Thoracic (Dorsal) Spine
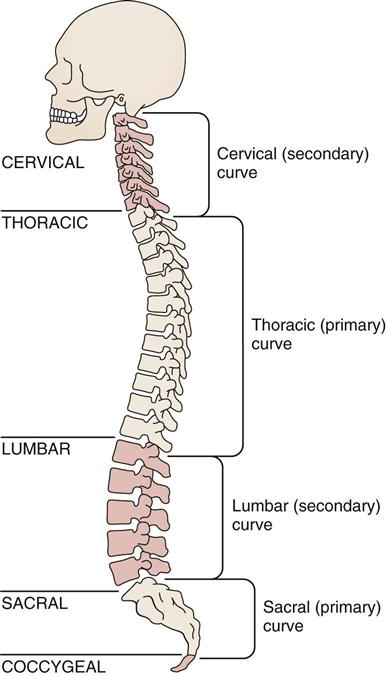
Assessment of the thoracic spine involves examination of the part of the spine that is most rigid because of the associated rib cage. The rib cage in turn provides protection for the heart and lungs. Normally, the thoracic spine, being one of the primary curves, exhibits a mild kyphosis (posterior curvature); the cervical and lumbar sections, being secondary curves, exhibit a mild lordosis (anterior curvature). When the examiner assesses the thoracic spine, it is essential that the cervical and/or lumbar spines be evaluated at the same time (Figure 8-1; see Figure 3-7).
Applied Anatomy
The costovertebral joints are synovial plane joints located between the ribs and the vertebral bodies (Figure 8-2). There are 24 of these joints, and they are divided into two parts. Ribs 1, 10, 11, and 12 articulate with a single vertebra. The other articulations have no intra-articular ligament that divides the joint into two parts, so each of ribs 2 through 9 articulates with two adjacent vertebrae and the intervening intervertebral disc. The main ligament of the costovertebral joint is the radiate ligament, which joins the anterior aspect of the head of the rib radiating to the sides of the vertebral bodies and disc in between. For ribs 10, 11, and 12, it attaches only to the adjacent vertebral body. The intra-articular ligament divides the joint and attaches to the disc.
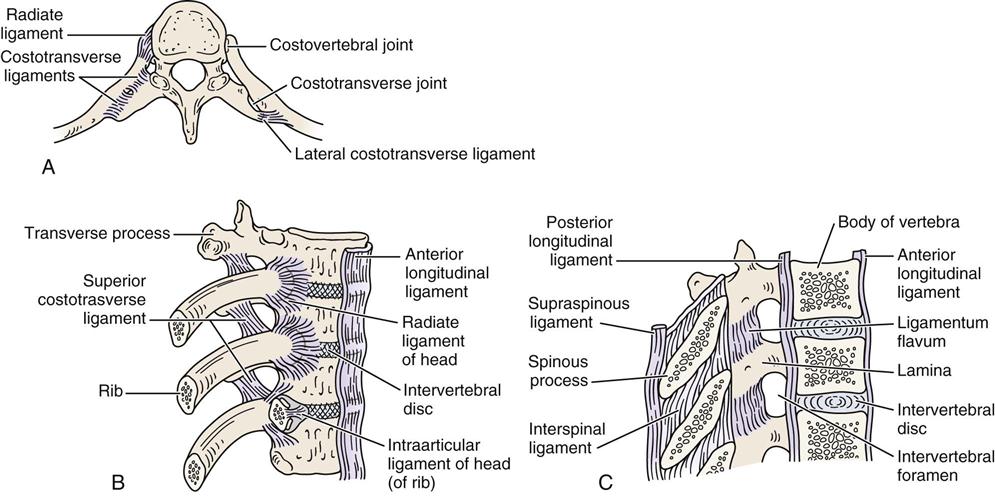
A, Superior view. B, Anterolateral aspect. C, Median section through vertebra.
The costotransverse joints are synovial joints found between the ribs and the transverse processes of the vertebra of the same level for ribs 1 through 10 (see Figure 8-2). Because ribs 11 and 12 do not articulate with the transverse processes, this joint does not exist for these two levels. The costotransverse joints are supported by three ligaments. The superior costotransverse ligament runs from the lower border of the transverse process above to the upper border of the rib and its neck. The costotransverse ligament runs between the neck of the rib and the transverse process at the same level. The lateral costotransverse ligament runs from the tip of the transverse process to the adjacent rib.
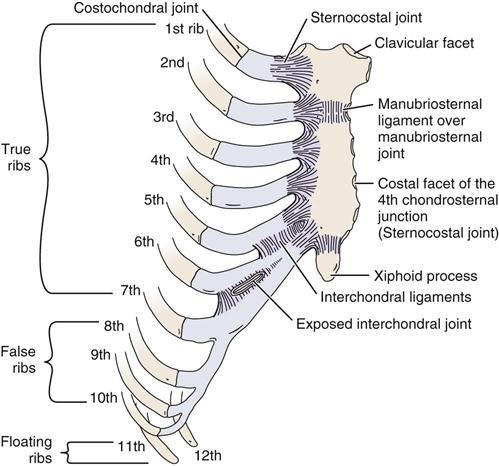
The costochondral joints lie between the ribs and the costal cartilage (Figure 8-3). The sternocostal joints are found between the costal cartilage and the sternum. Joints 2 through 6 are synovial, whereas the first costal cartilage is united with the sternum by a synchondrosis. Where a rib articulates with an adjacent rib or costal cartilage (ribs 5 through 9), a synovial interchondral joint exists.
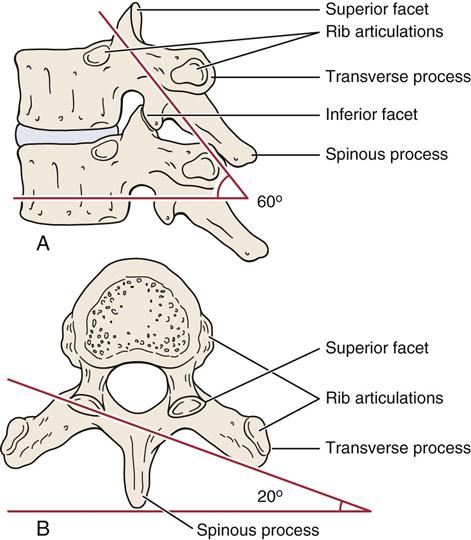
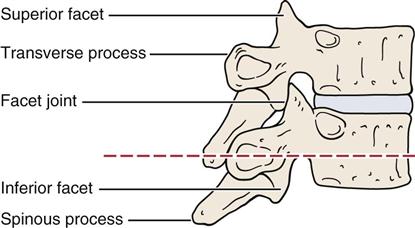
As in the cervical and lumbar spines, the two apophyseal or facet joints make up the main tri-joint complex along with the disc between the vertebrae. The superior facet of the T1 vertebra is similar to a facet of the cervical spine. Because of this, T1 is classified as a transitional vertebra. The superior facet faces up and back; the inferior facet faces down and forward. The T2 to T11 superior facets face up, back, and slightly laterally; the inferior facets face down, forward, and slightly medially (Figure 8-4). This shape enables slight rotation in the thoracic spine. Thoracic vertebrae T11 and T12 are classified as transitional, and the facets of these vertebrae become positioned in a way similar to those of the lumbar facets. The superior facets of these two vertebrae face up, back, and more medially; the inferior facets face forward and slightly laterally. The ligaments between the vertebral bodies include the ligamentum flavum, the anterior and posterior longitudinal ligaments, the interspinous and supraspinous ligaments, and the intertransverse ligament. These ligaments are found in the cervical, thoracic, and lumbar spine. The close packed position of the facet joints in the thoracic spine is extension.
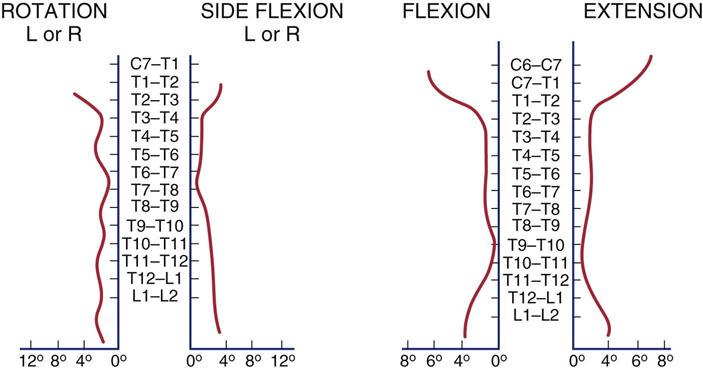
Within the thoracic spine, there are 12 vertebrae, which diminish in size from T1 to T3 and then increase progressively in size to T12. These vertebrae are distinctive in having facets on the body and transverse processes for articulation with the ribs. The spinous processes of these vertebrae face obliquely downward (Figure 8-5 ). T7 has the greatest spinous process angulation, whereas the upper three thoracic vertebrae have spinous processes that project directly posteriorly. In other words, the spinous process of these vertebrae is on the same plane as the transverse processes of the same vertebrae.
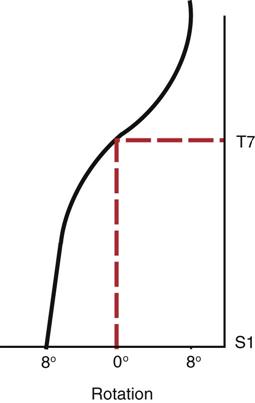
T4 to T6 vertebrae have spinous processes that project downward slightly. In this case, the tips of the spinous processes are on a plane halfway between their own transverse processes and the transverse processes of the vertebrae below. For T7, T8, and T9 vertebrae, the spinous processes project downward, the tip of the spinous processes being on a plane of the transverse processes of the vertebrae below. For the T10 spinous process, the arrangement is similar to that of the T9 spinous process (i.e., the spinous process is level with the transverse process of the vertebra below). For T11, the arrangement is similar to that of T6 (i.e., the spinous process is halfway between the two transverse processes of the vertebra), and T12 is similar to T3 (i.e., the spinous process is level with the transverse process of the same vertebra). The location of the spinous processes becomes important if the examiner wishes to perform posteroanterior central vertebral pressures (PACVPs). For example, if the examiner pushes on the spinous process of T8, the body of T9 also moves. In fact, the vertebral body of T8 probably arcs backwards slightly, whereas T9 will move in an anterior direction. T7 is sometimes classified as a transitional vertebra, because it is the point at which the lower limb axial rotation alternates with the upper limb axial rotation (Figure 8-6).
The ribs, which help to stiffen the thoracic spine, articulate with the demifacets on vertebrae T2 to T9. For T1 and T10, there is a whole facet for ribs 1 and 10, respectively. The first rib articulates with T1 only, the second rib articulates with T1 and T2, the third rib articulates with T2 and T3, and so on. Ribs 1 through 7 articulate with the sternum directly and are classified as true ribs (see Figure 8-3). Ribs 8 through 10 join directly with the costocartilage of the rib above and are classified as false ribs. Ribs 11 and 12 are classified as floating ribs, because they do not attach to either the sternum or the costal cartilage at their distal ends. Ribs 11 and 12 articulate only with the bodies of the T11 and T12 vertebrae, not with the transverse processes of the vertebrae, nor with the costocartilage of the rib above. The ribs are held by ligaments to the body of the vertebra and to the transverse processes of the same vertebrae. Some of these ligaments also bind the rib to the vertebra above.
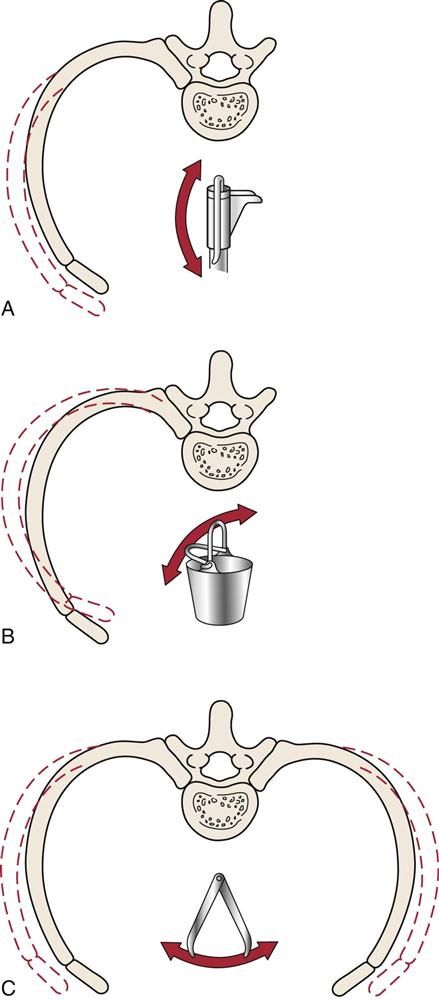
At the top of the rib cage, the ribs are relatively horizontal. As the rib cage descends, they run more and more obliquely downward. By the 12th rib, the ribs are more vertical than horizontal. With inspiration, the ribs are pulled up and forward; this increases the anteroposterior diameter of the ribs. The first six ribs increase the anteroposterior dimension of the chest, mainly by rotating around their long axes. Rotation downward of the rib neck is associated with depression, whereas rotation upward of the same portion is associated with elevation. These movements are known as a pump handle action and are accompanied by elevation of the manubrium sternum upward and forward (Figure 8-7, A).1–3 Ribs 7 through 10 mainly increase in lateral, or transverse, dimension. To accomplish this, the ribs move upward, backward, and medially to increase the infrasternal angle, or they move downward, forward, and laterally to decrease the angle. These movements are known as a bucket handle action. This action is also performed by ribs 2 through 6 but to a much lesser degree (Figure 8-7, B). The lower ribs (ribs 8 through 12) move laterally, in what is known as a caliper action, to increase lateral diameter (Figure 8-7, C).2 The ribs are quite elastic in children, but they become increasingly brittle with age. In the anterior half of the chest, the ribs are subcutaneous; in the posterior half, they are covered by muscles.
Patient History
A thorough and complete history should include past and present problems. By listening carefully, the examiner is often able to identify the patient’s problem, develop a working diagnosis, and then use the observation and examination to confirm or refute the impressions established from the history. All information concerning the present pain and its site, nature, and behavior is important. If any part of the history implicates the cervical or lumbar spine, the examiner must include these areas in the assessment as well.
In addition to the questions listed under the “Patient History” section in Chapter 1, the examiner should obtain the following information from the patient:
2. What was the mechanism of injury? Most commonly, rib injuries are caused by trauma. Thoracic spine problems may result from disease processes (e.g., scoliosis) and may have an insidious onset. Pain from true thoracic trauma tends to be localized to the area of injury. Facet syndromes present as stiffness and local pain, which can be referred.4,5
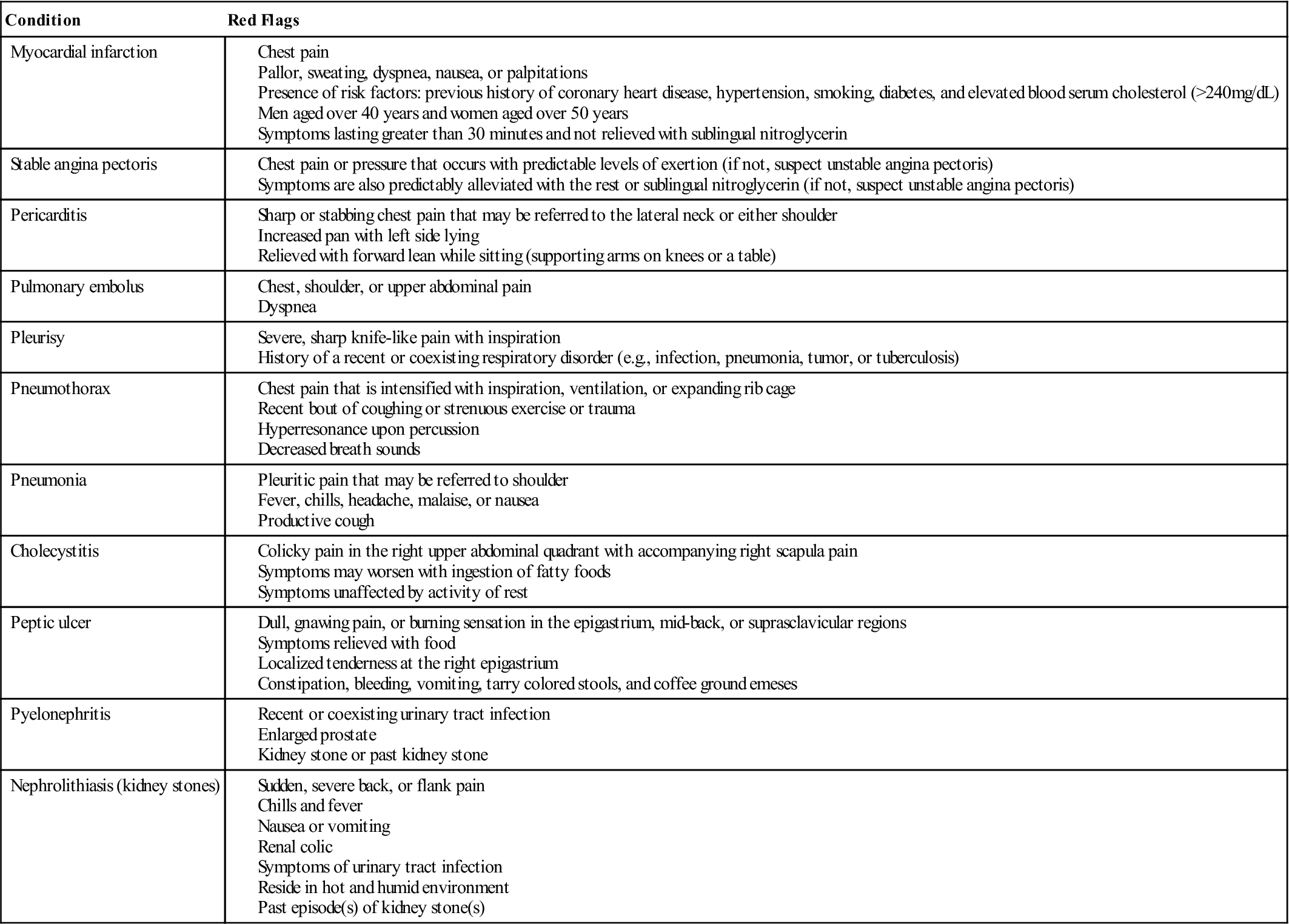
3. What are the details of the present pain and other symptoms? What are the sites and boundaries of the pain? Have the patient point to the location or locations. Is there any radiation of pain? The examiner should remember that many of the abdominal structures, such as the stomach, liver, and pancreas, may refer pain to the thoracic region (Tables 8-1 and 8-2 for thoracic spine and rib cage red flags and chest pain patterns). With thoracic disc lesions, because of the rigidity of the thoracic spine, active movements do not often show the characteristic pain pattern, and sensory and strength deficits are difficult if not impossible to detect.6 Thoracic root involvement or spondylosis usually causes pain that follows the path of the ribs or a deep, “through-the-chest” pain.
5. Is the pain deep, superficial, shooting, burning, or aching? Thoracic nerve root pain is often severe and is referred in a sloping band along an intercostal space. Pain between the scapulae may be the result of a cervical lesion. It has been reported that any symptoms above a line joining the inferior angles of the scapula should be considered of cervical origin until proven otherwise, especially if there is no history of trauma.7
9. Is the condition improving, becoming worse, or staying the same?
10. Does any particular posture bother the patient?
13. Does the patient have any problems with digestion? Pain may be referred to the thoracic spine or ribs from pathological conditions within the thorax or abdomen. Visceral pain tends to be vague, dull, and indiscrete and may be accompanied by nausea and sweating. It tends to follow dermatome patterns in its referral. For example, cardiac pain is referred to the shoulder (C4) and posteriorly to T2. Stomach pain is referred to T6–T8 posteriorly. Ulcers may be referred to T4–T6 posteriorly.4
14. Is the skin in the thorax area normal? Conditions, such as herpes zoster, can cause unilateral, spontaneous pain. In the observation, the examiner should watch for erythema and grouped vesicles.6
![]() TABLE 8-1
TABLE 8-1
Thoracic Spine and Rib Cage Red Flags
From Dutton M: Dutton’s orthopedic examination, evaluation and intervention, ed 3, New York, 2012, McGraw Hill, p. 1247.
![]() TABLE 8-2
TABLE 8-2
| Origin of Pain | Site of Referred Pain | Type of Disorder |
| Substernal or retrosternal | Neck, jaw, back, left shoulder and arm, and abdomen | Angina |
| Substernal, anterior chest | Neck, jaw, back, and bilateral arms | Myocardial infarction |
| Substernal or above the sternum | Neck, upper back, upper trapezius, supraclavicular area, left arm, and costal margin | Pericarditis |
| Anterior chest (thoracic aneurysm); abdomen (abdominal aneurysm) | Posterior thoracic, chest, neck, shoulders, interscapular, or lumbar region | Dissecting aortic aneurysm |
| Variable | Variable, depending on structures involved | Musculoskeletal |
| Costochondritis (inflammation of the costal cartilage): sternum and rib margins | Abdominal oblique trigger points: pain referred up into the chest area | |
| Upper rectus abdominis trigger points (left side), pectoralis, serratus anterior, and sternalis muscles: precordial pain | Pectoralis trigger points: pain referred down medial bilateral arms along ulnar nerve distribution (fourth and fifth fingers) | |
| Precordium region (upper central abdomen and diaphragm) | Sternum, axillary lines, and either side of vertebrae; lateral and anterior chest wall; occasionally to one or both arms | Neurological |
| Substernal, epigastric, and upper abdominal quadrants | Around chest area, shoulders, and upper back region | Gastrointestinal |
| Within breast tissue; may be localized in pectoral and supraclavicular regions | Chest area, axilla, mid-back, and neck and posterior shoulder girdle | Breast pain |
| Commonly substernal and anterior chest region | No referred pain | Anxiety |
From Dutton M: Dutton’s orthopedic examination, evaluation and intervention, ed 3, New York, 2012, McGraw Hill, p. 1246.
Observation
The patient must be suitably undressed so that the body is exposed as much as possible. In the case of a female, the bra is often removed to provide a better view of the spine and rib cage. The patient is usually observed first standing and then sitting.
As with any observation, the examiner should note any alteration in the overall spinal posture (see Chapter 15), because it may lead to problems in the thoracic spine. It is important to observe the total body posture from the head to the toes and look for any deviation from normal (Figure 8-8). Posteriorly, the medial edge of the spine of the scapula should be level with the T3 spinous process, whereas the inferior angle of the scapula is level with the T7–T9 spinous process, depending on the size of the scapula. The medial border of the scapula is parallel to the spine and approximately 5 cm lateral to the spinous processes.
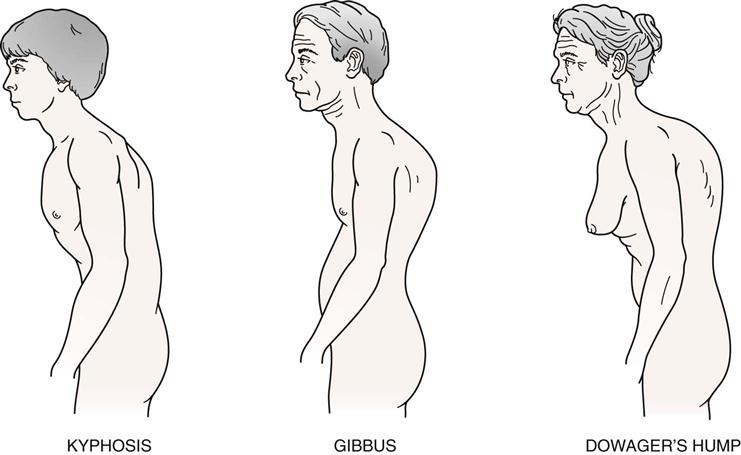
Kyphosis
Kyphosis is a condition that is most prevalent in the thoracic spine (Figure 8-9). The examiner must ensure that a kyphosis is actually present, remembering that a slight kyphosis, or posterior curvature, is normal and is found in every individual. Hyperkyphosis is a kyphotic angle of greater than 40° commonly measured by the Cobb method (see Figure 8-53) on a lateral x-ray measuring between T4 and T12.8 After age 40, the thoracic kyphosis tends to increase.8 In addition, some people have “flat” scapulae, which give the appearance of an excessive kyphosis, as does winging of the scapulae. The examiner must ensure that it is actually the spine that has the excessive curvature. Types of kyphotic deformities are shown in Figure 8-10 and listed below9:
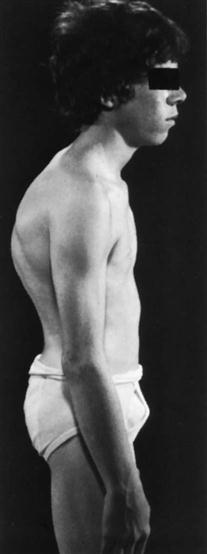
1. Round back is decreased pelvic inclination (20°) with a thoracolumbar or thoracic kyphosis (Figure 8-11). Most forms of kyphosis seen show a decreased pelvic inclination. To compensate and maintain the body’s center of gravity, a structural kyphosis, usually caused by tight soft tissues from prolonged postural change or by a growth disturbance results, causing a round back deformity.
2. Scheuermann’s disease is the most common structural kyphosis in adolescents but can occur in adults. Its etiology is unknown.10
3. Hump back is a localized, sharp, posterior angulation called a gibbus.8 This kyphotic deformity is usually structural and often results from an anterior wedging of the body of one or two thoracic vertebrae. The wedging may be caused by a fracture, tumor, or bone disease. The pelvic inclination is usually normal (30°).
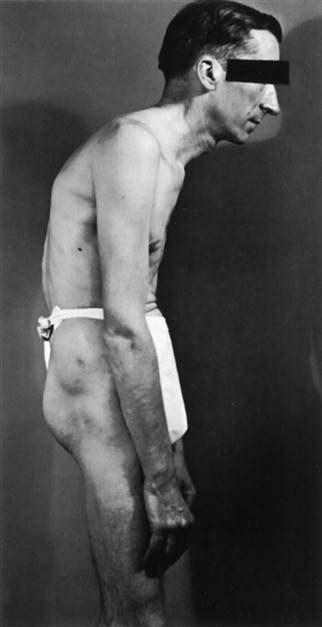
5. Dowager’s hump8 results from postmenopausal osteoporosis. Because of the osteoporosis, anterior wedge fractures occur to several vertebrae, usually in the upper to middle thoracic spine, causing a structural scoliosis that also contributes to a decrease in height.
Scoliosis
Scoliosis is a deformity in which there are one or more lateral curvatures of the lumbar or thoracic spine; it is this spinal deformity that was suffered by the “Hunchback of Notre Dame.” (In the cervical spine, the condition is called torticollis.) The curvature may occur in the thoracic spine alone, in the thoracolumbar area, or in the lumbar spine alone (Figure 8-12). Scoliosis may be nonstructural (i.e., relatively easily correctable once the cause is determined) or structural. Poor posture, hysteria, nerve root irritation, inflammation in the spine area, leg length discrepancy, or hip contracture can cause nonstructural scoliosis. Structural changes may be genetic, idiopathic, or caused by some congenital problem, such as a wedge vertebra, hemivertebra, or failure of vertebral segmentation. In other words, there is a structural change in the bone, and normal flexibility of the spine is lost.11
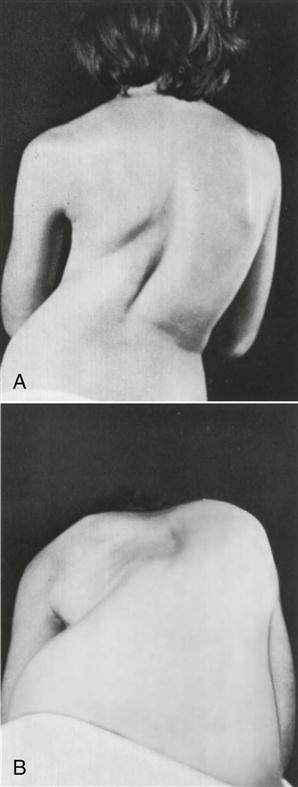
A, Postural deformity caused by idiopathic thoracolumbar scoliosis. B, Asymmetry of posterior thorax accentuated with patient flexed. Note “hump” on the right and “hollow” on the left. (From Gartland JJ: Fundamentals of orthopedics, Philadelphia, 1979, WB Saunders, p. 341.)
A number of curve patterns may be present with scoliosis (Figure 8-13).11 The curve patterns are designated according to the level of the apex of the curve (Table 8-3). A right thoracic curve has a convexity toward the right, and the apex of the curve is in the thoracic spine. With a cervical scoliosis, or torticollis, the apex is between C1 and C6. For a cervicothoracic curve, the apex is at C7 or T1. For a thoracic curve, the apex is between T2 and T11. The thoracolumbar curve has its apex at T12 or L1. The lumbar curve has an apex between L2 and L4, and a lumbosacral scoliosis has an apex at L5 or S1. The involvement of the thoracic spine results in a very poor cosmetic appearance or greater visual defect as a result of deformation of the ribs along with the spine. The deformity can vary from a mild rib hump to a severe rotation of the vertebrae, causing a rib deformity called a razorback spine.
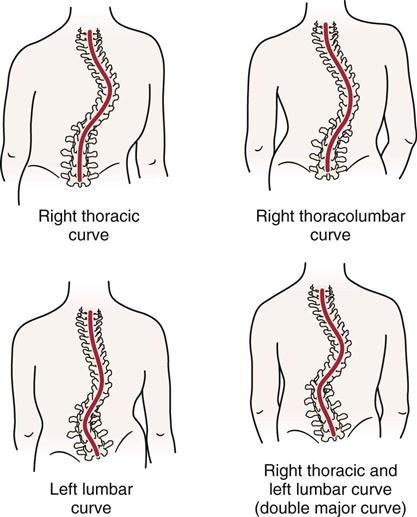
TABLE 8-3
Curve Patterns and Prognosis in Idiopathic Scoliosis
| CURVE PATTERN | |||||
| Primary Lumbar | Thoracolumbar | Combined Thoracic and Lumbar | Primary Thoracic | Cervicothoracic | |
| Incidence (%) | 23.6 | 16 | 37 | 22.1 | 31.3 |
| Average age curve noted (year) | 13.25 | 14 | 12.3 | 11.1 | 15.3 |
| Average age curve stabilized (year) | 14.5 | 16 | 15.5 | 16.1 | 16.3 |
| Extent of curve | T11–L3 | T6 or T7–L1 or L1, L2 | Thoracic, T6–T10 Lumbar, T11–L4 | T6–T11 | C7 or T1–T4 or T5 |
| Apex of curve | L1 or L2 | T11 or L2 | Thoracic, T7 or T8 Lumbar, L2 | T8 or T9 (rotation extreme, convexity usually to right) | T3 |
| Average angular value at maturity (degrees) | |||||
| Standing | 36.8 | 42.7 | Thoracic, 51.9; Lumbar, 41.4 | 81.4 | 34.6 |
| Supine | 29.1 | 35 | Thoracic, 41.4; Lumbar, 37.7 | 73.8 | 32.2 |
| Prognosis | Most benign and least deforming of all idiopathic curves | Not severely deforming Intermediate between thoracic and lumbar curves | Good Body usually well aligned, curves even if severe tend to compensate each other High percentage of very severe scoliosis if onset before age of 10 years | Worst Progresses more rapidly, becomes more severe, and produces greater clinical deformity than any other pattern Five years of active growth during which curve could increase | Deformity unsightly Poorly disguised because of high shoulder, elevated scapula, and deformed thoracic cage |
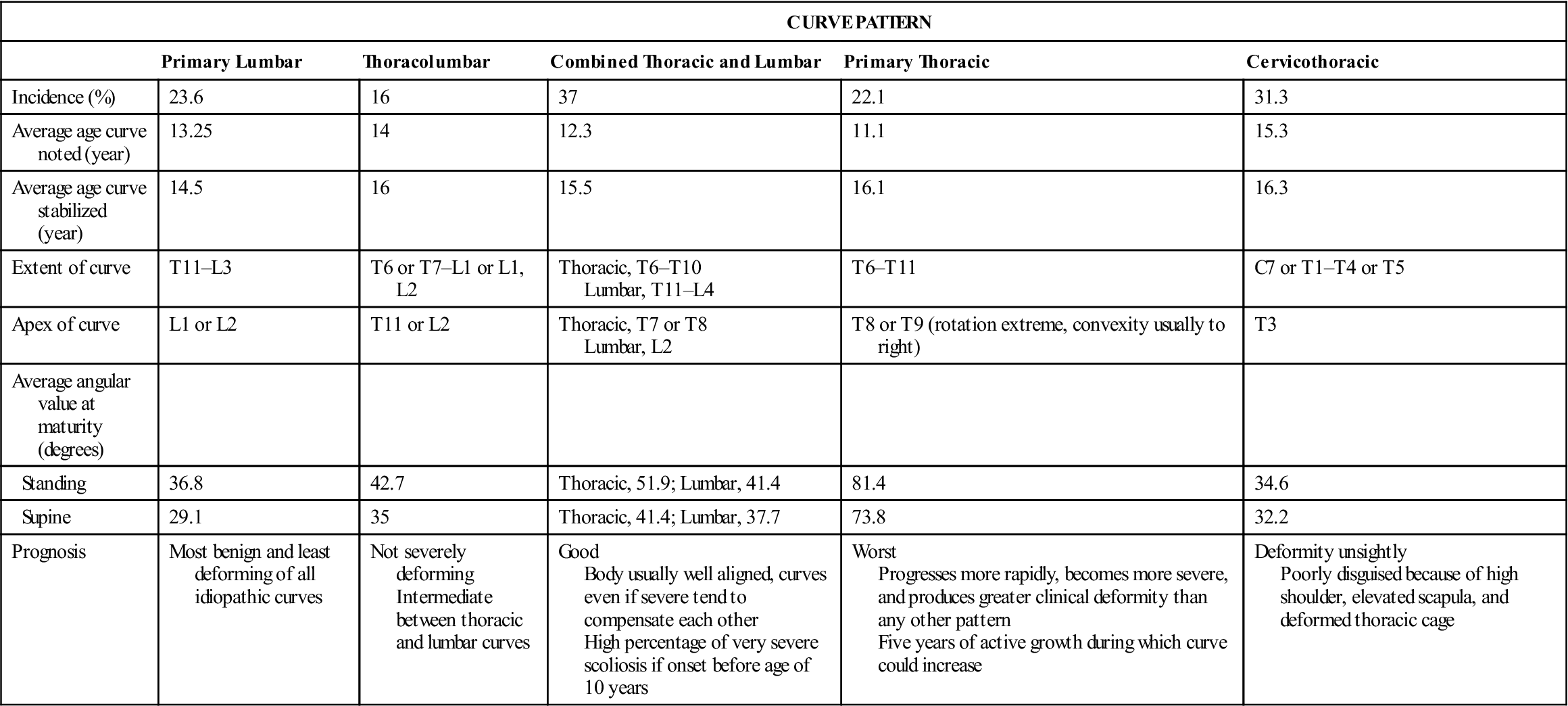
Adapted from Ponseti IV, Friedman B: Prognosis in idiopathic scoliosis. J Bone Joint Surg Am 32:382, 1950.
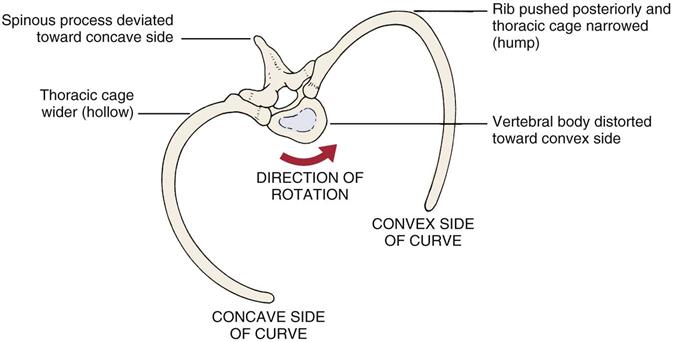
With a structural scoliosis, the vertebral bodies rotate to the convexity of the curve and become distorted.12 If the thoracic spine is involved, this rotation causes the ribs on the convex side of the curve to push posteriorly, causing a rib “hump” and narrowing the thoracic cage on the convex side. As the vertebral body rotates to the convex side of the curve, the spinous process deviates toward the concave side. The ribs on the concave side move anteriorly, causing a “hollow” and a widening of the thoracic cage on the concave side (Figure 8-14). Lateral deviation may be more evident if the examiner uses a plumb bob (plumbline) from the C7 spinous process or external occipital protuberance (Figure 8-15).
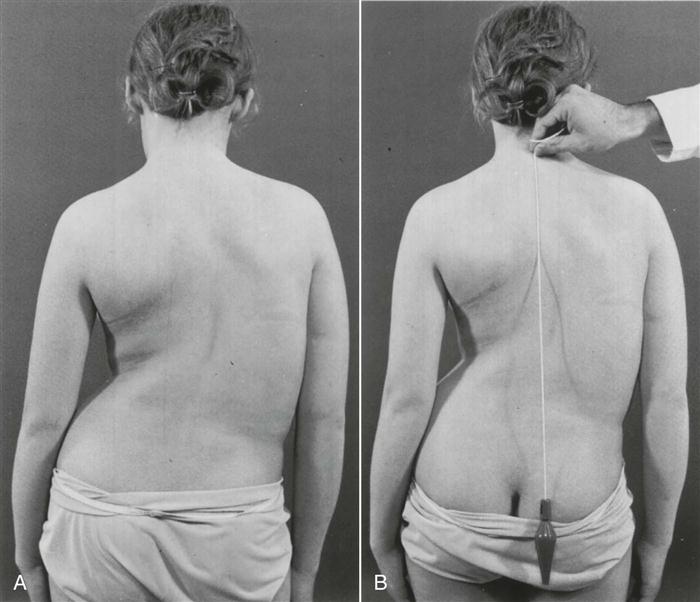
A, The left shoulder is lower, and the right scapula is more prominent. Note the decreased distance between the right arm and the thorax with the shift of the thorax to the right. The left iliac crest appears higher, but this results from the shift of the thorax with fullness on the right and elimination of the waistline; the “high” hip is only apparent, not real. B, Plumbline dropped from the prominent vertebra of C7 (vertebra prominens) measures the decompensation of the thorax over the pelvis. The distance from the vertical plumbline to the gluteal cleft is measured in centimeters and is recorded along with the direction of deviation. If there is a cervical or cervicothoracic curve, the plumb should fall from the occipital protuberance (inion). (From Moe JH, Winter RB, Bradford DS, et al: Scoliosis and other spinal deformities, Philadelphia, 1978, WB Saunders, p. 14.)
The examiner should note whether the ribs are symmetric and whether the rib contours are normal and equal on the two sides. In idiopathic scoliosis, the rib contours are not normal, and there is asymmetry of the ribs. Muscle spasm resulting from injury may also be evident. The bony and soft-tissue contours should be observed for equality on both sides or for any noticeable difference.
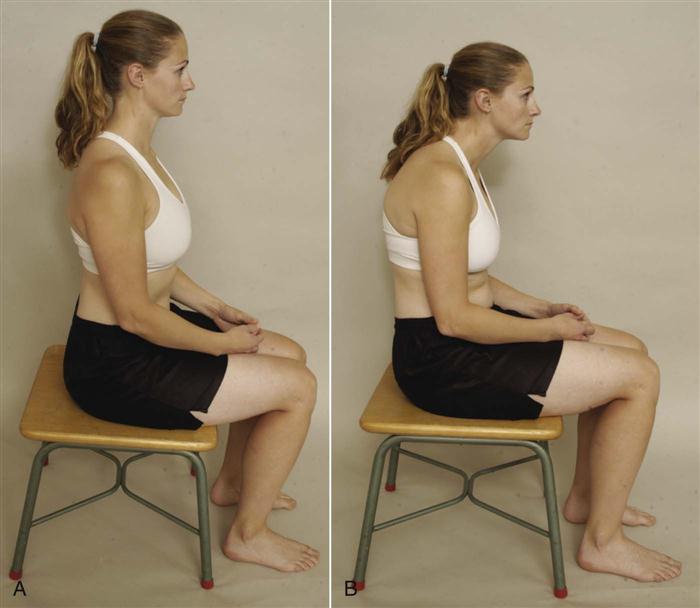
The examiner should note whether the patient sits up properly with the normal spinal curves present (Figure 8-16, A); whether the tip of the ear, tip of the acromion process, and high point of the iliac crest are in a straight line as they should be; and whether the patient sits in a slumped position (i.e., sag sitting, as in Figure 8-16, B).
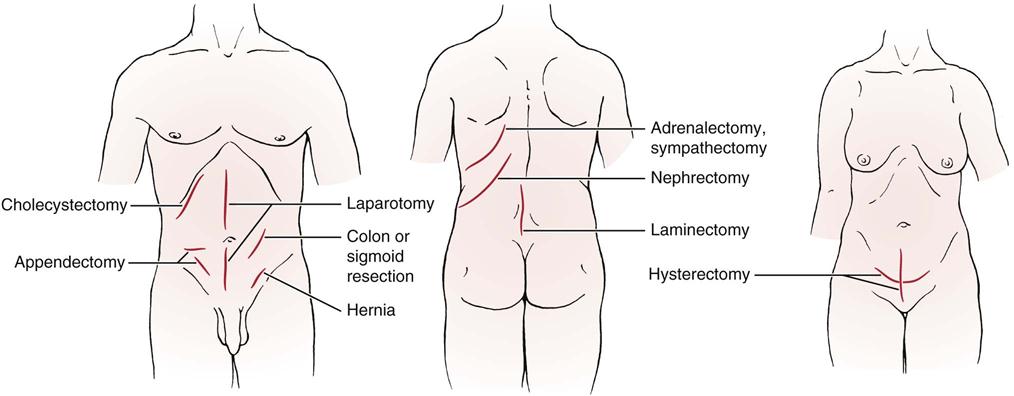
The skin should be observed for any abnormality or scars (Figure 8-17). If there are scars, are they a result of surgery or trauma? Are they new or old scars? If from surgery, what was the purpose of the surgery?
Breathing
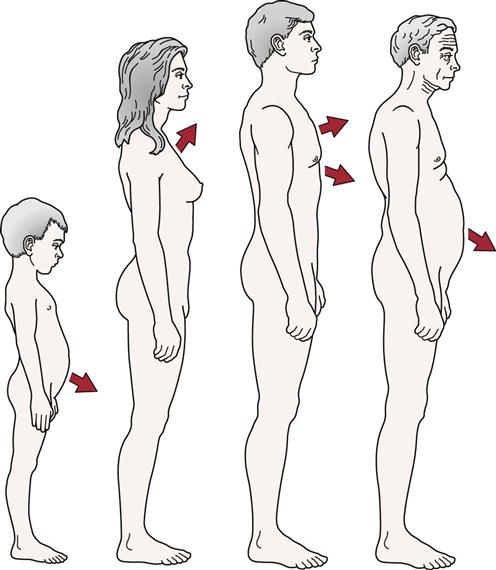
As part of the observation, the examiner should note the patient’s breathing pattern. Children tend to breathe abdominally, whereas women tend to do upper thoracic breathing. Men tend to be upper and lower thoracic breathers. In the aged, breathing tends to be in the lower thoracic and abdominal regions (Figure 8-18). The examiner should note the quality of the respiratory movements as well as the rate, rhythm, and effort required to inhale and exhale. The examiner should also note whether the patient is using the primary muscles of respiration and/or the accessory muscles of respiration, because this will help indicate the ease of the patient’s breathing (Table 8-4). In addition, the presence of any coughing or noisy or abnormal breathing patterns should be noted. Because the chest wall movement that occurs during breathing displaces the pleural surfaces, thoracic muscles, nerve, and ribs, pain is accentuated by breathing and coughing if any one of these structures is injured.
TABLE 8-4
| Primary | Secondary | |
| Inspiration | Diaphragm Levator costorum External intercostals Internal intercostals (anterior) | Scaleni Sternocleidomastoid Trapezius Serratus anterior and posterior Pectoralis major Pectoralis minor Subclavius |
| Both | Latissimus dorsi | |
| Expiration | Internal obliques External obliques Rectus abdominus Transverse abdominus Transversus thoracis Transverse intercostals Internal intercostals (posterior) | Serratus posterior inferior Quadratus lumborum Iliocostalis lumborum |
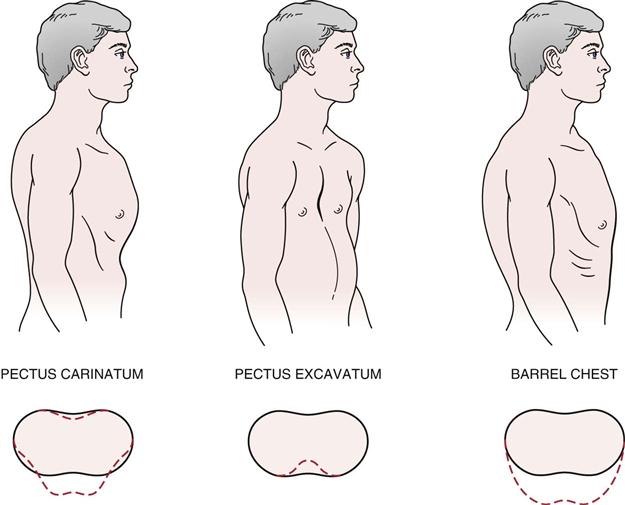
Chest Deformities
In addition to rib movements during breathing, the examiner should note the presence of any chest deformities. The more common deformities are shown in Figure 8-19 and are listed below:
2. The funnel chest (pectus excavatum) is a congenital deformity that results from the sternum’s being pushed posteriorly by an overgrowth of the ribs.13 The anteroposterior dimension of the chest is decreased, and the heart may be displaced. On inspiration, this deformity causes a depression of the sternum that affects respiration and may result in kyphosis.
Examination
Although the assessment is primarily of the thorax and thoracic spine, if the history, observation, or examination indicates symptoms into or from the neck, upper limb, or lumbar spine and lower limb, these structures must be examined as well using an upper or lower scanning examination. If any signs or symptoms are elicited in the scanning exam, more detailed examination of the cervical or lumbar spine may be performed. Therefore, the examination of the thoracic spine may be an extensive one. Unless there is a history of specific trauma or injury to the thoracic spine or ribs, the examiner must be prepared to assess more than that area alone. If a problem is suspected above the thoracic spine, the scanning examination of the cervical spine and upper limb (as described in Chapter 3) should be performed. If a problem is suspected below the thoracic spine, the scanning examination of the lumbar spine and lower limb (as described in Chapter 9) should be performed. Only examination of the thoracic spine is described here.
Active Movements
The active movements of the thoracic spine are usually done with the patient standing. Movement in the thoracic spine is limited by the rib cage and the long spinous processes of the thoracic spine. When assessing the thoracic spine, the examiner should be sure to note whether the movement occurs in the spine or in the hips. A patient can touch the toes with a completely rigid spine if there is sufficient range of motion (ROM) in the hip joints. Likewise, tight hamstrings may alter the results. The movements may be done with the patient sitting, in which case the effect of hip movement is eliminated or decreased. Similarly, shoulder motion may be restricted if the upper thoracic segments or ribs are hypomobile.14 As with any examination, the most painful movements are done last. The active movements to be carried out in the thoracic spine are shown in Figure 8-20.
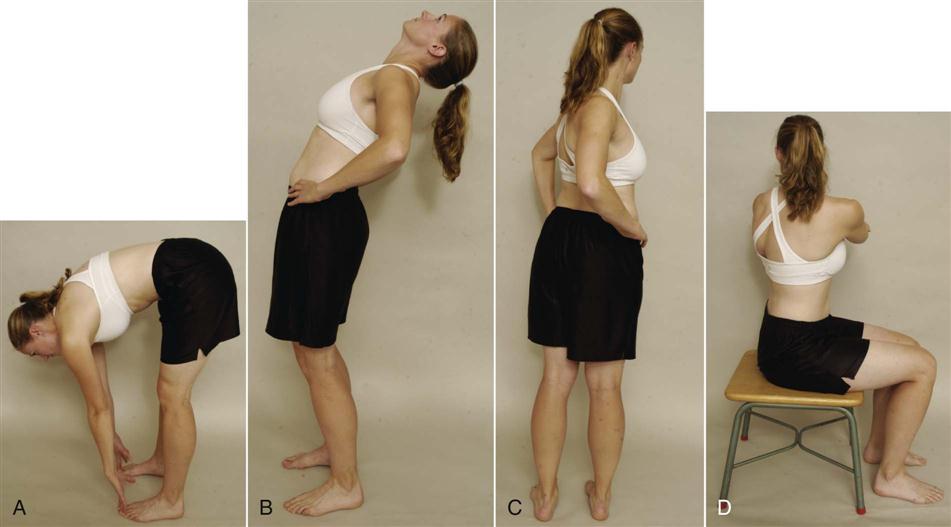
 Figure 8-20 Active movements.
Figure 8-20 Active movements.A, Forward flexion. B, Extension. C, Rotation (standing). D, Rotation (sitting).
Forward Flexion
The normal ROM of forward flexion (forward bending) in the thoracic spine is 20° to 45° (Figure 8-21). Because the ROM at each vertebra is difficult to measure, the examiner can use a tape measure to derive an indication of overall movement (Figure 8-22). The examiner first measures the length of the spine from the C7 spinous process to the T12 spinous process with the patient in the normal standing posture. The patient is then asked to bend forward and the spine is again measured. A 2.7-cm (1.1-inch) difference in tape measure length is considered normal.
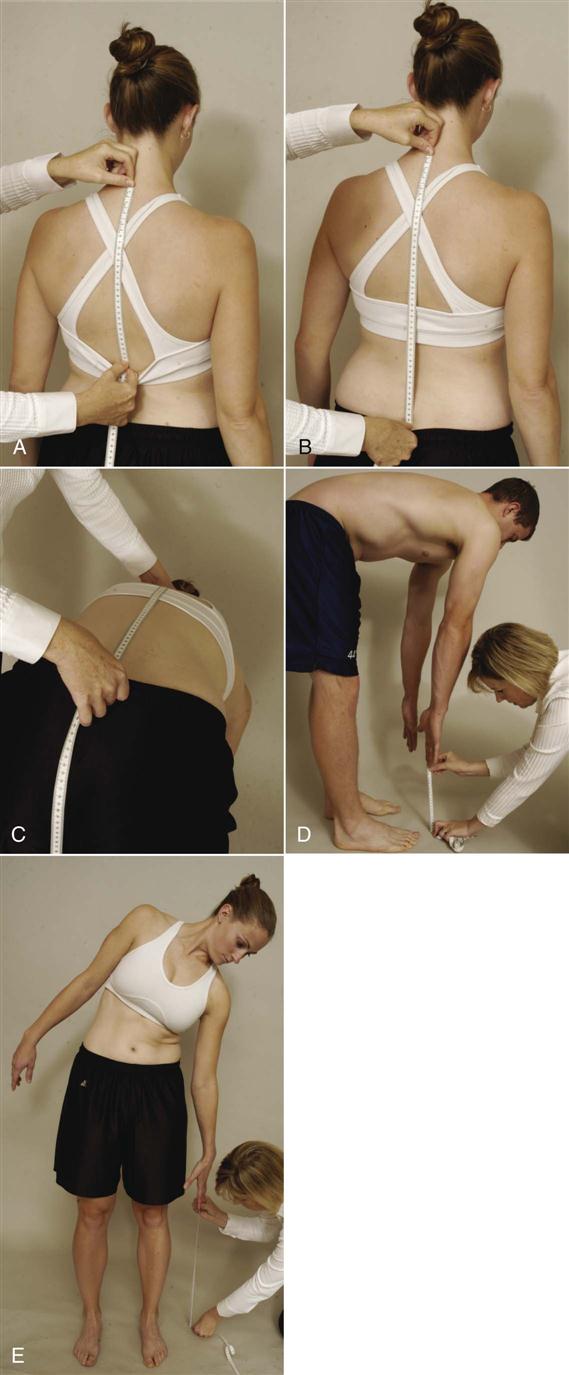
A, Positioning of tape measure for determining flexion and extension in the thoracic spine. B, Positioning of tape measure for determining flexion or extension in the thoracic and lumbar spines combined. C, Forward flexion measurement of thoracic and lumbar spines. D, Forward flexion measurement of thoracic and lumbar spines and hips (fingertips to floor). E, Side flexion measurement (fingertips to floor).
If the examiner wishes, the spine may be measured from the C7 to S1 spinous process with the patient in the normal standing position. The patient is then asked to bend forward, and the spine is again measured. A 10-cm (4-inch) difference in tape measure length is considered normal. In this case, the examiner is measuring movement in the lumbar spine as well as in the thoracic spine; most movement, approximately 7.5 cm (3 inches), occurs between T12 and S1.
A third method of measuring spinal flexion is to ask the patient to bend forward and try to touch the toes while keeping the knees straight. The examiner then measures from the fingertips to the floor and records the distance. The examiner must keep in mind that with this method, in addition to the thoracic spine movement, the movement may also occur in the lumbar spine and hips; in fact, movement could occur totally in the hips.
Each of these methods is indirect. To measure the ROM at each vertebral segment, a series of radiographs would be necessary. The examiner can decide which method to use. It is of primary importance, however, to note on the patient’s chart how the measuring was done and which reference points were used.
While the patient is flexed forward, the examiner can observe the spine from the “skyline” view (Figure 8-23). With nonstructural scoliosis, the scoliotic curve disappears on forward flexion; with structural scoliosis, it remains. With the skyline view, the examiner is looking for a hump on one side (convex side of curve) and a hollow (concave side of curve) on the other. This “hump and hollow” sequence is caused by vertebral rotation in idiopathic scoliosis, which pushes the ribs and muscles out on one side and causes the paravertebral valley on the opposite side. The vertebral rotation is most evident in the flexed position.
When the patient flexes forward, the thoracic spine should curve forward in a smooth, even manner with no rotation or side flexion (Figure 8-24). The examiner should look for any apparent tightness or sharp angulation, such as a gibbus, when the movement is performed. If the patient has an excessive kyphosis to begin with, very little forward flexion movement occurs in the thoracic spine. McKenzie7 advocates doing flexion while sitting to decrease pelvic and hip movements. The patient then slouches forward flexing the thoracic spine. The patient can put the hands around the neck to apply overpressure at the end of flexion. If symptoms arise from forward flexion on the spine with the neck flexed by the hands, the examiner should repeat the movement with the neck slightly extended and the hands removed. This will help differentiate between cervical and thoracic pain.
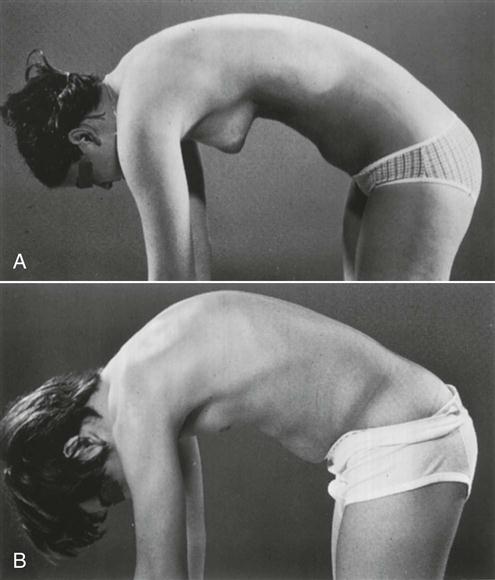
A, Normal thoracic roundness is demonstrated with a gentle curve to the whole spine. B, An area of increased bending is seen in the thoracic spine, indicating structural changes—Scheuermann disease, in this example. (From Moe JH, Winter RB, Bradford DS, et al: Scoliosis and other spinal deformities, Philadelphia, 1978, WB Saunders, p. 18.)
Extension
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree