Mark W. Pagnano
The Aseptic, Failed Total Knee Arthroplasty: Indications for Revision
INTRODUCTION
Most patients achieve lasting improvements in their knee pain and function following primary total knee arthroplasty (TKA). In a series of more than 11,000 primary total knee arthroplasties of different designs,1 the survivorship was 91% at 10 years and 78% at 20 years. Over time, the orthopaedic community has attempted to improve upon these survivorship results by refining surgical indications, techniques, and implant design. Despite these efforts, a subset of knees will eventually require revision surgery due to septic or aseptic modes of failure. Moreover, due to the rapid increase in the number of primary TKA performed annually, this revision burden is expected to increase over time.2
Three recent studies have analyzed the modes of failure precipitating revision TKA. Fehring et al.3 reviewed the indications for early revision (within 5 years of the index arthroplasty) in 279 cases. Excluding the 105 infections, there were 174 patients who underwent revision for aseptic failure. The indications for aseptic revision surgery included instability (43%), failed ingrowth of uncemented components (21%), extensor mechanism complications (13%), polyethylene wear/osteolysis (12%), and aseptic loosening of cemented components (5%). Sharkey et al.4 reviewed 212 surgeries in 203 patients. The modes of failure seen in this study included polyethylene wear, aseptic loosening, instability, infection, arthrofibrosis, malalignment or malposition, deficient extensor mechanism, avascular necrosis in the patella, periprosthetic fracture, and isolated patellar resurfacing. More than half of all revisions in this series were performed within 2 years of the index operation, most of which were related to instability, malalignment or malposition, and failure of fixation. Finally, one recent study from the Mayo Clinic evaluated over 1,800 revision condylar total knee arthroplasties performed for aseptic reasons over a 30-year period.5 The indications for revision included loosening of components (36%), patellar or extensor mechanism problems (19%), instability (12%), failed unicondylar arthroplasty (11%), polyethylene wear (9%), malalignment (4%), stiffness (3%), periprosthetic fracture (2%), and other reasons in the remaining knees. The purpose of this chapter is to review the evaluation and treatment of these common modes of TKA failure.
EVALUATION OF THE FAILED TOTAL KNEE ARTHROPLASTY
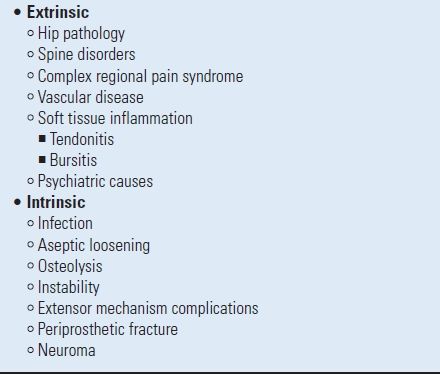
When evaluating the patient with a failed TKA, a systematic approach is required to differentiate the extrinsic and intrinsic causes of knee dysfunction (Table 39.1). This begins with obtaining a thorough history, performing a physical examination, and reviewing plain radiographs. The possibility of deep prosthetic infection should be further investigated with the use of arthrocentesis and screening laboratory tests. The occasional use of ancillary techniques, such as computed tomography or radionuclide scanning, may be deemed necessary to determine the etiology of enigmatic knee pain. Overall, each patient’s complaints with regard to pain, stability, and stiffness must be ascertained and prioritized. Establishing these specifics facilitates and clarifies the ensuing investigation. The importance of a clear diagnosis prior to proceeding with revision TKA cannot be overstated.6,7
TABLE 39.1 Intrinsic and Extrinsic Causes of Knee Dysfunction
History Historical information must be gathered from the preoperative, perioperative, and postoperative time periods. From the preoperative period, the surgeon should seek to understand the original etiology of the patient’s knee dysfunction, as well as any prior knee injuries or operations. Documentation of preoperative joint motion is critical when evaluating symptomatic postoperative stiffness. When possible, the patient’s prearthroplasty radiographs should also be reviewed.
Important perioperative data include the details of the surgical exposure, soft tissue releases, and complications. The patient should also be questioned about wound healing and antibiotic requirements associated with the original knee arthroplasty procedure. Finally, any issues related to physiotherapy should be discussed.
The postoperative history should elicit the location, character, severity, and timing of pain symptoms in relationship to the surgery. Factors that precipitate or alleviate pain symptoms should also be documented. Patients complaining of instability should be questioned regarding the perceived direction of instability, and any inciting events or joint positions. Joint function can be further assessed based on the patient’s requirement of knee braces or gait aids.
There are several specific examples of “classic” historical findings that strongly suggest specific diagnoses. For instance, the continuation or progression of preoperative pain combined with a stiff knee may herald an extrinsic etiology, such as ipsilateral hip pathology. The combination of pain since the time of surgery and pain at rest may suggest infection. Start-up or activity-related pain of recent onset after years of good function often implies aseptic loosening. Finally, difficulty arising from a chair or circumnavigating stairs in the presence of good knee motion is suggestive of tibiofemoral instability.
It is also necessary to search for factors that may complicate the current assessment of the results of TKA. The examiner should look for signs of unrealistic expectations, and/or underlying psychiatric diagnoses, such as depression. A recent study demonstrated that poor preoperative mental health, as measured by the SF-36 evaluation, is correlated with decreased function and increased pain following TKA.8 It is also useful to determine the patient’s initial basis for proceeding with the index surgery, as arthroplasty for reasons other than alleviation of pain makes it more difficult to determine the present basis of the patient’s pain. Finally, the surgeon must be cognizant of any family dynamics that may impact the perceived results of surgery. When such factors are identified, the appropriate intervention strategy must be created and a multidisciplinary care plan is often required.
Physical Examination A complete, multisystem physical examination is imperative in the evaluation of the painful TKA.9 The spine and hip should be examined to exclude these potential sources of referred pain. Suspected hip pathology should be confirmed with plain radiographs of the hip. Furthermore, when pain referred from the hip joint is a consideration, an intra-articular injection of local anesthetic into the hip joint is usually helpful to differentiate the pain source.
A thorough evaluation of the vascular and neurologic function of the limb should always be done. The skin about the knee should be inspected for any erythema or warmth suggestive of infection. Furthermore, skin lesions at sites distant from the knee should be sought after, as these may serve as a portal of entry for bacterial infections. The knee examination is based on the fundamentals of inspection, palpation, manipulation, and occasionally auscultation for entities such as failure of a metal-backed patellar component or pseudoaneurysm. The patient’s static knee alignment while standing, as well as the dynamic alignment during gait, should be studied. The surgeon must document joint range of motion and the presence or absence of a knee effusion, synovitis, or crepitus. The stability of the knee to varus-valgus and anterior-posterior stress should be tested in flexion and extension. Posterior cruciate ligament (PCL) dysfunction can be further assessed with a positive posterior sag sign or quadriceps active test. Areas of point tenderness should be evaluated, since bursitis, tendonitis, and neuromata can cause significant pain following TKA. Special attention must be given to the assessment of patellar tracking, as this can signal problems with component alignment and rotation.
Plain Radiographs Plain radiographs are essential in the evaluation of failed TKA. Most authors recommend a series of films to include a standing, full-length hip to ankle view in addition to anteroposterior (AP), lateral, and Merchant patellar views.9,10 The films should be assessed for the appropriate size and position of the implants and overall limb alignment. Component fixation is analyzed at the interfaces for the presence of radiolucent lines. Subtle radiolucent lines can be discovered more readily with the use of fluoroscopic evaluation11 (Fig. 39-1). The films should be compared to prior exams in order to assess component wear, progression of radiolucent lines, or osteolysis. The surgeon should seek out signs of catastrophic failure, such as implant fracture or metallosis. It is also prudent to evaluate the knee for patella baja, patella alta, or marked elevation of the joint line.

FIGURE 39-1. Fluoroscopically guided radiographs improve the detection of subtle radiolucent lines.
ASEPTIC LOOSENING
Aseptic loosening can complicate both cemented and uncemented TKA, and persists as one of the most common modes of TKA failure. Patients with loose implants often present with start-up pain and weight-bearing pain. Localized tenderness may be found adjacent to loose components.
The Knee Society published a radiographic scoring system in 198912 in an effort to standardize the reporting of results following TKA. Scores are assigned to the radiographs related to the width and extent of periprosthetic radiolucencies. While this system remains in wide use, many simplified adaptations can be found in the literature. Criteria for definite loosening often used include component subsidence ≥2 mm; a continuous periprosthetic radiolucency >1 mm in width; and progressive bead shedding from uncemented implants.
A number of risk factors for aseptic loosening following TKA have been reported.10 Varus malalignment can predispose the patient to tibial component loosening. Surface-only cement technique has also shown a detrimental effect in some designs.4 Failure of cemented femoral components has been ascribed to poor cement technique, inaccurate cuts, and deficient bone.13 On the patellar side, there are multiple risk factors that include asymmetric resection, patellar maltracking, patellar fracture, cementing into a sclerotic bed, and patellar osteonecrosis.10
Variable results have been reported regarding the rates of aseptic loosening of TKAs performed with or without cement. Uncemented implants were designed in an attempt to improve implant durability through biologic fixation; however, the use of uncemented implants resulted in some novel failure mechanisms. First, all uncemented implants are at risk of failed ingrowth and early loosening. Furthermore, incomplete osseointegration at the implant-bone interfaces of uncemented implants allows bony access of joint fluid laden with particulate wear debris, which can predispose to osteolysis and secondary aseptic loosening of uncemented implants. Many failures of uncemented designs are related to the failure of the metal-backed patella,14 as excellent results have been reported in some designs used without metal-backed patellae.15 However, in one study of cemented versus uncemented implants of a single design,16 the authors found a significantly higher rate of revision for aseptic loosening/osteolysis in the uncemented group, even when controlled for the use of a metal-backed patella. Moreover, in their retrospective review of over 11,000 primary total knees, Rand et al.1 found that the 10-year survivorship of cemented total knees was 92% compared to 61% for uncemented total knees. Surgeons choosing the method of initial implant fixation should evaluate both general and implant-specific survivorship data in order to maximize the benefits to the patient.
Symptomatic, loose TKA implants should be revised in medically fit patients. Radiographic loosening in the absence of symptoms or progressive bone loss could be closely monitored. Careful preoperative planning must be utilized to identify any underlying causes of prosthetic joint failure such as component malposition or malalignment, or any areas of bone loss which must be accounted for at the time of revision surgery. As mentioned previously, infection must be considered as an etiology of loosening and excluded prior to revision TKA.
OSTEOLYSIS
Wear particles generated by the prosthetic joint are thought to initiate a cascade of events mediated by proinflammatory cytokines and prostaglandins leading to the activation of osteoclasts and the inhibition of osteoblasts in the periprosthetic tissues.17 The net result is resorptive periprosthetic bone loss, or osteolysis, and has been recognized as an emerging cause of concern following TKA.18
There are a number of sources of wear debris around the prosthetic knee, including the articular and nonarticular surfaces of the polyethylene tibial component, the tibial post, the polyethylene patellar component, metal debris from failed implants, and cement debris from loosening of cemented implants19 (Fig. 39-2).

FIGURE 39-2. Backside wear in modular tibial components has been recognized as a major contributing factor to osteolysis following TKA.
The amount and type of wear debris generated depends on a variety of patient factors, surgical factors, and implant design issues. Patient factors of significance include age, size, and activity level, with activity level perhaps the most important variable.20 Surgical factors, such as failure to achieve a neutral mechanical axis, component malrotation, and poor ligament balance lead to a suboptimal mechanical environment and dramatically increased wear.18,20 Malalignment in the sagittal plane can lead to anterior postimpingement in some posterior stabilized (PS) knee designs and may also play a role in the development of osteolysis.21 Certain implant factors known to contribute to osteolysis20 include some flat-on-flat designs and thin tibial inserts, which can lead to higher contact stresses and rapid wear. Osteolysis has been seen more frequently following uncemented TKA compared to cemented TKA.22,23 Backside wear in modular TKA designs is another serious contributor to the generation of wear debris. Attempts to alter the wear characteristics of standard polyethylene, such as fabrication with carbon fibers and the use of Hylamer-M (DePuy;Warsaw, IN), have also had some deleterious effects.20,24 One of the most important advances in implant design has come with the recognition of the deleterious nature of gamma irradiation in air for polyethylene sterilization. In particular, if gamma-in-air-irradiated polyethylene is implanted after a long shelf life, high failure rates due to accelerated wear can be expected.25
Osteolysis around the knee is not always easy to recognize. It may present as a purely radiographic finding, or it may present with pain and an effusion. Care should be taken to evaluate the potential for infection, as not all periprosthetic bone loss is aseptic. Although CT scans and MRI with metal suppression techniques can be utilized to search out areas of osteolysis, plain radiographs remain the key means of investigation. Osteolysis tends to occur most frequently in certain anatomic areas around the knee19 (Fig. 39-3). In loose implants, areas of osteolysis typically expand the loose interfaces into the adjacent cancellous bone. Femoral osteolysis around well-fixed implants tends to occur in the posterior condyles and beneath the collateral ligament attachments, as best seen on the lateral and AP radiographs, respectively. In the tibia, these changes tend to occur at the periphery of the component or along access channels such as screws and stems. Patellar osteolysis tends to occur along the component margins and at the bone-implant/cement interfaces.

FIGURE 39-3. Massive femoral osteolysis noted on the lateral projection of the knee.
There are no absolute indications for revision TKA due to osteolysis; however, most would recommend revision surgery in medically fit patients in the presence of significant and/or progressive bone loss. Osteolysis that compromises implant fixation should also be addressed surgically. Mikulak et al.26 recently reported good results of revision TKA in patients with aseptic loosening and osteolysis. Surgeons caring for these patients must recognize that the level of bone loss encountered at the time of revision often greatly exceeds what is noted on the preoperative radiographs.
INSTABILITY
Instability is now one of the most common indications for revision TKA, especially in the first few years following index surgery.3,4 Classification of prosthetic tibiofemoral instability is based upon the direction of instability. The three basic types include coronal plane instability (collateral ligament instability, extension space instability), sagittal plane instability (AP instability, flexion space instability), and global instability.27 Patients with an unstable TKA can present with a variety of complaints. While some patients can present with frank giving-way episodes, many patients will present with a combination of subjective instability without giving-way, recurrent effusions, and pain.28,29
Instability following TKA can result from a number of causes,29,30 including gradual soft tissue stretching, failure to appropriately balance the soft tissues at the time of index surgery due to over- or underrelease, inaccurate bone resection leading to gap mismatch, acute trauma, and atraumatic acute rupture of a partially compromised ligament. Wear of the bearing surface and component subsidence can also lead to soft tissue laxity and ligamentous incompetence. Function of the extensor mechanism must be tested in all patients at the time of evaluation for instability, because extensor dysfunction can cause instability in the presence of intact ligamentous support.
The various prosthetic designs also impact TKA stability, such as cruciate-retaining, cruciate-substituting, constrained condylar, and hinged designs. In like manner, the overall size, alignment, and rotation of the prosthetic components will greatly impact ligamentous stability. The history, physical examination, and radiographs should be carefully scrutinized to evaluate the many possible etiologies of instability.
Collateral Ligament Instability Patients presenting with varus/valgus instability are often markedly disabled, often requiring external braces and gait aids. In most cases, the site of ligamentous insufficiency is easily determined based on the evaluation of gait, varus or valgus opening, and weight-bearing radiographs. Evaluation of coronal plane alignment is critical, as failure to correct pathologic varus or valgus alignment will continue to stress the convex side of the deformity.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








