Temporomandibular Joint
The temporomandibular joints are two of the most frequently used joints in the body, but they probably receive the least amount of attention. Without these joints, we would be severely hindered when talking, eating, yawning, kissing, or sucking. In any examination of the head and neck, the temporomandibular joints should be included. Temporomandibular disorders (TMDs) consist of several complex multifactorial ailments involving many interrelating factors including psychosocial issues.1–3 Three cardinal features of TMD are orofacial pain, restricted jaw motion, and joint noise.1 Much of the work in this chapter has been developed from the teachings of Rocabado.4
Applied Anatomy
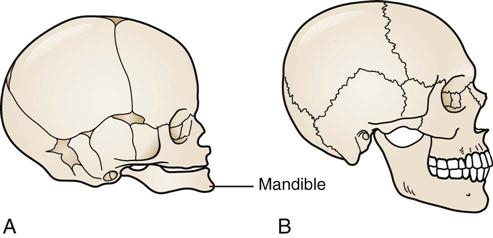
The temporomandibular joint is a synovial, condylar, modified ovoid, and hinge-type joint with fibrocartilaginous surfaces rather than hyaline cartilage5 and an articular disc; this disc completely divides each joint into two cavities (Figure 4-1). Both joints, one on each side of the jaw, must be considered together in any examination. Along with the teeth, these joints are considered to be a “trijoint complex.”
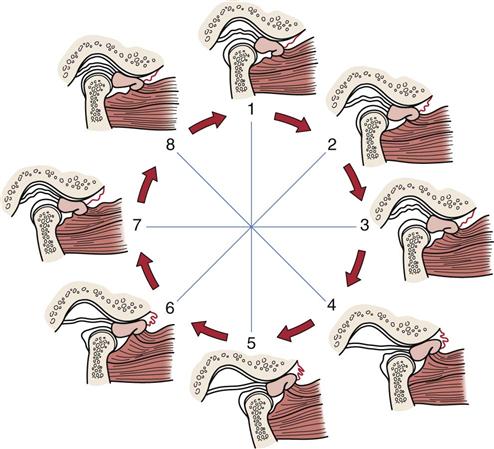
Gliding, translation, or sliding movement occurs in the upper cavity of the temporomandibular joint, whereas rotation or hinge movement occurs in the lower cavity (Figure 4-2). Rotation occurs from the beginning to the midrange of movement. The upper head of the lateral pterygoid muscle draws the disc, or meniscus, anteriorly and prepares for condylar rotation during movement. The rotation occurs through the two condylar heads between the articular disc and the condyle. In addition, the disc provides congruent contours and lubrication for the joint. Gliding, which occurs as a second movement, is a translatory movement of the condyle and disc along the slope of the articular eminence. Both gliding and rotation are essential for full opening and closing of the mouth (Figure 4-3). The capsule of the temporomandibular joints is thin and loose. In the resting position, the mouth is slightly open, the lips are together, and the teeth are not in contact but slightly apart. In the close-packed position, the teeth are tightly clenched, and the heads of the condyles are in the posterior aspect of the joint. Centric occlusion is the relation of the jaw and teeth when there is maximum contact of the teeth, and it is the position assumed by the jaw in swallowing. The position in which the teeth are fully interdigitated is called the median occlusal position.6
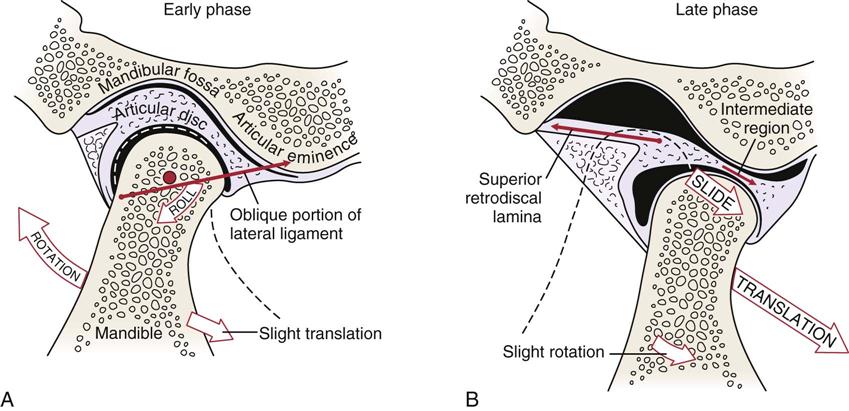
A, Early phase. B, Late phase. (Modified from Neumann DA: Kinesiology of the musculoskeletal system—foundations for physical rehabilitation, St Louis, 2002, CV Mosby, p. 360.)
Note that the disc is rotated posteriorly on the condyle as the condyle is translated out of the fossa. The closing movement is the exact opposite of the opening movement.
The temporomandibular joints actively displace only anteriorly and slightly laterally. When the mouth is opening, the condyles of the joint rest on the disc in the articular eminences, and any sudden movement, such as a yawn, may displace one or both condyles forward. As the mandible moves forward on opening, the disc moves medially and posteriorly until the collateral ligaments and lateral pterygoid stop its movement. The disc is then “seated” on the head of the mandible, and both disc and mandible move forward to full opening. If this “seating” of the disc does not occur, full range of motion at the temporomandibular joint is limited. In the first phase, mainly rotation occurs, primarily in the inferior joint space. In the second phase, in which the mandible and disc move together, mainly translation occurs in the superior joint space.7
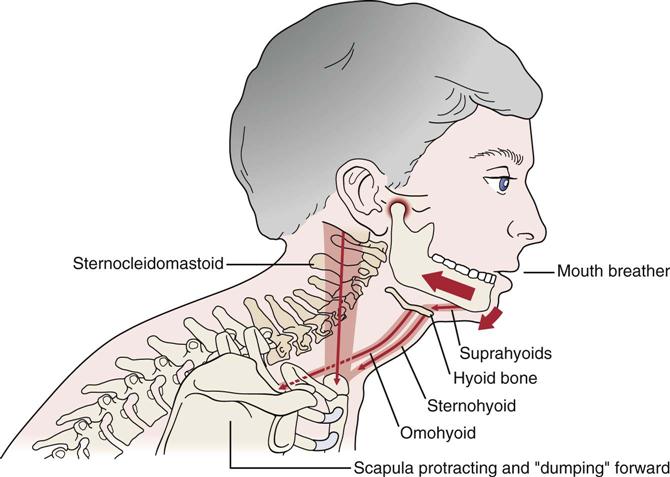
The hyoid bone, found in the anterior throat region, is sometimes referred to as the skeleton of the tongue.6 It serves as an attachment for the extrinsic tongue muscles and infrahyoid muscles and, by so doing, provides reciprocal stabilization during swallowing and through its muscle attachments can affect cervical and even shoulder function. Figure 4-4 outlines the effect of a forward head posture and the relation to the hyoid bone and related muscles.
The temporomandibular joints are innervated by branches of the auriculotemporal and masseteric branches of the mandibular nerve. The disc is innervated along its periphery but is aneural and avascular in its intermediate (force-bearing) zone.
The temporomandibular, or lateral, ligament restrains movement of the lower jaw and prevents compression of the tissues behind the condyle. In reality, this collateral ligament is a thickening in the joint capsule. The sphenomandibular and stylomandibular ligaments act as “guiding” restraints to keep the condyle, disc, and temporal bone firmly opposed. The stylomandibular ligament is a specialized band of deep cerebral fascia with thickening of the parotid fascia.
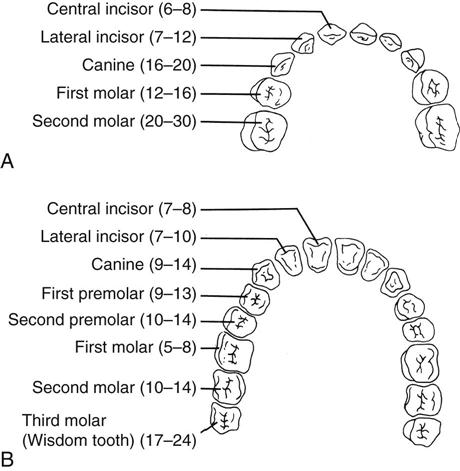
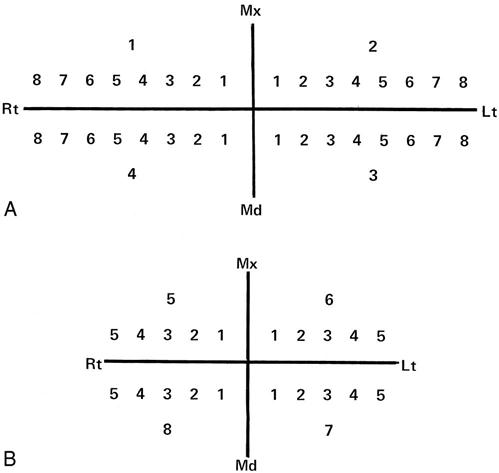
In the human, there are 20 deciduous, or temporary (“baby”), teeth and 32 permanent teeth (Figure 4-5). The temporary teeth are shed between the ages of 6 and 13 years. In the adult, the incisors are the front teeth (four maxillary and four mandibular) with the maxillary incisors being larger than the mandibular incisors. The incisors are designed to cut food. The canine teeth (two maxillary and two mandibular) are the longest permanent teeth and are designed to cut and tear food. The premolars crush and break down the food for digestion; usually they have two cusps. There are eight premolars in all, two on each side, top and bottom. The final set of teeth is the molars, which crush and grind food for digestion. They have four or five cusps, and there are two or three on each side, top and bottom (total eight to twelve). The third molars are called wisdom teeth. Missing teeth, abnormal tooth eruption, malocclusion, or dental caries (decay) may lead to problems of the temporomandibular joint. By convention, the teeth are divided into four quadrants—the upper left, the upper right, the lower left, and the lower right quadrants (Figure 4-6).
Patient History
In addition to the questions listed under Patient History in Chapter 1, the examiner should obtain the following information from the patient:8,9
1. Is there pain or restriction on opening or closing of the mouth? Pain in the fully opened position (e.g., pain associated with opening to bite an apple, yawning) is probably caused by an extra-articular problem, whereas pain associated with biting firm objects (e.g., nuts, raw fruit and vegetables) is probably caused by an intra-articular problem.10 Limited opening may be due to the disc displaced anteriorly, inert tissue tightness, or muscle spasm. Restriction can lead to anxiety in patients because of its effect on everyday activities (e.g., eating, talking).3
2. Is there pain on eating? Does the patient chew on the right? Left? Both sides equally? Loss of molars or worn dentures can lead to loss of vertical dimension, which can make chewing painful. Vertical dimension is the distance between any two arbitrary points on the face, one of these points being above and the other below the mouth, usually in midline. Often, chewing on one side is the result of malocclusion.10
3. What movements of the jaw cause pain? Do the symptoms change over a 24-hour period? The examiner should watch the patient’s jaw movement while the patient is talking. A history of stiffness on waking with pain on function that disappears as the day goes on suggests osteoarthritis.11
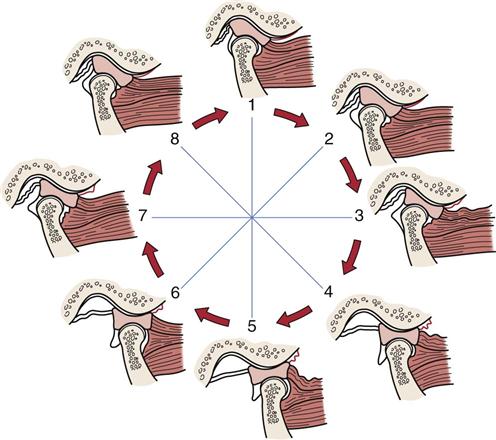
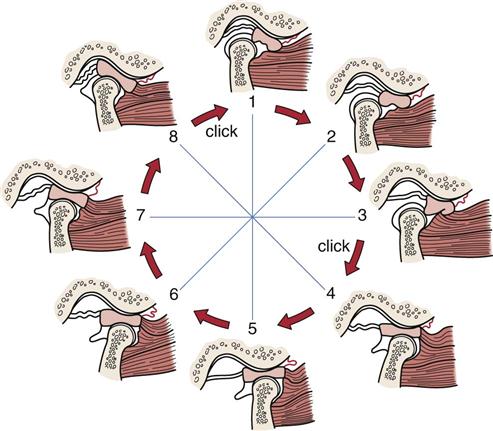
6. Has the patient complained of any crepitus or clicking? Normally, the condyles of the temporomandibular joint slide out of the concavity and onto the rim of the disc. Clicking is the result of abnormal motion of the disc and mandible. Early clicking implies a developing dysfunction, whereas late clicking is more likely to mean a chronic problem. Clicking may occur when the condyle slides back off the rim into the center (Figure 4-7).12 If the disc sticks or is bunched slightly, opening causes the condyle to move abruptly over the disc and into its normal position, resulting in a single click (see Figure 4-7).13 There may be a partial anterior displacement (subluxation) or dislocation of the disc, which the condyle must override to reach its normal position when the mouth is fully open (Figure 4-8). This override may also cause a click. Similarly, a click may occur if the disc is displaced anteriorly and/or medially, causing the condyle to override the posterior rim of the disc later than normal during mouth opening. This is referred to as disc displacement with reduction. If clicking occurs in both directions, it is called reciprocal clicking (Figure 4-9). The opening click occurs somewhere during the opening or protrusive path, and the click indicates the condyle is slipping over the thicker posterior border of the disc to its position in the thinner middle or intermediate zone. The closing (reciprocal) click occurs near the end of the closing or retrusive path as the pull of the superior lateral pterygoid muscle causes the disc to slip more anteriorly and the condyle to move over its posterior border.
Clicks may also be caused by adhesions (Figure 4-10), especially in people who clench their teeth (bruxism). These “adhesive” clicks occur in isolation, after the period of clenching.14 If adhesions occur in the superior or inferior joint space, translation or rotation will be limited. This presents as a temporary closed lock, which then opens with a click.
If the articular eminence is abnormally developed (i.e., short, steep posterior slope or long, flat anterior slope), the maximum anterior movement of the disc may be reached before maximum translation of the condyle has occurred. As the condyle overrides the disc, a loud crack is heard, and the condyle-disc leaps or jogs (subluxes) forward.14
“Soft” or “popping” clicks that are sometimes heard in normal joints are caused by ligament movement, articular surface separation, or sucking of loose tissue behind the condyle as it moves forward. These clicks usually result from muscle incoordination. “Hard” or “cracking” clicks are more likely to indicate joint pathology or joint surface defects. Soft crepitus (like rubbing knuckles together) is a sound that sometimes occurs in symptomless joints and is not necessarily an indication of pathology.15 Hard crepitus (like a footstep on gravel) is indicative of arthritic changes in the joints. The clicking may be caused by uncoordinated muscle action of the lateral pterygoid muscles, a tear or perforation in the disc, osteoarthrosis, or occlusal imbalance. Normally, the upper head of the lateral pterygoid muscle pulls the disc forward. If the disc does not move first, the condyle clicks over the disc as it is pulled forward by the lower head of the lateral pterygoid muscle. Iglarsh and Snyder-Mackler7 have divided disc displacement into four stages (Table 4-1).
7. Has the mouth or jaw ever locked? Locking may imply that the mouth does not fully open or it does not fully close and is often related to problems of the disc or joint degeneration. Locking is usually preceded by reciprocal clicking. If the jaw has locked in the closed position, the locking is probably caused by a disc with the condyle being posterior or anteromedial to the disc. Even if translation is blocked (e.g., “locked” disc), the mandible can still open 30 mm by rotation. If there is functional dislocation of the disc with reduction (see Figure 4-8), the disc is usually positioned anteromedially, and opening is limited. The patient complains that the jaw “catches” sometimes, so the locking occurs only occasionally and, at those times, opening is limited. If there is functional anterior dislocation of the disc without reduction, a closed lock occurs. Closed lock implies there has been anterior and/or medial displacement of the disc so that the disc does not return to its normal position during the entire movement of the condyle. In this case, opening is limited to about 25 mm, the mandible deviates to the affected side (Figure 4-11), and lateral movement to the uninvolved side is reduced.14 If locking occurs in the open position, it is probably caused by subluxation of the joint or possibly by posterior disc displacement (see Figure 4-11). With an open lock, there are two clicks on opening, when the condyle moves over the posterior rim of the disc and then when it moves over the anterior rim of the disc, and two clicks on closing. If, after the second click occurs on opening, the disc lies posterior to the condyle, it may not allow the condyle to slide back (Figure 4-12).16 If the condyle dislocates outside the fossa, it is a true dislocation with open lock; the patient cannot close the mouth, and the dislocation must be reduced.16
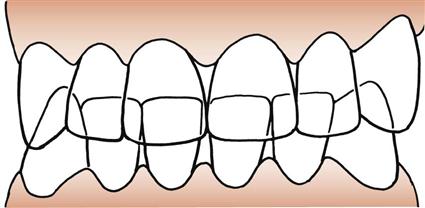
9. Does the patient grind the teeth or hold them tightly? Bruxism is the forced clenching and grinding of the teeth, especially during sleep. This may lead to facial, jaw, or tooth pain, or headaches in the morning along with muscle hypertrophy. If the front teeth are in contact and the back ones are not, facial and temporomandibular pain may develop as a result of malocclusion. Normally, the upper teeth cover the upper one third of the bottom teeth (Figure 4-13).
10. Does there appear to be any related psychosocial problems? Temporomandibular dysfunction is often accompanied by related psychosocial issues.1,17 Table 4-2 outlines psychosocial factors that may affect the temporomandibular joint.
11. Are any teeth missing? If so, which ones, and how many? The presence or absence of teeth and their relation to one another must be noted on a table similar to the one shown in Figure 4-6. Their presence or absence can have an effect on the temporomandibular joints and their muscles. If some teeth are missing, others may deviate to fill in the space, altering the occlusion.
13. Does the patient have any difficulty swallowing? Does the patient swallow normally or gulp? What happens to the tongue when the patient swallows? Does it move normally, anteriorly, or laterally? Is there any evidence of tongue thrust or thumb sucking? For example, the facial nerve (cranial nerve VII) and the trigeminal nerve (cranial nerve V), which control facial expression and mastication and contribute to speech, also control anterior lip seal. If lip seal is weakened, the teeth may move anteriorly, an action that would be accentuated in “tongue thrusters.” The normal resting position of the tongue is against the anterior palate (Figure 4-14). It is the position in which one would place the tongue to make a “clicking” sound.
16. Has the patient noticed any voice changes? Changes may be caused by muscle spasm.
18. Does the patient ever feel dizzy or faint?
19. Has the patient ever worn a dental splint? If so, when? For how long?
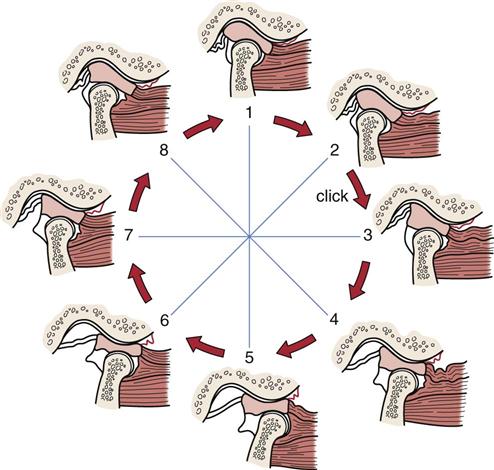
Between positions 2 and 3, a click is felt as the condyle moves across the posterior border into the intermediate zone of the disc. Normal condyle-disc function occurs during the remaining opening and closing movement. In the closed joint position (1), the disc is again displaced forward (and medially) by activity of the superior lateral pterygoid muscle.
During opening, the condyle passes over the posterior border of the disc into the intermediate area of the disc, thus reducing the dislocated disc.
Between positions 2 and 3, a click is felt as the condyle moves across the posterior border of the disc. Normal condyle-disc function occurs during the remaining opening and closing movement until the closed joint position is approached. A second click is heard as the condyle once again moves from the intermediate zone to the posterior border of the disc between positions 8 and 1.
TABLE 4-1
Temporomandibular Disc Dysfunction
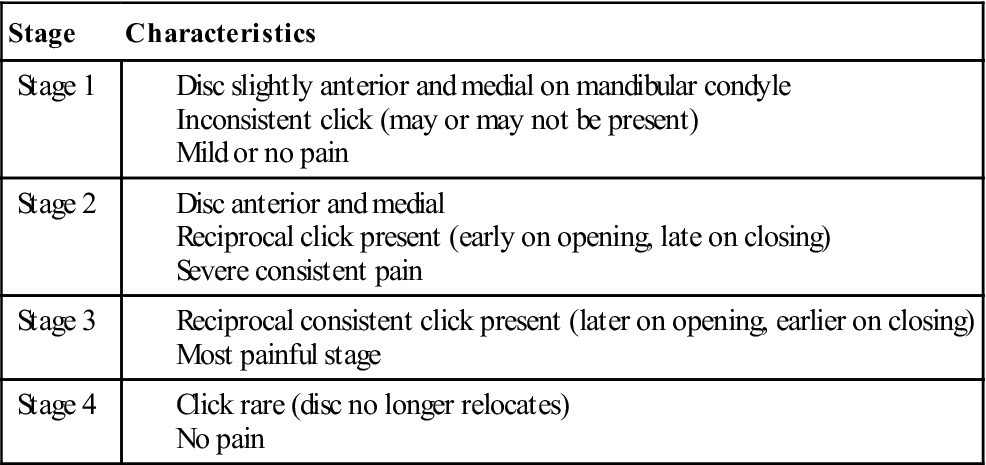
Data from Iglarsh ZA, Snyder-Mackler L: Tempormandibular joint and the cervical spine. In Richardson JK, Iglarsh ZA (editors): Clinical orthopedic physical therapy, Philadelphia, 1994, WB Saunders.
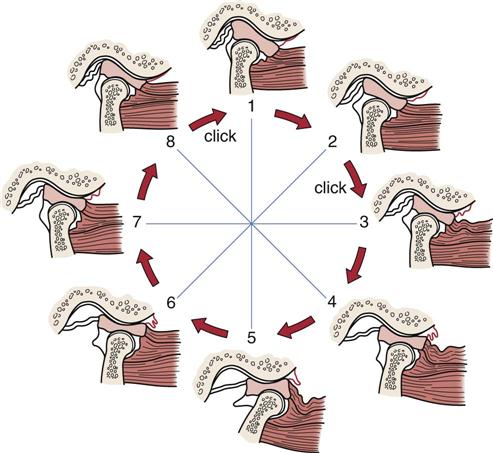
The condyle never assumes a normal relation to the disc but instead causes the disc to move forward ahead of it. This condition limits the distance the condyle can translate forward.
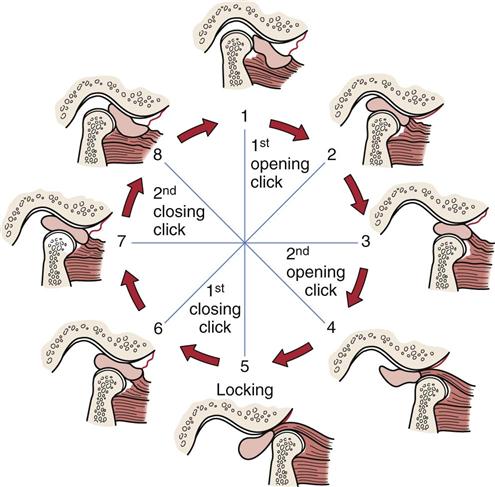
1, The disc always stays in anterior position with the jaw closed. 1-4, Disc is displaced posterior to the condyle with one or two opening clicks. 5-6, The disc disturbs jaw closing after maximum opening. 6-1, The disc is again displaced to anterior position from the posterior with one or two clicks.
TABLE 4-2
Checklist of Psychological and Behavioral Factors*
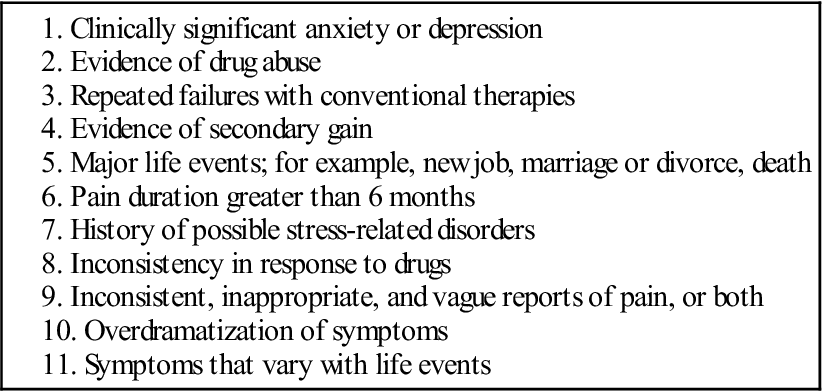
*Note: The first two factors are the most significant and warrant further evaluation by a mental health professional; factors 3 to 6 need at least one more factor for consideration of referral; and factors 7 to 11 require three or more factors for consideration of referral to a mental health professional.
From McNeill C, Mohl ND, Rugh JD, et al: Temporomandibular disorders: diagnosis, management, education and research. J Am Dent Assoc 120:259, 1990.
Observation
When assessing the temporomandibular joints, the examiner must also assess the posture of the cervical spine and head. For example, it is necessary that the head be “balanced” on the cervical spine and be in proper postural alignment.
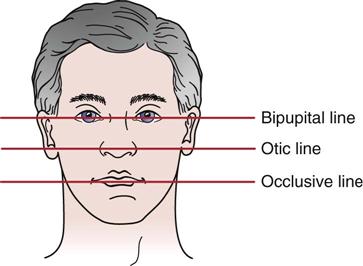
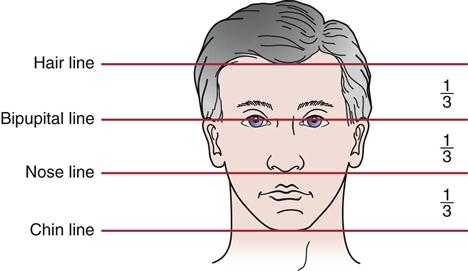
1. Is the face symmetrical horizontally and vertically, and are facial proportions normal (Figure 4-15)? The examiner should check the eyebrows, eyes, nose, ears, and corners of the mouth for symmetry on both horizontal and vertical planes. Horizontally, the face of an adult is divided into thirds (Figure 4-16); this demonstrates normal vertical dimension. Usually the upper and lower teeth are used to measure vertical dimension. The horizontal bipupital, otic, and occlusive lines should be parallel to each other (Figure 4-17). Loss of teeth on one side can lead to convergence in which at least two of the lines may converge because the jaw line is short on one side relative to the other. A quick way to measure the vertical dimension is to measure from the lateral edge of the eye to the corner of the mouth and from the nose to the chin (Figure 4-18). Normally, the two measurements are equal. If the second measurement is smaller than the first by 1 mm or more, there has been a loss of vertical dimension, which may have resulted from loss of teeth, overbite, or temporomandibular joint dysfunction. In children, elderly persons, and those with massive tooth loss, the lower third of the face is not well developed (lack of teeth) or has recessed (Figure 4-19). As the teeth grow, the lower third develops into its normal proportion. The examiner should notice whether there is any paralysis, which could be indicated by ptosis (drooping of an eyelid) or by drooping of the mouth on one side (Bell palsy).
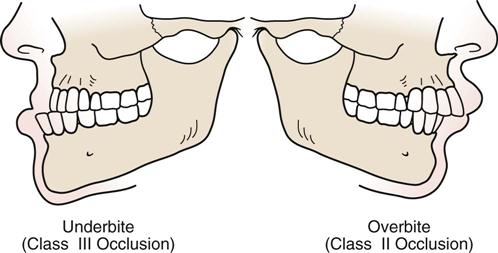
2. The examiner should note whether the teeth are normally aligned or there is any crossbite, underbite, or overbite (Figure 4-20). With crossbite, the teeth of the mandible are lateral to the upper (maxillary) teeth on one side and medial on the opposite side. There is abnormal interdigitation of the teeth. With anterior crossbite, the lower incisors are ahead of the upper incisors. With posterior crossbite, there is a transverse abnormal relation of the teeth. In underbite, the mandibular teeth are unilaterally, bilaterally, or in pairs in buccoversion (i.e., they lie anterior to the maxillary teeth). In overbite, the anterior maxillary incisors extend below the anterior mandibular incisors when the jaw is in centric occlusion. A small amount of overbite (2 to 3 mm) anteriorly is the most common position of the teeth. This is because the maxillary arch is slightly longer than the mandibular arch. Overjet (Figure 4-21) is the distance that the maxillary incisors close over the mandibular incisors when the mouth is closed. This distance is normally 2 to 3 mm. Occlusal interference refers to premature teeth contact, which tends to deflect the jaw laterally and/or anteriorly.18 Any orthodontic appliances or false teeth present should also be evaluated for fit and possible sore spots.
3. The examiner should note whether there is any malocclusion that may result in a faulty bite. Malocclusion may be a major factor in the development of disc problems of the temporomandibular joints. Occlusion occurs when the teeth are in contact and the mouth is closed. Malocclusion is defined as any deviation from normal occlusion. Class I occlusion refers to the normal anteroposterior relation of the maxillary teeth to mandibular teeth. A slight modification with only the incisors affected and overjet slightly larger is sometimes classified as a Class I malocclusion. Class II malocclusion (overbite) occurs when the mandibular teeth are positioned posterior to their normal position relative to the maxillary teeth. This malocclusion deformity involves all the teeth, including the molars. The designation Class II Division 1 malocclusion (also called large overjet or horizontal overlap) indicates that the maxillary incisors demonstrate significant overjet. Class II Division 2 malocclusion (also called deep overbite or vertical overlap) implies that overjet is not significant but that there is overbite and lateral flaring of the lateral maxillary incisors.19 Class III malocclusion (i.e., underbite) occurs when the mandibular teeth are positioned anterior to their normal position relative to the maxillary teeth. If maxillary and mandibular teeth are on the same vertical plane, a Class III malocclusion would be present.
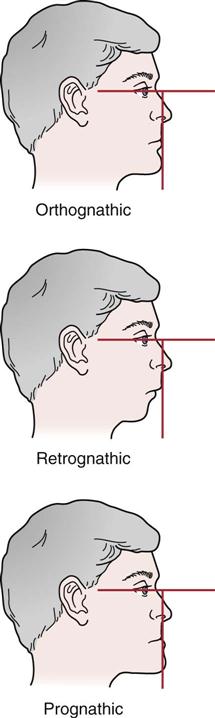
4. What is the facial profile? The orthognathic profile is the normal, “straight-jawed” form. With this facial profile, a vertical line dropped perpendicular to the bipupital line would touch the upper and lower lips and the tip of the chin. In a person with a retrognathic profile, the chin would lie behind the vertical line and the person would be said to have a “receding chin.” With the prognathic profile, the chin would be in front of the vertical line and the person would have a protruded or “strong” chin (Figure 4-22).19
5. The examiner should note whether the patient demonstrates normal bony and soft-tissue contours. When the patient bites down, do the masseter muscles bulge as they normally should? Hypertrophy caused by overuse may lead to abnormal wear of the teeth. When looking at the soft tissues, it is important to note symmetry. The upper lip should normally cover two thirds of the maxillary teeth at rest. If it does not, the lip is said to be short.7 If the lip can be drawn over the upper teeth, however, the upper lip is said to be functional, and no treatment is necessary. The lower lip normally covers the mandibular teeth and, when the mouth is closed, part of the maxillary teeth.
6. Is the patient able to move the tongue properly? Can the patient move the tongue up to and against the palate? Can the tongue be protruded or rolled? Is the patient able to “click” the tongue? Tongue thrusting refers to forward movement of the tongue, usually to push against the lower teeth; it also occurs when the tongue is pushed against the upper teeth and the lower teeth are closed firmly against it, creating an oral seal.20 Tongue thrusters find it easier to thrust the tongue if the head is protruded. Therefore, to test for tongue thrusting, the patient’s head posture is corrected and the patient is asked to swallow. In the tongue thruster, swallowing causes the tongue to move forward resulting in protrusion of the head. Tongue thrusting may be due to hyperactivity of the masticatory muscles. When one swallows, the hyoid bone should move up and down quickly. If it moves only upward and slowly, and the suboccipital muscles posteriorly contract, it is suggestive of a tongue thrust.21

Look for asymmetry both vertically and horizontally. Asymmetrical changes may be seen with no smile (A) or with smile (B). These asymmetrical differences may or may not be related to pathology.
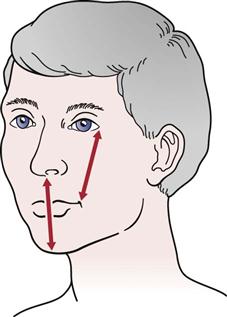
Normally, the distance from the lateral edge of the eye to the corner of the mouth equals the distance from nose to point of chin.
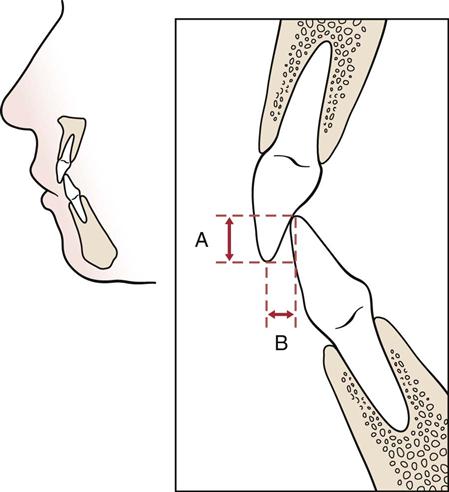
A, Vertical overlap (overbite). B, Horizontal overlap (overjet). (Redrawn from Friedman MH, Weisberg J: The temporomandibular joint. In Gould JA, editor: Orthopedics and sports physical therapy, St Louis, 1990, CV Mosby, p. 578.)
Examination
The examiner must remember that many problems of the temporomandibular joints may be the result of or related to problems in the cervical spine or teeth. Therefore, the cervical spine is at least partially included in any temporomandibular assessment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree