The Ankle 
The ankle joint is constituted by multiple ligaments and supporting tendons, which are subject of various pathologies that can affect them in isolation or in combination with other structures. For systematic imaging analysis and structured reporting, the ankle can be divided into medial, lateral, anterior, and posterior compartmental structures. This chapter discusses the imaging evaluation approach and describes how to fill in the structured checklist in Box 1. Conceptual details of related MR physics and imaging protocol are discussed in the chapter on MR protocol optimization.
 IMAGE EVALUATION
IMAGE EVALUATION
The below-outlined stepwise interpretation approach is only a practical guide, and all ankle structures should be evaluated in multiple planes for their optimal assessment. The discussion below will help the reader perceive which structures are best depicted and evaluated in which particular plane.
1. Line up the similar-plane fat-saturated (fs) and non-fs images and synchronize them for tandem evaluation. From three-dimensional (3D) isotropic images, the technologist should create reconstructions in pre-specified planes to save the reading time.
2. Start with the sagittal images to look for possible tibiotalar, talonavicular, and subtalar joint effusions, integrity of the tibiotalar capsule and dorsal talonavicular ligament. Subsequently, evaluate for possible talar fault, pes planus/alta, Stieda process, os trigonum, Achilles tendon (AT) pathology, retrocalcaneal and/or retroachilles bursitis, as well as for Kager fat pad abnormalities. Then, evaluate sinus tarsi, Gissane angle, lateral process of talus, the anterior process of calcaneus, and bifurcate ligament moving from medial to lateral images. Look for plantar enthesophyte (spur), and for plantar fascia, and heel pad pathology. Finally, check for any obvious lesions, such as hindfoot or midfoot osteochondral lesion (OCL), osteoarthritis, mass lesion, or fracture. Although the sagittal plane is not ideal for ligament evaluation, the anterior and posterior talofibular ligaments can be seen on the far-lateral images as moustache-like structures extending from the fibula to the calcaneus (Fig. 1).
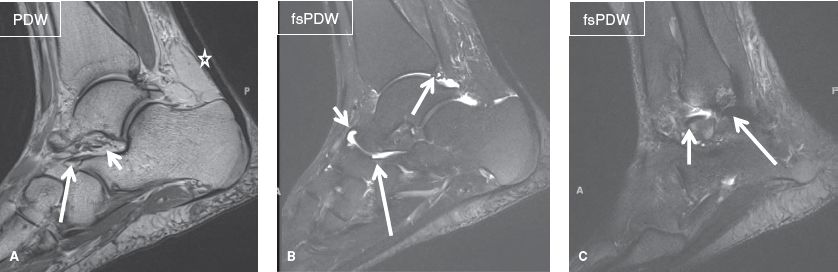
Fig. 1: Normal ankle anatomy on sagittal images. A: Long arrow, bifurcate ligament; short arrow, sinus tarsi; star, Achilles tendon. B: Long arrow, bifurcate ligament; medium arrow, posterior intermalleolar ligament; short arrow, dorsal talonavicular ligament. C: Long arrow, posterior talofibular ligament; short arrow, anterior talofibular ligament.
3. On the coronal plane, moving from anterior to posterior images, look for anteromedial talonavicular uncovering, ankle mortise asymmetry, talocalcaneal coalition, and hindfoot valgus. On the medial side, evaluate the medial malleolus, the three bands of the spring ligament (superomedial, medial plantar oblique, and inferoplantar), as well as the superficial and deep portions of the deltoid ligament. After reassessing the sinus tarsi, move to the lateral side, where the syndesmotic ligaments above the tibiotalar joint line (interosseous, anterior distal tibiofibular, and posterior distal tibiofibular), posterior intermalleolar (at the joint line), posterior talofibular (PFL), and calcaneofibular ligaments (CFL) (below the joint line) can be assessed from superior to inferior on a single image. Subsequently, evaluate the lateral malleolus, look for OCL in the talus or tibia, and check the three (medial, central, and lateral) cords of the plantar fascia bordering the plantar muscles. Finally, check the peroneus longus (PL) tendon insertion on the first metatarsal base, as it courses under the foot arch from lateral to medial (Figs. 2, 3).
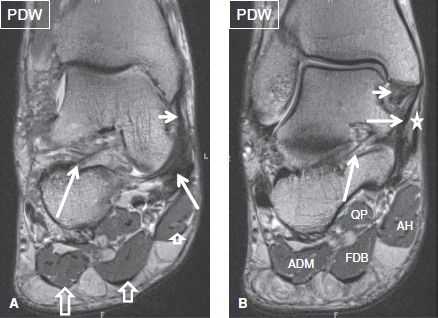
Fig. 2: Normal ankle anatomy on coronal images. A: Long arrow, cervical ligament; medium arrow, superomedial band of spring ligament; short arrow, tibiospring ligament; long open arrow, lateral cord of plantar fascia; medium open arrow, central cord of plantar fascia; short open arrow, medial cord of plantar fascia. B: Long arrow, interosseous talocalcaneal ligament; medium arrow, tibiocalcaneal ligament; short arrow, posterior deep tibiotalar ligament; star, flexor retinaculum; AH, abductor hallucis; FDB, flexor digitorum brevi; ADM, abductor digiti minimi; QP, quadratus plantae.
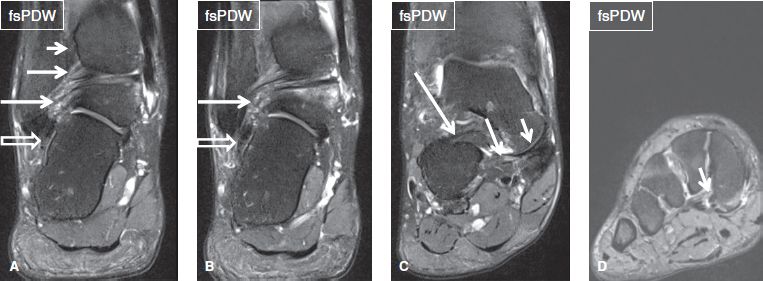
Fig. 3: Normal ankle anatomy on coronal images. A: Open arrow, calcaneofibular ligament; long arrow, posterior talofibular ligament; medium arrow, PIML; short arrow, posterior distal tibiofibular ligament. B: Open arrow, calcaneofibular ligament; long arrow, posterior talofibular ligament. C: Long arrow, inferoplantar band; medium arrow, medioplantar oblique band; short arrow, superomedial band of spring ligament. D: Arrow, normal striated insertion of the peroneus longus tendon.
4. The axial plane is best for ligament and tendon assessment. The interosseous, anterior distal tibiofibular, and posterior distal tibiofibular ligaments should be again evaluated above the joint line, the posterior intermalleolar ligament (PIML) at the joint line, and the deltoid, spring, anterior talofibular ligament (AFL), and PFLs below the joint line. All tendons should be traced from above the ankle to their insertions. Vessels, nerves, and tarsal tunnel are also best evaluated on the axial plane. Finally, axial plane is excellent for measuring the osteochondral lesions and mass lesions in the transverse axes (Fig. 4).
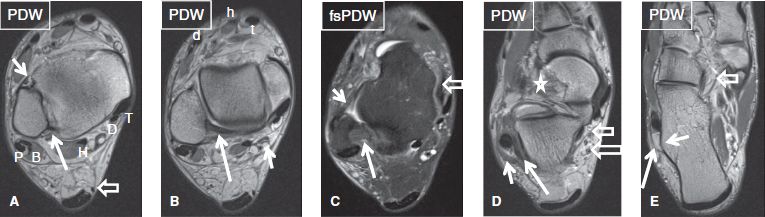
Fig. 4: Normal ankle anatomy on axial images. A: Long arrow, posterior distal tibiofibular ligament; short arrow, anterior distal tibiofibular ligament; open arrow, plantaris tendon; T, tibialis posterior; D, flexor digitorum longus; H, flexor hallucis longus; P, peroneus longus; B, peroneus brevis. B: Long arrow, posterior intermalleolar ligament; short arrow, tibial nerve; t, tibialis anterior; h, extensor hallucis; d, extensor digitorum. C: Long arrow, posterior talofibular ligament; short arrow, anterior talofibular ligament; open arrow, superomedial band of spring ligament. D: Long open arrow, lateral plantar nerve; short open arrow, medial plantar nerve; long arrow, calcaneofibular ligament; short arrow, superior peroneal retinaculum; star, sinus tarsi. E: Long arrow, inferior peroneal retinaculum; short arrow, peroneal tubercle; open arrow, recurrent slip of tibialis posterior.
 BOX 1: The Structured Report: Ankle
BOX 1: The Structured Report: Ankle
The checklist for structured reporting of MR imaging of the Ankle. For each field, Normal is considered default in the dictation whereas the rest of the elements describe various pathologies that could be encountered during imaging evaluation. See Appendix 1 and 2 at the end of the chapter for a sample completed reports of the normal and abnormal examination results.
Examination: MRI of Ankle [<With/Without>] Contrast
FINDINGS:
Alignment: [<Normal> <Talonavicular uncovering> <Talar fault> <Hindfoot valgus> <Pes planus> <Pes alta>]
Fluid:
Tibiotalar joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Posterior subtalar joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Talonavicular joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Calcaneonavicular joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Medial structures:
Medial malleolus: [<Normal> <Enthesopathy> <Contusion>]
Tendons:
Posterior tibial tendon: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Flexor digitorum longus: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Flexor hallucis longus: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Ligaments:
Deltoid ligament complex—superficial: [<Intact> <Thickened> <Acute sprain>]
Deltoid ligament complex–deep: [<Intact> <Thickened> <Acute sprain>]
Spring (plantar calcaneonavicular) ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Lateral structures:
Lateral malleolus: [<Normal> <Enthesopathy> <Contusion>]
Retromalleolar groove: [<Concave> <Flat> <Convex>]
Tendons:
Peroneus longus: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Peroneus brevis: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Superior peroneal retinaculum: [<Intact> <Thickened> <Deficient>]
Ligaments:
Interosseous (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
Anterior inferior tibiofibular (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
Posterior inferior tibiofibular (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
Anterior talofibular ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Calcaneofibular ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
Posterior talofibular ligament: [<Intact> <Thickened> <Mucoid degeneration> <Acute sprain>]
Bifurcate ligament: [<Intact> <Thickened> <Acute sprain>]
Posterior structures:
Posterior talus: [<Normal> <Os trigonum> <Stieda process>]
Posterior intermalleolar ligament: [<Intact> <Thickened>]
Achilles tendon: [<Normal> <Tendinosis> <Tear> <Kager fat pad edema> <Enthesophyte> <Retrocalcaneal bursitis> <Retroachilles bursitis>]
Plantar fascia: [<Normal> <Thickened> <Tear> <Perifascial edema> <Enthesophyte> <Heel pad edema>]
Anterior structures:
Tendons:
Anterior tibial tendon: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Extensor hallucis longus: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Extensor digitorum longus: [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Ligaments:
Dorsal talonavicular ligament: [<Intact> <Thickened> <Enthesopathy>]
Tibiotalar joint: [<Normal> <Osteochondral lesion> <Osteoarthritis>]
Subtalar joint: [<Normal> <Osteochondral lesion> <Osteoarthritis>]
Bones (other than subarticular marrow and malleoli): [<Normal> <Midfoot enthesopathy> <Midfoot osteoarthritis>]
Muscles: [<Normal>]
Nerves and tarsal tunnel: [<Normal> <Hyperintense medial plantar nerve>]
Sinus tarsi: [<Normal> <Edema> <Sinus tarsi syndrome>]
Vessels: [<Normal>]
Other: [<None>]
Impression:
[<In the order of importance with acute findings first>]
 HOW TO FILL THE STRUCTURED REPORT
HOW TO FILL THE STRUCTURED REPORT
Alignment: [<Normal> <Talonavicular uncovering> <Talar fault> <Hindfoot valgus> <Pes planus> <Pes alta>]
Evaluation of bony structures and bone alignment is best performed on non fs images, as one can clearly see the fatty marrow, bony cortices, and osteophytes. Normal alignment means bony articulation congruency at the tibiotalar, subtalar, and talonavicular joints. It is easy to remember the rule of 2–4–6: The medial and lateral mortise (tibiotalar articular) spaces are symmetrical with less than 2 mm side-to-side difference. The medial clear space (medial gutter) between the medial malleolus and the talus is less than 4 mm whereas the syndesmotic space (between the distal tibia and the fibula at 1 cm above the tibial plafond) is less than 6 mm. The central axis of the talus should correspond to the visualized base and shaft of the first metatarsal bone, and the central axis of the calcaneus should align with the base and shaft of the fourth metatarsal bone. The angle between these two lines is 20–40 degrees. Less than 20 degrees qualifies as hindfoot varus while more than 40 degrees as hindfoot valgus. Talar fault is best seen on sagittal images, where the talus inferiorly subluxes relative to the first metatarsal bone axis. Anteromedial uncovering, best seen on axial or coronal images, is established when there is loss of congruency at the talonavicular joint with anteromedial translation of talar head. Hindfoot valgus is best assessed on the posterior ankle images, where the angle between the lines drawn along the tibial and talar axes is greater than 6–8 degrees (Figs. 5, 6). Hindfoot varus and valgus can also be diagnosed on the axial image through the calcaneus, where the tibial axis should match up with the calcaneus axis, if no varus or valgus exists. Alternatively, it is assessed on the sagittal image by drawing lines along the talus and calcaneus axis (valgus: lateral talocalcaneal angle >50 degrees, varus: lateral talocalcaneal angle <35 degrees).
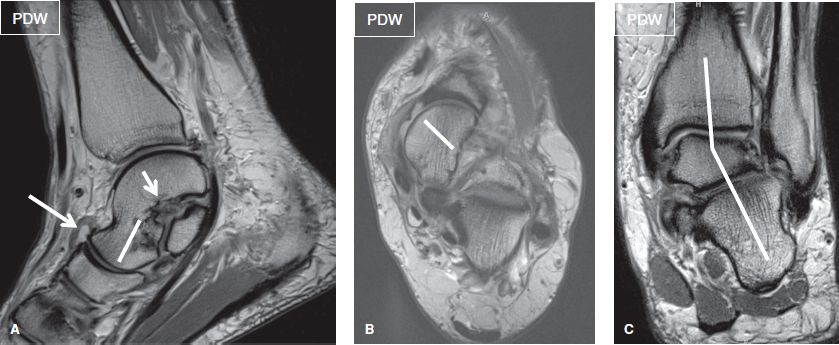
Fig. 5: Ankle malalignments. A: Line, mild talar fault; long arrow, thickened dorsal talonavicular ligament; short arrow, subcortical cysts at the sinus tarsi ligament attachment. B: Line, anteromedial uncovering of talus. C: Abnormally increased talocalcaneal angle indicates hindfoot valgus.
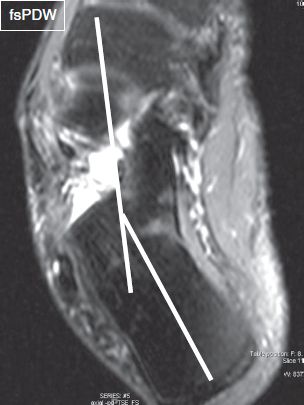
Fig. 6: Hindfoot varus on axial image. The angle between the central axis of the calcaneus and the shaft of the fourth metatarsal bone is less than 20 degrees.
Although weight-bearing imaging studies are the best for detecting malalignment, features suggesting various ankle instabilities (sensation of “giving way”) can also be seen on MR images. These instabilities can be lateral (typically inversion sprain), medial (typically eversion sprain), subtalar (related to pes planus), or rotational (with multidirectional malalignments). Lateral instability results from injury to two or more of lateral collateral ligaments, usually of the AFL and CFL, and leads to anterior translation and varus tilt to talus. Deltoid ligament injury is also common in these injuries, observed in 40% to 50% cases. Medial instability results from deltoid ligament injury and is seen as widening of medial gutter and valgus tilt of talus. Syndesmotic ligament injuries may also be associated due to similar mechanism leading to high ankle sprain. Subtalar instability results from CFL or sinus tarsi ligament tears and is associated with lateral translation of calcaneus with valgus positioning. Another important measurement is the calcaneal pitch (angle between horizontal along the heel and inferior calcaneus surface (normal angle = 20 to 25 degrees, pes alta >25 degrees, pes planus <20 degrees).
FLUID:
Tibiotalar joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Posterior subtalar joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Talonavicular joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
Calcaneonavicular joint: [<Normal> <Small effusion> <Moderate effusion> <Large effusion>]
The tibiotalar, posterior subtalar, talonavicular, and calcaneonavicular joints have thin synovial lining and small amount of fluid for nutrition and lubrication, which does not normally distend (convex margins) the capsule. Since the ankle is imaged in prone position, small amount of fluid in the posterior tibiotalar and subtalar recesses is normal. There is a normal communication between the tibiotalar and the posterior subtalar joints. To call the joint effusion, one should look for distention of the capsule (especially at the anterior, non-dependent portion of the capsule) and grade it as small (distension either anterior or posterior), moderate (distention both anterior and posterior), or large (distention anterior, posterior, and lateral) (Fig. 7). Associated synovial thickening, debris, intra-articular cartilaginous or osteochondral bodies, synovial diverticulae, and ganglion cysts should be reported, as they usually indicate underlying internal derangement. Capsular injuries may occur from recent or prior trauma, and manifest as irregularity, attenuation, and/or thickening of the capsules (Fig. 8). The articular cartilage normally appears as a 1–2 mm thick smooth continuous lining.
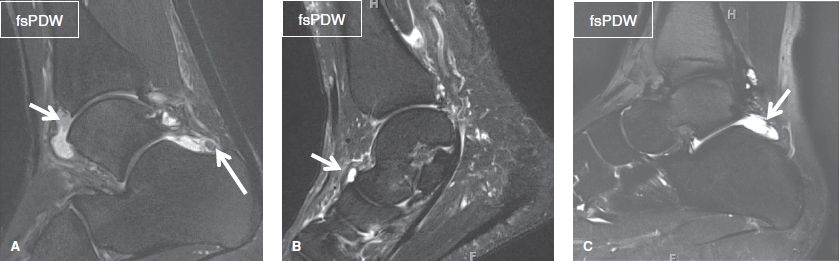
Fig. 7: Joint effusion on sagittal images. A: Moderate tibiotalar and small posterior subtalar effusion. Long arrow, loose body; short arrow, synovial thickening. B: Small talonavicular effusion (arrow). C: Small posterior subtalar effusion (arrow).
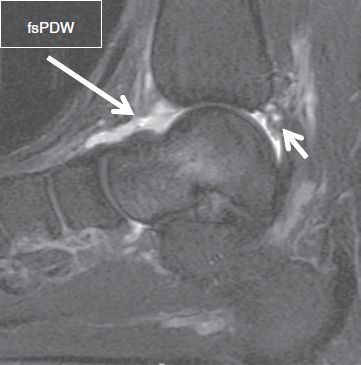
Fig. 8: Capsular rupture. Sagittal image demonstrates absent anterior joint capsule (long arrow) and irregular posterior joint capsule (short arrow) as well as an adjacent ill-defined fluid collections (short arrow).
MEDIAL STRUCTURES:
Medial malleolus: [<Normal> <Enthesopathy> <Contusion>]
TENDONS:
Posterior tibial tendon (PTT): [<Normal> < Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Flexor digitorum longus (FDL): [<Normal> < Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Flexor hallucis longus (FHL): [<Normal> < Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
LIGAMENTS:
Deltoid ligament complex—superficial: [<Intact> < Thickened> <Acute sprain>]
Deltoid ligament complex—deep: [<Intact> < Thickened> <Acute sprain>]
Spring (plantar calcaneonavicular) ligament: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
The bony contours are best assessed on coronal non–fs images for enthesopathy (Fig. 9), old or recent fractures (irregular edge/fragment fits the fracture site/bone marrow edema/acute angle with the fracture site) or accessory ossicles (round corticated unfused fragment with obtuse angle). The fat-suppressed images are useful for detecting subcortical avulsive cystic changes or bone marrow edema from flexor retinaculum or deltoid ligament avulsion, contusion or fracture. Beware of poor fat saturation images, especially on low-field scanners or frequency-selective fs images to avoid overcalling bone marrow edema (Fig. 10). Inversion recovery images perform better than frequency-selective fs images on low-field scanners for this purpose.
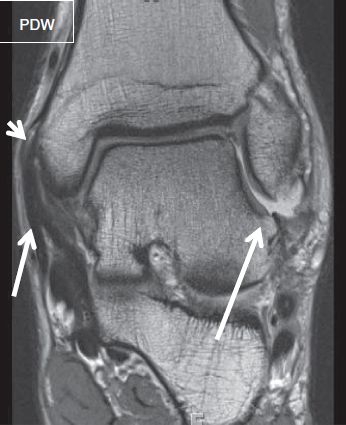
Fig. 9: Enthesophytes. Coronal image demonstrates an enthesophyte (short arrow) at the medial aspect of the medial malleolus with thickened flexor retinaculum (medium arrow) from prior injury. Also note enthesophyte at lateral process of talus from prior injury to calcaneofibular ligament (long arrow).
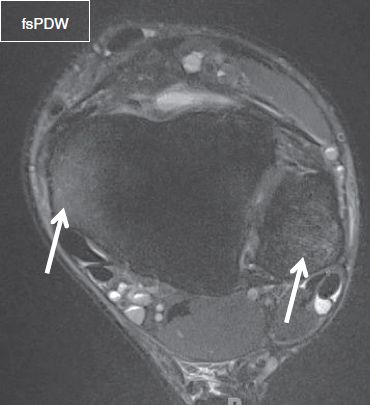
Fig. 10: Inadequate fat saturation on frequency-selective fat-suppressed axial image. High signal at the medial and lateral malleolus (arrows) is due to poor fat saturation, which should not be erroneously interpreted as marrow edema.
The medial tendons are best evaluated on the axial images. Liniing up, from anterior to posterior, are the PTT, FDL tendon, and FHL tendon, which are all bounded by the flexor retinaculum. Accessory muscles, such as accessory FHL or accessory FDL may be incidentally present and these follow the respective tendons. The flexor retinaculum attaches to medial malleolus and is proximally continuous with deep fascia of leg and distally with plantar aponeurosis and abductor hallucis (AH) fascia. If flexor tendons are torn, the retraction is best measured on the sagittal images. Trace fluid is normal along the dependent portions of the tendons. Tendons also have 1–2 remnant linear bands of synovial layers within their sheath, called mesotenon(s). The findings indicative of tenosynovitis include, any fluid that is circumferential around the tendon, or more than 2 mm thickness in the nondependent portion, or if it is associated with synovial thickening/debris (Fig. 11). Although infection leads to abnormal synovial thickening, fascial edema, and/or surrounding tissue reaction, it is often difficult to define the cause of tenosynovitis (mechanical, infection, inflammatory, or post-traumatic). If there is clinical suspicion for infection, synovial fluid should be aspirated. Stenosing tenosynovitis is diagnosed when multiple septations, asymmetric pooling of fluid and/or fluid loculations exist within and along the tendon sheath. FHL stenosing tenosynovitis has been associated with os trigonum syndrome. As elsewhere in the body, tendinosis reflects incompletely healed microtears. Mild tendinosis is seen as increased signal in the tendon on the proton density-weighted (PDW) images without fluid-like bright signal. Moderate tendinosis is seen as increased signal and tendon thickening. Severe tendinosis is seen as near fluid-bright signal, marked tendon thickening, and edge irregularities, often difficult to differentiate from tendon tears. Tendon tear shows up as fluid-bright signal (partial or complete tear) or as longitudinal split with or without distal reconstitution, or as complete tear with retracted edges. Tendinosis predisposes to tears, as normal tendons do not tear spontaneously, unless transected by a penetrating injury. Therefore, it is important to describe both quality of the tendon and tear, as mild/moderate/severe tendinosis with superimposed partial/complete tear. FHL tenosynovitis is common at the sites of anatomic constrictions, at os trigonum/Stieda process, at the Henry knot (crossing of FHL and FDL), and at level of the hallux sesamoid bones (Fig. 12). It should be noted that the submalleolar portions of the medial flexor tendons are prone to magic angle artifacts, and minimal increased signal may be normally seen on low echo time images.
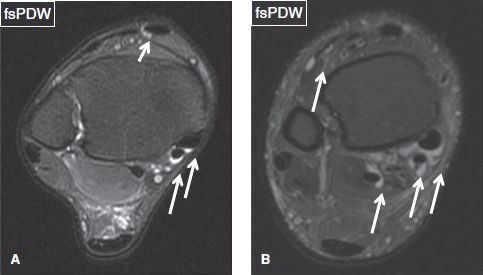
Fig. 11: Physiologic versus pathologic tendon sheath fluid on axial images. A: Normal trace fluid along the dependent portions of the posterior tibial and flexor digitorum longus tendons (long arrows). Normal vessels mimicking fluid adjacent to tibialis anterior tendon (short arrow). B: Circumferential and greater than 2 mm in thickness fluid around the posterior tibial, flexor digitorum longus, flexor hallucis longus, and extensor digitorum tendons (arrows) indicating tenosynovitis.
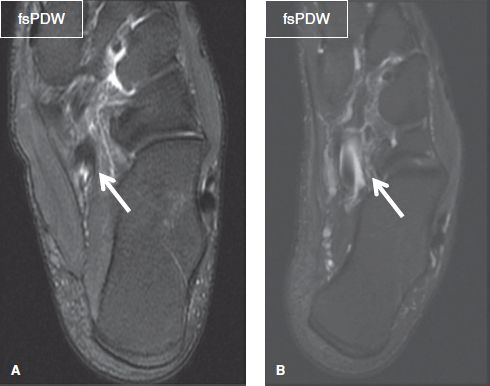
Fig. 12: Henry knot on axial images. A: Trace fluid is a common finding at Henry knot (arrow), where the flexor digitorum longus and flexor hallucis longus tendons cross each other. B: Circumferential fluid (arrow) around the flexor hallucis longus tendon at the level of Henry knot, without ankle effusion, corresponds to tenosynovitis.
The PTT is the most commonly injured and biomechanically important medial tendon. It is the anterior most medial tendon in the retromalleolar grove, coursing beneath the flexor retinaculum along with two other medial tendons, to terminate as multiple layers that insert on the navicular tuberosity, cuneiforms, metatarsals, and sustentaculum talus. It is the primary invertor of the foot, aids in plantar flexion, and supports the medial longitudinal arch with assistance from FHL and FDL. On axial images, normal PTT is about 1.5 to 2 times the size of the FDL tendon. The PTT overlies the superomedial band of the spring ligament and is separated from the latter by a connective tissue layer (gliding zone). At its insertion, the PTT fans out to insert on navicular tuberosity, cuneiforms, sustentaculum talus, and bases of second to fourth metatarsals. At the insertion, it commonly shows minimal thickening and/or increased signal, which are normal findings. However, fluid and edema surrounding this distal 1–2 cm segment (paratenonitis) is abnormal, since there is no normal synovial sheath around this distal part of the tendon.
An accessory ossification center for the navicular, known as os naviculare, may be identified along the insertional fibers of the PTT. Type I os naviculare (os tibiale externum) is a small (few mm) sesamoid bone within the distal PTT. Type II (prehallux) is a triangular or heart-shaped ossicle which measures up to 12 mm and is connected to the navicular tuberosity by fibrocartilage or hyaline cartilage (synchondrosis). Type III (cornuate naviculum) is a partially (medially) fused ossicle that is connected to the navicular by a medial bony ridge (Fig. 13). Type II os naviculare is most commonly implicated in pathology. Painful os naviculare syndrome involves one or a more of the following findings: presence of os naviculare (commonly type II); bony hypertrophy of the accessory ossicle and navicular tuberosity; bone marrow edema; soft tissue edema; formation of adventitial bursa over the bony prominence; frank disruption and widening of the synchondrosis with fluid-like cleft; PTT tendinosis and/or tear (Fig. 14).
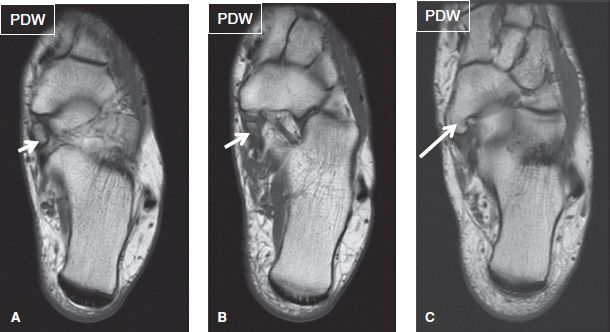
Fig. 13: Os naviculare types on axial images. A: Type I os naviculare (os tibiale externum): 6 mm sesamoid bone (arrow) within the distal posterior tibial tendon. B: Type II os naviculare (prehallux): a triangular or heart-shaped ossicle (arrow) which is connected to the navicular tuberosity by fibrocartilage (synchondrosis). C: Type III os naviculare (cornuate naviculum): a partially fused ossicle (arrow), which is connected to the navicular by a medial bony ridge.

Fig. 14: Painful os naviculare. Axial images (A, B) demonstrate a type II os naviculare (arrows), associated with bone marrow edema on both sides of the synchondrosis.
Insertional PTT tendinosis is best seen on axial and coronal images. It presents with moderate thickening and/or signal alteration of the tendon (Fig. 15). PTT tears most commonly occur at or just distal to the level of the medial malleolus, rather than more distally, and have been classified into three types, based on severity:
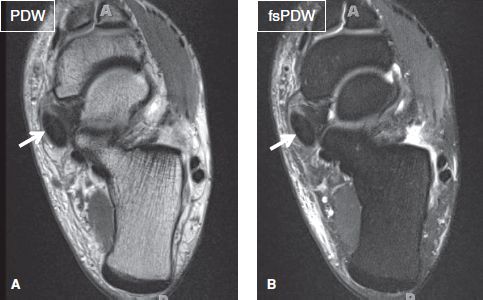
Fig. 15: Posterior tibial tendinosis. Axial images (A, B) exhibit moderate thickening and intermediate signal in the distal posterior tibial tendon (arrows).
 In type I tears, there is fusiform tendon enlargement (>2× the size of FDL tendon) with varying degrees of increased intrasubstance tendon signal that histologically represent chronic tendinopathy with superimposed areas of longitudinal split tears. With current imaging techniques, the splits can be easily identified in most cases.
In type I tears, there is fusiform tendon enlargement (>2× the size of FDL tendon) with varying degrees of increased intrasubstance tendon signal that histologically represent chronic tendinopathy with superimposed areas of longitudinal split tears. With current imaging techniques, the splits can be easily identified in most cases.
 In type II tear, there is thinning (<1.5× the size of the FDL tendon) and elongation of the affected tendon segment with variable amounts of increased intrasubstance signal intensity. In some cases, the tendon splits completely into two subtendons (Figs. 16–18).
In type II tear, there is thinning (<1.5× the size of the FDL tendon) and elongation of the affected tendon segment with variable amounts of increased intrasubstance signal intensity. In some cases, the tendon splits completely into two subtendons (Figs. 16–18).
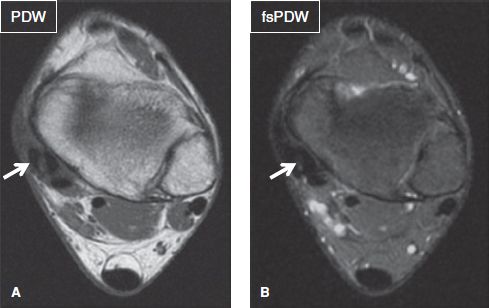
Fig. 16: Longitudinal split tear of the posterior tibial tendon, creating the “four-tendon sign.” Axial images (A, B) demonstrate four (instead of three) distinct tendons at the medial side of the ankle joint. The two most anteromedial tendinous structures (arrows) represent longitudinal splitting and separation of the original posterior tibial tendon.
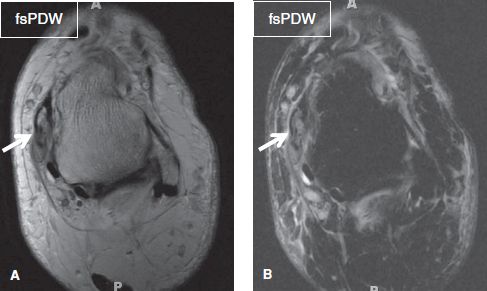
Fig. 17: Multifocal split tears of the posterior tibial tendon. Axial images (A, B) demonstrate multiple linear fluid-like signals within the distal posterior tibial tendon fragments (arrows).
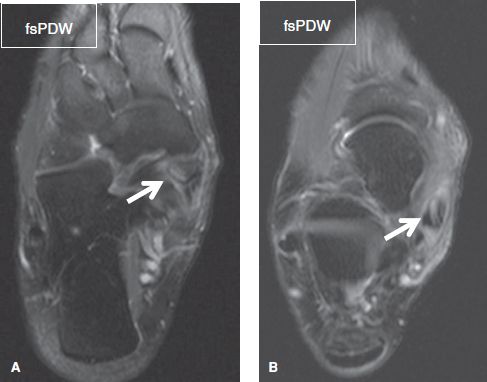
Fig. 18: Posterior tibial tendon tear in the presence of os naviculare. A: Axial image demonstrates an os naviculare type II (arrow) with mild bone marrow edema at the posterior tibial tendon insertion. B: More proximally, the posterior tibial tendon exhibits a longitudinal split tear (arrow).
 In type III tears, there is complete tendon disruption with fluid signal intensity within the tendon gap (Fig. 19).
In type III tears, there is complete tendon disruption with fluid signal intensity within the tendon gap (Fig. 19).
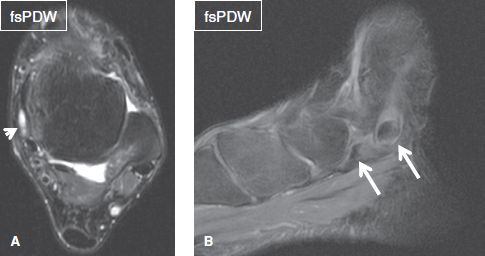
Fig. 19: Complete posterior tibial tendon disruption. A: In the axial plane, only fluid is identified at the expected position of the posterior tibial tendon (arrow). B: Sagittal image shows complete disruption of the posterior tibial tendon, with associated retraction of the torn fragments (arrows).
In all three types, additional findings may include tenosynovitis, flexor retinaculum thickening or attenuation, partial tear of the superomedial portion of the spring ligament, marginal osteophytes of the medial malleolus (retromalleolar groove), and/or marrow edema of the medial talus (Fig. 20). Thickened tenosynovium, focal fluid distensions of the tendon sheath and complex septations within the fluid are indicative of stenosing tenosynovitis (Fig. 21).
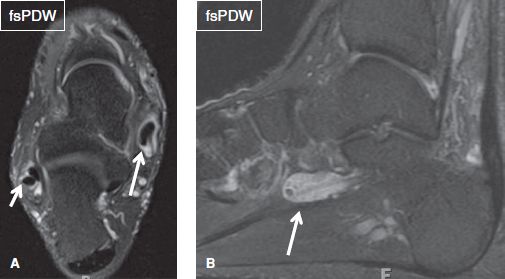
Fig. 20: Posterior tibial tenosynovitis. A: Circumferential fluid along the posterior tibial tendon (long arrow) is indicative of tenosynovitis, in this case of rheumatoid arthritis. Note concurrent peroneus longus tenosynovitis (short arrow). B: A large fluid collection along with multiple tiny hypointense foci within the flexor hallucis tendon sheath (arrow) is due to synovial chondromatosis and stenosing tenosynovitis.
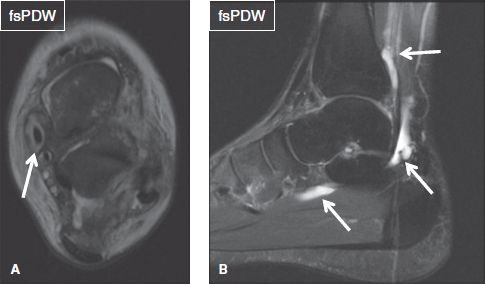
Fig. 21: Post-traumatic synovitis and stenosing tenosynovitis. A: Axial image acquired after recent ankle injury demonstrates circumferential fluid (arrow) around the posterior tibial tendon and diffuse soft tissue edema, corresponding to post-traumatic tenosynovitis. B: Sagittal image exhibits focal fluid distensions and septations within the flexor hallucis longus tendon sheath, which are indicative of stenosing tenosynovitis.
The PTT may rarely undergo subluxation or dislocation in an anteromedial direction relative to the medial malleolus. PTT dislocation may be associated with stripping or avulsion of the overlying flexor retinaculum, seen as a fleck of bone near the medial malleolus or enthesopathy at its expected attachment. Isolated spring ligament tears and flexor retinaculum injuries may clinically mimic PTT abnormality. Degeneration of the PTT may be associated with secondary abnormalities of multiple ligaments, joint capsule, fascia, articulations, and bony structures of the ankle, hindfoot, midfoot, and forefoot, in a syndrome known as PTT dysfunction (described below, in a separate paragraph).
The FHL tendon is the posterior-most tendon of the ankle. It is located between the medial and the lateral tubercles of the ankle, and features a long muscle belly, which is commonly visible at the tibiotalar joint level. The tendon courses along the undersurface of the sustentaculum talus (typical location for tendon identification on the sagittal view) and between the sesamoid bones of the first toe to insert at the base of the great toe distal phalanx. It is a weak plantar flexor of the ankle, maintains the first toe pad on ground when the foot is on ground, and plantar flexes the phalanges of the great toe when the foot is off ground. In 20–40% of individuals, the FHL tendon sheath communicates with the tibiotalar joint, and therefore, the reader should not overcall FHL tenosynovitis unless the tendon sheath fluid is disproportionate to the ankle joint effusion and/or more complex. In most situations, the FHL tendon shows more fluid than the PTT and the FDL tendon. The FDL and FHL tendons cross each other at the hindfoot–midfoot junction (Henry’s knot), where their tenosynovial sheaths communicate, and it is common to see fluid loculation or ganglion cyst formation at that site. FHL tenosynovitis/tears are most commonly seen in ballet dancers. Other settings include os trigonum syndrome, fracture of posterior process of talus (medial tubercle, Cedell fracture; lateral tubercle, Shepherd fracture) and accessory FHL muscle. The typical locations of pathology include, behind the ankle, at Henry’s knot, and in the inter-sesamoid space. The latter is commonly associated with first metatarsophalangeal degenerative changes and/or hallux valgus deformity.
The FDL tendon is located posterior to the PTT under the flexor retinaculum. The tendon then runs laterally, across the plantar arch, crosses superficial to the FHL tendon, and inserts on the plantar base of all lesser toe distal phalanges. It divides into four slips, which give origin to lumbricals that assist in plantar flexion of foot. When the foot is on ground, it maintains pads of lesser toes whereas when the foot is off ground, it flexes second to fifth phalanges. It is relatively well protected and is rarely involved in pathologies. Its most common pathology is tenosynovitis whereas tears are uncommon. Small amount of tenosynovial fluid at the level of the ankle joint is a normal finding, as is at the Henry’s knot, particularly if there is FHL tenosynovial fluid more proximally.
The deltoid ligament is a very strong ligament, composed of superficial and deep components. The superficial components are best depicted on the axial and coronal images and include the following, from anterior to posterior:
 The tibionavicular ligament is a thin, homogenous hypointense band, which is 0.5 to 1 cm wide, and extends from the medial malleolus to the navicular tuberosity
The tibionavicular ligament is a thin, homogenous hypointense band, which is 0.5 to 1 cm wide, and extends from the medial malleolus to the navicular tuberosity
 The tibiospring ligament is the most superficial component, which extends from the medial malleolus to the superior border of the spring ligament (Fig. 22)
The tibiospring ligament is the most superficial component, which extends from the medial malleolus to the superior border of the spring ligament (Fig. 22)
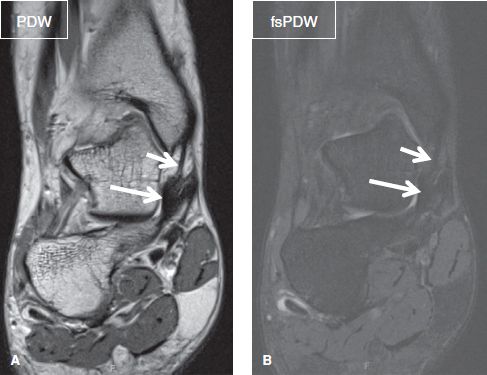
Fig. 22: Normal spring and tibiospring ligaments. Coronal images (A, B) demonstrate the superomedial band of the spring ligament (long arrows), which connects the medial surface of sustentaculum talus to naviculum and merges superiorly with tibiospring ligament (short arrows), which extends superiorly to the medial malleolus.
 The tibiocalcaneal ligament is 2 to 3 mm thick and represents the strongest superficial component. It originates from the medial aspect of the anterior colliculus, descends vertically, and inserts on the medial border of the sustentaculum tali. It interlaces with those of the superomedial band of the spring ligament (Fig. 23)
The tibiocalcaneal ligament is 2 to 3 mm thick and represents the strongest superficial component. It originates from the medial aspect of the anterior colliculus, descends vertically, and inserts on the medial border of the sustentaculum tali. It interlaces with those of the superomedial band of the spring ligament (Fig. 23)
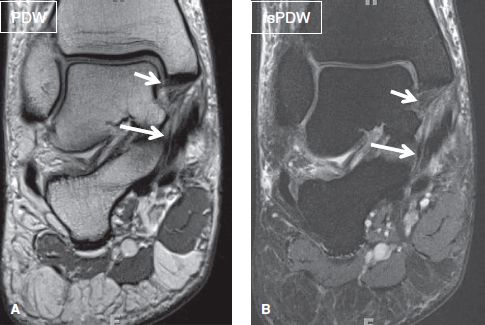
Fig. 23: Normal tibiocalcaneal and posterior deep tibiotalar ligaments. Coronal images (A, B) demonstrate the tibiocalcaneal ligament (long arrows), which extends from the medial malleolus to the sustentaculum tali, as well as the thick and normally striated posterior deep tibiotalar ligament (short arrows), which extends from the medial surface of the talus to the posteromedial talar tubercle.
 The superficial posterior tibiotalar ligament is a thin hypointense band, which originates from the posterior part of the medial surface of the anterior colliculus. It courses posteriorly, inferiorly, and laterally, and inserts on the posteromedial talar tubercle.
The superficial posterior tibiotalar ligament is a thin hypointense band, which originates from the posterior part of the medial surface of the anterior colliculus. It courses posteriorly, inferiorly, and laterally, and inserts on the posteromedial talar tubercle.
Of these components, the tibiocalcaneal ligament is the thickest, and the tibiospring is the only one that attaches to the spring ligament; the other bundles connect adjacent bones. The deep components of the deltoid ligament include a) the anterior deep tibiotalar ligament, which appears as a 2–3 mm thick striated band that extends from the anteromedial portion of the medial malleolus and inserts onto the talar neck (Fig. 24) b) the deep posterior tibiotalar ligament, which appears as a 5–15 mm thick striated band with broad attachment to the medial surface of the talus, as far posteriorly as the posteromedial talar tubercle (Fig. 23).
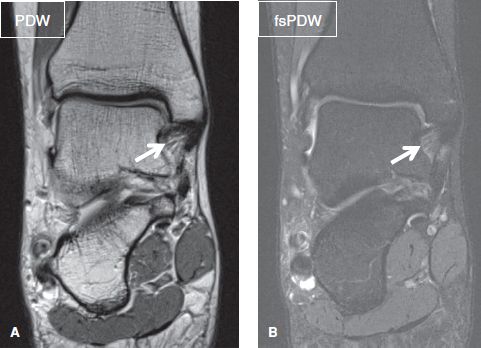
Fig. 24: Normal anterior deep tibiotalar ligament. Coronal images (A, B) demonstrate the anterior deep tibiotalar ligament as a striated band (arrows), extending from the anteromedial portion of the medial malleolus to the talar neck.
Rotational and translation injuries are the most frequent mechanisms for deltoid ligament injury. Acute tears of the deltoid ligament usually result from significant pronation/eversion injuries, involve both the superficial and the deep portions, and are commonly associated with lateral ligament injuries. Clinically, patients present with medial ankle pain, tenderness, and instability. Tears of the deep posterior tibiotalar component often occur with medial malleolus fractures, and are associated with local hemorrhage. Acute ligament sprains are classified as follows.
 Grade I (ligament stretch): Appears as thickening and/or loss of the fatty striations of the ligament on PDW or T1-weighted (T1W) images, along with periligamentous edema. With chronic injury or repeated sprains, it may lead to diffuse thickening of the ligament from remodeling (Figs. 25, 26)
Grade I (ligament stretch): Appears as thickening and/or loss of the fatty striations of the ligament on PDW or T1-weighted (T1W) images, along with periligamentous edema. With chronic injury or repeated sprains, it may lead to diffuse thickening of the ligament from remodeling (Figs. 25, 26)
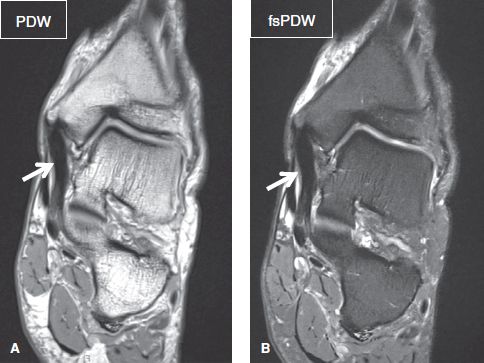
Fig. 25: Chronic sprain of the tibiospring ligament. Coronal images (A, B) show homogeneous thickening and remodeling of the tibiospring ligament with proximal enthesopathy (arrows).
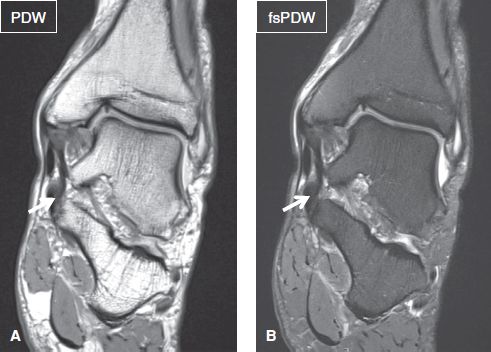
Fig. 26: Chronic sprain of tibiocalcaneal ligament. Coronal images show mild diffuse thickening of the tibiocalcaneal ligament with distal enthesopathy (arrows).
 Grade II (partial tear): Appears as intraligamentous increased signal on fat-suppressed PDW or T2-weighted (T2W) images (Figs. 27–29)
Grade II (partial tear): Appears as intraligamentous increased signal on fat-suppressed PDW or T2-weighted (T2W) images (Figs. 27–29)

Fig. 27: Grade II sprain of the tibiospring ligament. Coronal image exhibits thickening and ill definition of the tibiospring ligament, which maintains partial continuity (arrow). Findings correspond to a partial tear.

Fig. 28: Grade II sprain of the tibiocalcaneal ligament. Coronal image demonstrates a near full-thickness tear of the tibiocalcaneal ligament (arrow).
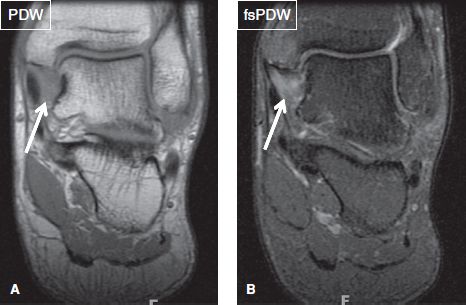
Fig. 29: Grade II sprain of the deep deltoid ligament. Coronal images (A, B) exhibit an ill-defined deep deltoid ligament, which lacks its normal striated configuration (arrows). Notice medial malleolar avulsive edema.
 Grade III (complete tear): Characterized by discontinuity and wavy contours of the torn ligament (Figs. 30, 31)
Grade III (complete tear): Characterized by discontinuity and wavy contours of the torn ligament (Figs. 30, 31)
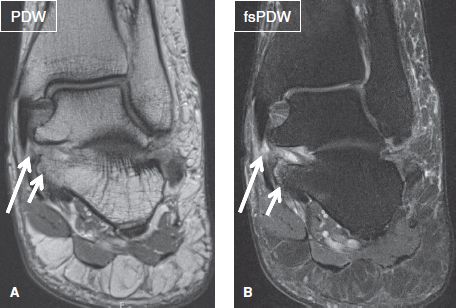
Fig. 30: Grade III sprain of the tibiocalcaneal (superficial) deltoid ligament. Coronal images (A, B) demonstrate discontinuity of the tibiocalcaneal (long arrows) ligament. Notice chronic enthesopathy and cystic changes of the calcaneal attachment site (short arrows).
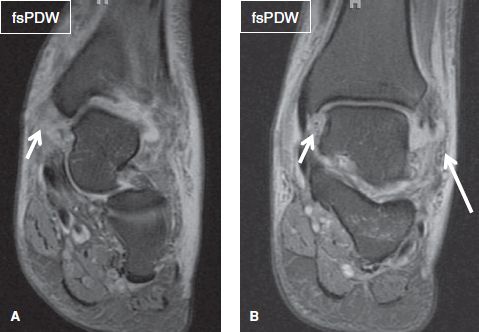
Fig. 31: Grade III sprain of the deltoid ligament. On coronal images (A, B), there is extensive soft-tissue edema around the ankle, and particularly at the medial aspect of the joint, where the tibiospring and deep posterior tibiotalar ligaments are not visualized at their expected location (short arrows). Also note complete lateral collateral ligament disruption (long arrow).
Acute ligament sprains may also be associated with syndesmotic ligament injuries (occasionally with posterior malleolar fracture), flexor retinaculum tears (occasionally with bony avulsion), enthesopathic changes of the medial clear space (i.e., of the medial malleolus and medial process of talus or calcaneus), PTT and/or spring ligament injuries, lateral collateral ligament injuries and Weber type A, B, or C (Maisonneuve) fibular fractures, and ganglion cyst formation (Fig. 32). If there is ankle dislocation with medial sided injury, such as malleolus fracture, deltoid ligament would be definitely torn. Treatment wise, superficial deltoid or associated spring ligament injuries can be repaired; deep deltoid injury is managed conservatively with immobilization; and syndesmotic ligament injury is fixed with syndesmotic screws.
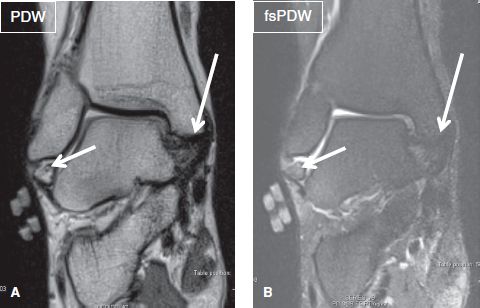
Fig. 32: Chronic Weber type A fracture. Coronal images (A, B) show a bone fragment inferior to the lateral malleolus, corresponding to a chronic Weber type A fracture (short arrows). Notice mild thickening of superior portion of the deep posterior tibiotalar ligament (long arrows).
The spring (or plantar calcaneonavicular) ligament extends from the calcaneus to the navicular bone and is composed of the superomedial, medioplantar oblique, and inferoplantar bands. It is normally 2–5 mm thick, features a small synovial recess between the superomedial and medioplantar oblique band. The superomedial band connects to the tibiospring ligament superiorly (Fig. 22). A fibrocartilaginous portion of the ligament lies superficial to the talar head. The superomedial band connects the medial surface of sustentaculum talus to the naviculum and merges superiorly with tibiospring ligament. Inferoplantar band connects the body of calcaneus to the naviculum, and medioplantar oblique connects the anterior margin of sustentaculum talus to the naviculum. The three bands are best assessed on axial and coronal images, though the medioplantar oblique and inferoplantar bands can also be evaluated on sagittal images. Acute injuries of the spring ligament most often involve the superomedial band, and these are commonly associated with deltoid ligament sprains. Because of the proximity of the spring ligament to the PTT and its integral function in stabilizing the plantar arch, spring ligament injuries are almost always associated with PTT dysfunction. Spring ligament injuries are classified similarly to deltoid ligament sprains (Figs. 33–35). Degeneration of the spring ligament is more common than acute sprains. Ganglions in relation to the spring ligament are usually encountered between the superomedial and the medial plantar oblique bands at the site of the plantar recess site, and in deltoid ligament among its deep fibers (Figs. 36, 37).
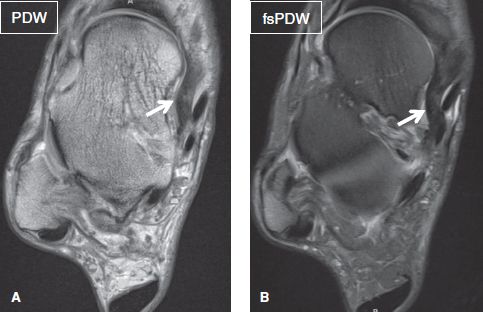
Fig. 33: Chronic sprain of the spring ligament. Axial images (A, B) show homogeneous thickening of the superomedial band of the spring ligament (arrows).
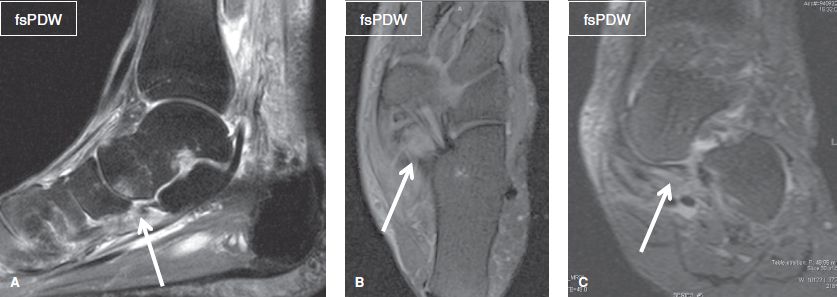
Fig. 34: Grade II sprain of the spring ligament. Sagittal (A), axial (B), and coronal (C) images demonstrate a partial thickness tear of the medioplantar oblique band of the spring ligament (arrows) with adjacent fascial edema.
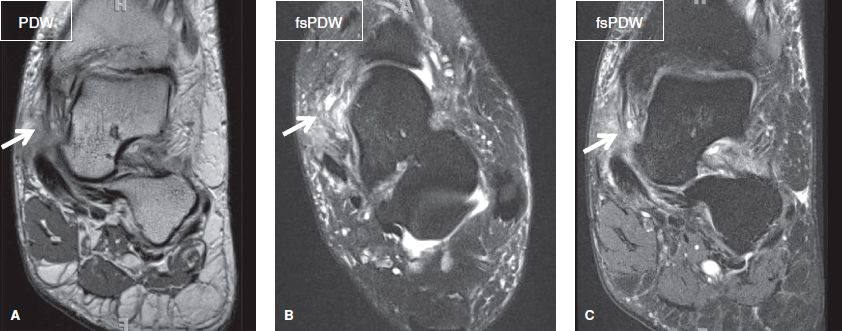
Fig. 35: Grade III sprain of the tibiospring ligament and superomedial band of the spring ligament. Coronal (A, C) and axial (B) images exhibit discontinuity of the tibiospring ligament and superomedial band of the spring ligament (arrows), as well as edema of the surrounding soft tissues. Notice edema and scarring suggesting sinus tarsi syndrome.
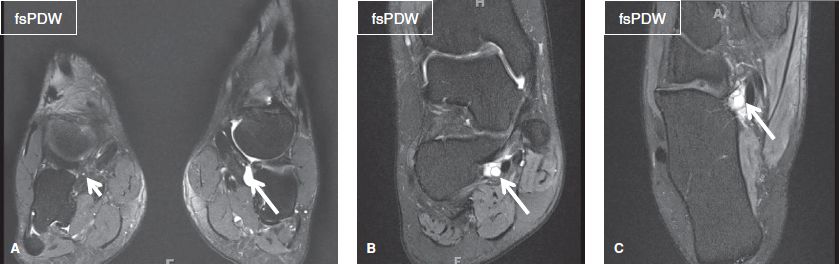
Fig. 36: The plantar recess of the spring ligament. Coronal image (A) of both ankles demonstrates the normal recess of the spring ligament (short arrow), located between its superomedial and medial plantar oblique bands in the right ankle and small synovial diverticulum (long arrow) in the left ankle. Coronal (B) and axial images (C) in another individual show a multiloculated ganglion (arrows) at the expected recess.

Fig. 37: Ganglion of the deltoid ligament. Coronal image exhibits a ganglion (arrow) within the substance of the deltoid ligament, related to chronic ligamentous and adjacent synovial injury.
LATERAL STRUCTURES:
Lateral malleolus: [<Normal> <Enthesopathy> <Contusion>]
Retromalleolar groove: [<Concave> <Flat> <Convex>]
TENDONS:
PL: [<Normal> < Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Peroneus brevis (PB): [<Normal> <Tendinosis> <Tenosynovitis> <Split tear> <Complete tear>]
Superior peroneal retinaculum (SPR): [<Intact> < Thickened> <Deficient>]
LIGAMENTS:
Interosseous (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
Anterior inferior tibiofibular (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
Posterior inferior tibiofibular (syndesmosis): [<Intact> <Thickened> <Acute sprain>]
AFL: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
CFL: [<Intact> <Thickened> <Attenuated> <Acute sprain>]
PFL: [<Intact> <Thickened> <Mucoid degeneration> <Acute sprain>]
Bifurcate ligament: [<Intact> <Thickened> <Acute sprain>]
The lateral malleolus is also best assessed on coronal non–fs images for enthesopathy, old/recent fractures, or accessory ossicles. Fat-suppressed images are useful for detection of subcortical avulsive cystic changes or bone marrow edema from extensor/peroneal retinaculum or ligament avulsion, contusion, and fracture. Beware of poor fat saturation images, especially on low-field scanners to avoid overcalling bone marrow edema. Inversion recovery images perform better than frequency-selective fat saturation images on low field scanners. The retromalleolar groove is best assessed on the axial images, about 1 cm proximal to the tip of the fibula. In 82% of individuals it is smooth and concave, though less commonly it assumes a flat or convex configuration with or without irregular contour. The latter predisposes to peroneal tendon subluxation or dislocation and mechanical attrition (Fig. 38). The SPR, a thickening of the deep fascia, extends from the lateral malleolus to the deep fascia of foot or the calcaneus. The inferior peroneal retinaculum (IPR) extends from the posterior surface of the lateral malleolus to the peroneal tubercle (trochlea) of the lateral calcaneus, distal to the retrotrochlear eminence, where the CFL inserts (Fig. 39).
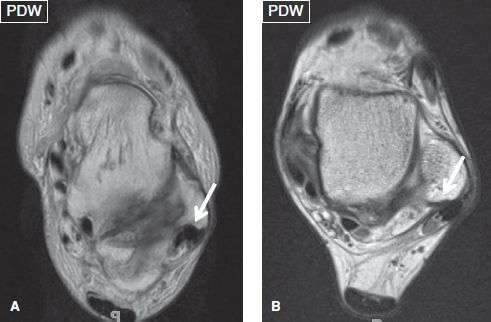
Fig. 38: Morphology of the retromalleolar groove. Axial images demonstrate a concave (arrow in A) and a flat (arrow in B) retromalleolar groove.
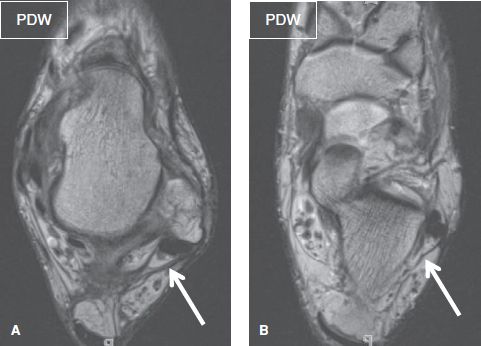
Fig. 39: Axial images (A, B) show the normal SPR (arrow in A) and IPR (arrow in B).
Similar to other tendons, the peroneal tendons are best evaluated on the axial images. The PL tendon is superficial to the PB tendon, the muscle belly of which extends inferiorly to the level of the malleolus (Fig. 40). Both tendons are contained at the retromalleolar groove by the SPR, and adjacent to the calcaneal tubercle by the IPR. They have a common tendon sheath at the level of the SPR, and separate sheaths at the level of the IPR. The PL tendon curves under the foot, courses through the cuboid sulcus and inserts as multiple fibers at the lateral aspect of the base of the first metatarsal and medial cuneiform. The PB tendon insets at the base of the fifth metatarsal bone. The PL plantarflexes the ankle, everts the foot, and supports the longitudinal and transverse foot arches during ambulation. The PB lies deep to PL and everts the foot. An accessory muscle, the peroneus quartus, may be present in up to 20% individuals (Figs. 41, 42). This accessory muscle originates from the distal fibula, PL or PB and has variable insertions on the lateral foot bones, including the peroneal retinaculum.
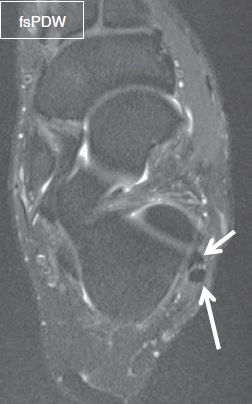
Fig. 40: Normal peroneal tendons. Axial image shows a normal crescentic-shaped peroneal brevis tendon (short arrow) and a normal oval-shaped peroneal longus tendon (long arrow).
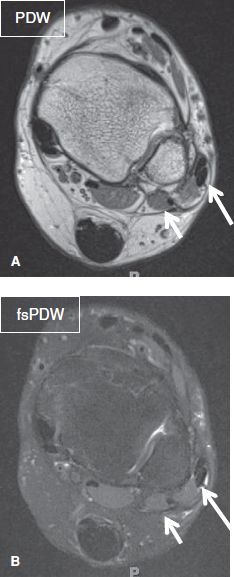
Fig. 41: Axial images (A, B) show peroneus quartus muscle (short arrows) posterior to the PL and PB tendons (long arrows).
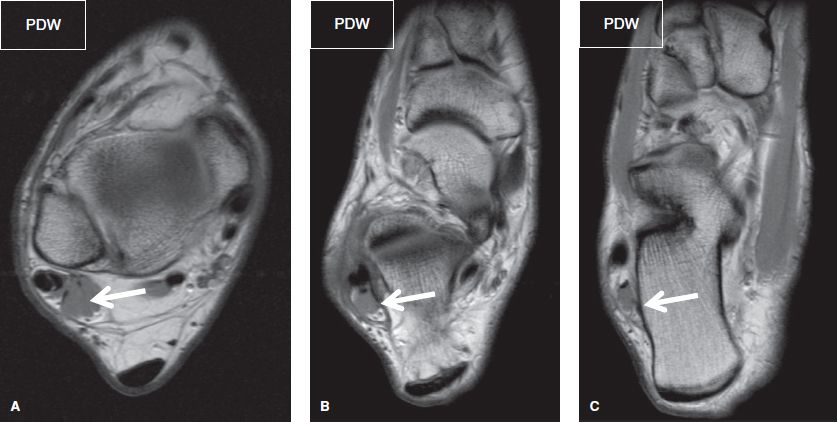
Fig. 42: Peroneus quartus muscle. Axial images (A–C). An accessory muscle is present in the lateral compartment (arrows) posterior to the peroneus longus and brevis.
The peroneal tendons frequently undergo injuries including tendinosis, tenosynovitis, tear, and dislocation. A small amount of fluid may normally be present within the peroneal tendon sheath. The fluid is considered pathologic when a) it correlates to the patient’s site of maximal pain, or b) is, circumferential about the tendon, or is greater than 2 mm in thickness when measured from the tendon edge to the synovial sheath. Apart from tenosynovitis, fluid could accumulate in the peroneal sheath in the setting of a torn CFL, which forms the floor of the peroneal tendons, or with calcaneus fracture. Peroneal tendinosis manifests as increased intrasubstance signal with or without tendon thickening. The PB and PL are considered thickened if they are equal to or larger in size than the PTT.
The PB tendon undergoes tears much more commonly than the PL tendon. Longitudinal (split) tears of the PB tendon often originate within the fibular groove, where the tendon can get entrapped between the PL tendon and the lateral malleolus. Conditions predisposing to split tear include SPR tear or laxity, flat or convex posterior aspect of the lateral malleolus, low-lying PB muscle belly (extending inferior to the tip of the lateral malleolus), peroneal tubercle hypertrophy, and presence of the accessory peroneus quartus muscle. When split, the PB tendon partially envelops the PL tendon and the split fragments encircle on either side of PL that are 2.5–5 cm in length and reconstitute distally along the length of the tendon, proximal to its insertion (Fig. 44). This creates a “Mickey Mouse ears” configuration, where the face is formed by the PL tendon and the ears by the PB subtendons. A C-shaped or boomerang (pre-split) configuration below the lateral malleolus is a degenerative variant on MR imaging and should not be overcalled as split tear. In acute cases, marrow edema of the lateral calcaneus at the retinacular attachment site may be present. One should be aware of the bifid PB or bifid peroneus quartus tendons, normal variants, in which the two tendons simulate the subtendons of a PB tendon split tear. The key to avoid misdiagnosis is the identification of separate muscle fibers about each of the bifurcated tendons (Fig. 45). In children, the PB tendon may avulse from the base of the fifth metatarsal. The bony fracture assumes a transverse orientation, which can be distinguished from the normal ossification center that is longitudinally oriented.
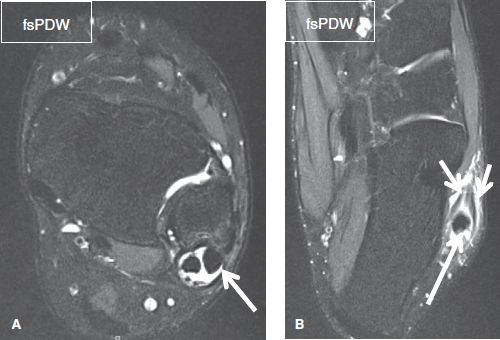
Fig. 43: Peroneal tenosynovitis and longitudinal split tear of the peroneus brevis tendon on the axial images. A: Circumferential fluid collection is evident within the common peroneal tendon sheath (arrow), in keeping with tenosynovitis. B: The peroneus brevis tendon has been divided into two separate subtendons (short arrows) which partially envelope the peroneus longus tendon (long arrow), in this case of peroneus brevis longitudinal split tear.
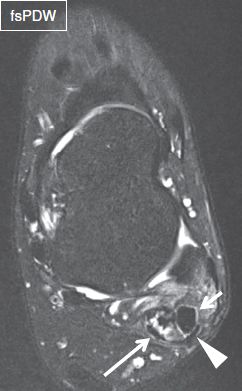
Fig. 44: Peroneus brevis tendon with multiple split tears (shredded tendon). Axial image demonstrates a normal peroneus longus tendon (short arrow), as well as multiple subtendons in the expected location of the peroneus brevis tendon (long arrow), in keeping with multiple split tears. The superior peroneal retinaculum is torn (arrowhead).

Fig. 45: Bifid peroneus brevis tendon. Axial image demonstrates the two tendons (arrows) of the peroneus brevis muscle, which originate from separate muscle fibers.
The PL tendinosis is much more common than the frank tears. PL tendinosis can be present at the retromalleolar groove or immediately above the cuboid sulcus. One should also be aware of the magic angle artifact that may cause artifactual alteration of the signal intensity of the PL tendon just above the cuboid sulcus. PL tendon tears most often occur at the level of the peroneal tubercle or the cuboid tunnel, and may be associated with lateral collateral ligament sprains and marrow edema of the cuboid or the lateral calcaneus (Figs. 46, 47). In complete PL tendon rupture, sagittal images can be prudently used to measure the tendon retraction. An os peroneum is a small round or oval-shaped accessory ossicle located immediately proximal to the base of the fifth metatarsal and within the substance of the PL tendon, adjacent to the calcaneocuboid joint (Fig. 48). Os peroneum is very common, present in about 26% of feet, may be uni- or multi-partite, and should not be erroneously interpreted as an avulsion fracture. When multi-partite, it features a synchondrosis less than 2 mm thick. The term painful os peroneum syndrome (POPS) presents as acute or chronic lateral pain, tenderness, and swelling along the course of the PL tendon. It can be caused by a wide spectrum of pathologies including os peroneum fracture, hypertrophic healing of a fractured os peroneum, diastases of a multi-partite os peroneum, attrition or tear of the PL tendon proximal or distal to the sesamoid bone, or an enlarged painful peroneal tubercle. Common imaging findings include an edematous and fragmented ossicle within the substance of a thickened partially torn PL tendon, with diastasis and retraction of the proximal fragment (Figs. 49, 50). Similar to the PB tendon, the PL tendon is more prone to tears in the setting of a peroneus quartus accessory muscle. PL tendon and PB tendon split- or complete tears can also occur simultaneously (Fig. 51). The relevant differential diagnoses include fifth metatarsal fracture, cuboid fracture, or SPR injury.
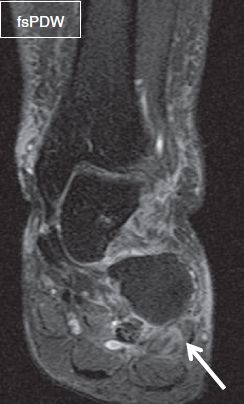
Fig. 46: Split tear of the peroneus longus tendon. Coronal image exhibits a high-grade split tear of the peroneus longus tendon (arrow) at the level of the cuboid sulcus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







