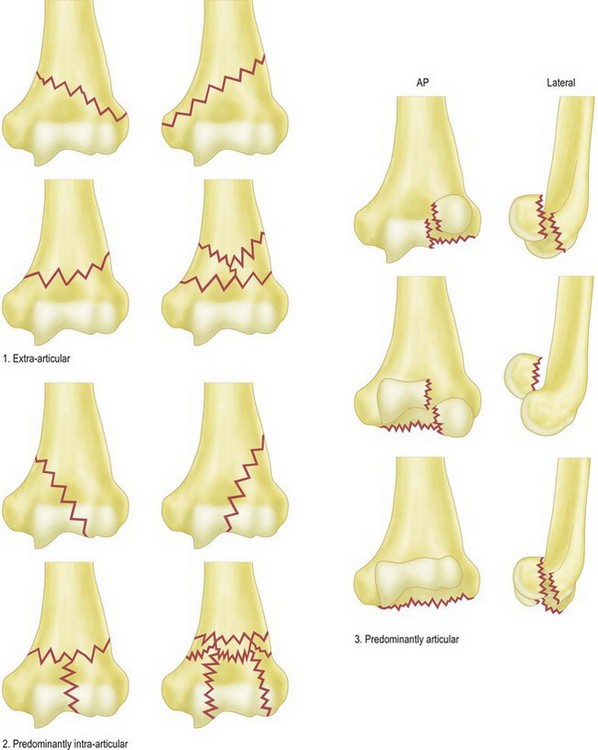
The humerus flattens and widens distally, with the maximum width between the epicondyles. The distal articular segment is held by the medial and lateral columns of thick cortical bone. A thin plate of bone between the columns constitutes the olecranon fossa posteriorly and the coronoid fossa anteriorly. This accommodates the olecranon and coronoid processes on extension and flexion respectively. The medial column diverges from the humerus at an angle of 45° and the proximal two-thirds are made of thick cortical bone, but the distal part is composed of soft cancellous bone. The triangular shape of the medial column enables screw placement for fracture fixation. The lateral column diverges from the humeral shaft at about 20° and has cortical bone similar to the medial column and also allows good fixation for screws. The distal part of this column is complex, with soft cancellous bone. The capitellum forms part of the lateral column.1,2 It has a curved anterior articular surface that articulates with the radial head. Posteriorly the surface is non-articular and therefore can be used for screw placement, although care should be taken not to penetrate the articular surface (Fig. 16.1A, B). The common extensor origin from the lateral column and the flexor origin from the medial column are responsible for fracture fragment rotation following injury.
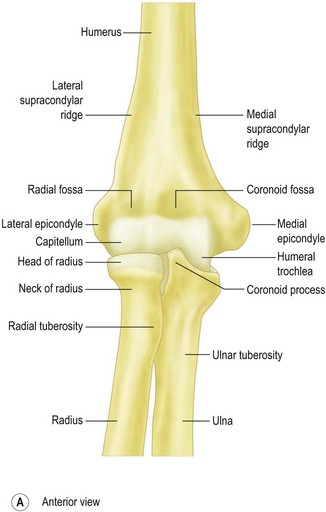
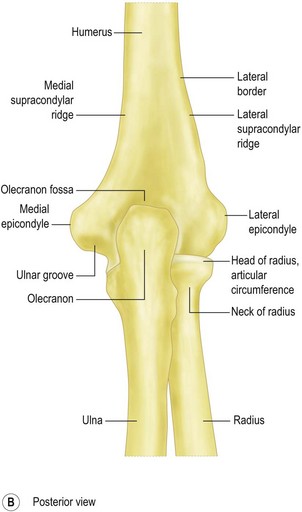
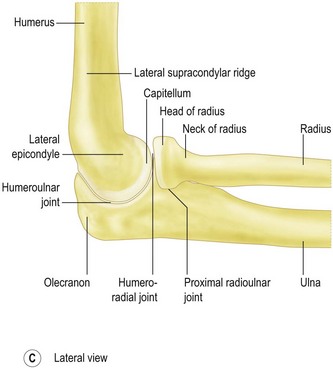
Figure 16.1 The anatomy of the distal humerus.
From Ross LM, Lamperti ED, consulting eds. Thieme atlas of anatomy. Georg Thieme: Stuttgart; 2006.
The articular portion projects anterior to the shaft of the humerus at about 40° in the sagittal plane; hence it is not well exposed through a posterior approach (Fig. 16.1C). It also has a valgus angulation of 4–8° to the shaft in the coronal plane.3 Restoring the articular anatomy and stabilizing the two columns without impingement of the fossae by metalwork is the key to successful surgical management of these complex injuries.4
Background/aetiology
Distal humeral fractures have a bimodal age distribution, affecting the young (high energy) or the elderly (low energy). Peaks of incidence have been noted in males aged 12–19 years and in females aged 80 and older. The most common mechanism of injury is axial loading of the distal humerus, by a simple fall. The next most common causes of fractures are road traffic accidents and sport.5
Fractures of the distal humerus account for approximately 2–6% of all fractures and about 30% of all elbow fractures.6 One epidemiological study from Finland showed that the age-adjusted incidence of osteoporotic fractures of the distal humerus increased, from 12/100 000 women in 1970 to 28/100 000 women in 1995 and it predicts a threefold increase by the year 2030.7
Classification
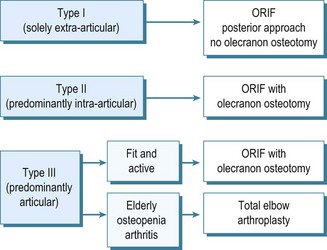
Various classification systems have been proposed for distal humeral fractures. In 1969 Riseborough and Radin developed a system of classifying T-shaped intercondylar fractures of the distal humerus based on the degree of fragment displacement, rotation and comminution.8 The AO group devised a classification system dividing the distal humerus into three types based on fracture lines lying extra-articularly, intra-articularly with or without involvement of a single column, and intra-articularly involving both columns. Stepwise progression into grouping and subgrouping of these fractures is dependent on the site of the fracture lines and the degree of fracture comminution. Fractures that do not fall into any of the three types or nine groups are labelled type D or .4, respectively.9 Later, Mehne and Jupiter developed a classification system based on three broad groups of fractures. Intra-articular fractures are subdivided into those with either single-columnar or bicolumnar involvement or those involving the capitellum or trochlea. Extra-articular, but intracapsular, fractures are also subdivided depending on the proximity of the fracture to the joint. Epicondyle fractures represent extra-articular fractures in this classification.1 In an assessment of these classification systems, Wainwright et al concluded that they were neither reliable nor reproducible, and thus their usefulness in decision making and comparison of outcomes was questionable.10 More recently, a clinically useful classification for fractures of the distal humerus has been developed and validated.11 This classification system has three main components – extra-articular, predominantly intra-articular and predominantly articular (Fig. 16.2) – based on plain AP and lateral radiographs. The classification system was found to be both substantially reliable (k, 0.664) and reproducible (k, 0.732). It achieved superior inter-observer and intra-observer agreement compared with the other three classification systems, with a low proportion of unclassifiable fractures. A management algorithm used with this classification aids the surgical decision-making process for these complex fractures (Fig. 16.3).
Presentation and investigations
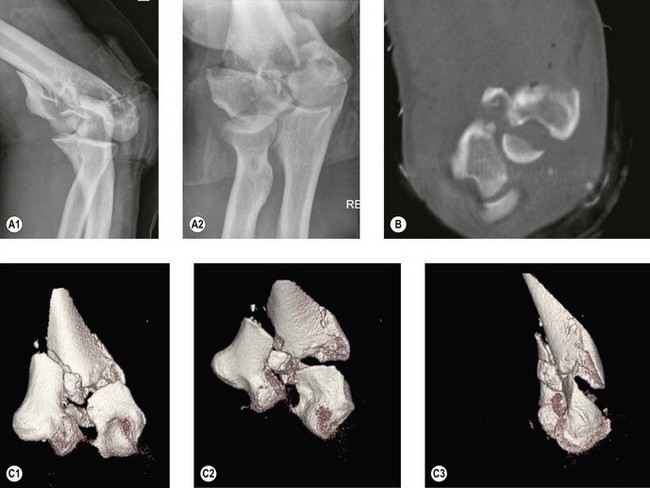
Once a clinical diagnosis has been established, plain anteroposterior and lateral radiographs should be performed to confirm the diagnosis (Fig. 16.4A). Further imaging with a CT scan may be helpful in assessing the type of fracture and the number and orientation of the fragments (Fig. 16.4B). More recently, three-dimensional reconstruction CT scanning has been used (Fig. 16.4C). Although these require more time and may increase the overall cost of imaging, they have been shown to be easier to interpret than two-dimensional scans and are helpful in identifying the components and special orientation of complex articular fragments. This can be particularly helpful for preoperative planning of complex fracture fixations.12
Surgical technique and rehabilitation
Clinical Pearl 16.2
With fractures extending proximally the radial nerve must also be found and protected.
If a preoperative decision is made that the fracture is not reconstructable, then either a hemiarthroplasty or total joint replacement should be considered. These options are described in Chapters 18 and 19.
Summary Box 16.1 Treatment options
| Elderly medically unfit patients | Conservative treatment |
|---|---|
| Young patients | Internal fixation – 90–90 plating or parallel plating |
| Elderly medically fit patients | Internal fixation, hemiarthroplasty or total elbow arthroplasty |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree