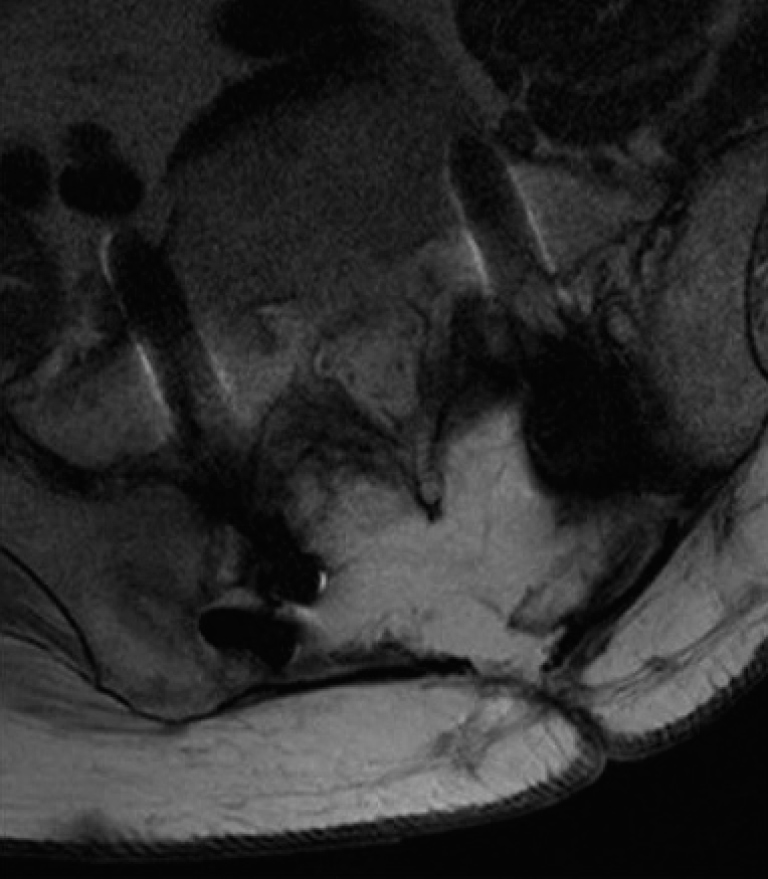
9 Operative treatment of metastatic spine disease is palliative and targeted to improve health-related quality of life (HRQOL). Surgical treatment is usually reserved for patients with metastatic spinal cord compression or spinal instability. The primary goals of surgery are to decompress neurologic elements to prevent, stabilize, or improve neurologic deficit, provide a safe margin for radiotherapy, stabilize the spinal column, and achieve local disease control. Despite these relatively clear indications, surgeons must not lose sight of the bigger picture: although palliative spine surgery can improve HRQOL,1 complications will lengthen the hospitalization2 and negatively impact the quality of life. Additionally, surgical complications may delay or prevent adjuvant radiation and chemotherapy for the patient’s primary disease. This chapter discusses specific complications and their avoidance. For surgical treatment of metastatic spine disease to be successful, a patient must be able to make a meaningful recovery. Accurately assessing the extent of disease and the medical risks of the procedure are important for prognostication and surgical decision making. In most cases, surgery is considered semi-urgent and a thorough but expedited workup is appropriate. Even in emergent cases of catastrophic neurologic deterioration, medical and oncological consultation should be obtained. Surgical intervention in metastatic spine disease is intended to protect or restore neurologic function; thus, a surgical candidate must meet functional criteria to be considered for surgery. Poor performance status may be a contraindication for surgery. Exceptions to this include patients with pathological fractures that have a poor performance status due to pain-related immobility, or patients with rapid neurologic deterioration in the previous 24 to 48 hours. Although they have been refined, the original Patchell criteria are an appropriate starting point. Patients should have a life expectancy of at least 3 months but preferably 6 months to achieve a measurably enhanced quality of life following the procedure,1 although this may be shortening with the advent of percutaneous and other minimally invasive procedures. Widely metastatic disease may be a contraindication for surgery. Thus, oncological workup may include needle biopsy of the spine or other accessible lesion to obtain pathological diagnosis of the primary tumor. Metastatic workup including chest, abdomen, and pelvis computed tomography (CT); bone scan; pan-spine magnetic resonance imaging (MRI) and brain MRI; and positron emission tomography can be considered to determine the extent of disease. Radiation-responsive tumors require particular thoughtfulness related to stability and the cause of neurology. A patient may be better served without a surgical procedure; however, cord compression involving bone fragments due to a pathological burst fracture may still require operative intervention, even in a radio-sensitive tumor. The surgical procedure must be well planned. In some cases, the burden of disease in the spinal column makes surgical resection or reconstruction technically impossible. The surgeon must be able to achieve a worthwhile decompression and restore biomechanical stability to the spinal column. If either of these goals cannot be met, the patient may not be a surgical candidate. If a patient is deemed an oncological and functional candidate for surgery, a patient must be able to tolerate the anticipated procedure. For a standard extracavitary approach, vertebrectomy, and stabilization, it is reasonable to estimate a 2-L blood loss and a 6-hour operative time, with the patient in the prone position. These estimates may enable the medical and anesthesia physicians to determine the surgical risk. Patients without a high probability of surviving the procedure should not undergo it, even in the face of imminent paralysis. Appropriate patient selection and anticipation of adverse events based on comorbid medical conditions is the most important component of complication avoidance. Detailed discussion of appropriate patient surgical selection is discussed in Chapter 1. Once it has been determined that a patient is a candidate for surgery, a thoughtful approach should be employed, even in urgent or emergent cases, to minimize oncology-specific risk factors. In most cases, the surgical target has been chosen because of potential or actual neurologic decline due to compression of instability or pain related to instability. The tumor at the surgical target itself may warrant preoperative intervention to decrease the surgical risk as discussed in the embolization section below. Additionally, the overall disease burden and the effect of previous radiation or chemotherapy that the patient may have already have undergone can greatly affect surgical outcome. Thus, this section discusses the hematologic and neurotoxic considerations that should be carefully addressed in the preoperative period. Although sudden catastrophic hemorrhage is rare in metastatic spine tumor surgery, a number of factors lead to high blood loss. Thus, surgical planning should include strategies to correct hematologic abnormalities, minimize blood loss, and manage intraoperative hemorrhage.3 The oncology patient’s natural hemostatic response may be disrupted by the primary disease, especially in cases of hematologic malignancies, those involving the liver, or following certain nonsurgical therapies resulting in bone marrow suppression. Preoperatively, a complete coagulation panel is imperative, with factor correction as necessary. Additionally, large-bore intravenous access or central lines should be considered preoperatively. Fluid and blood can be infused through warmers, which in conjunction with body warmers may reduce intraoperative coagulopathies. Unfortunately, due to the risk of metastasizing tumor from the surgical site, blood salvage equipment should not be used. Intraoperatively, attention should be paid to nontumoral blood loss and tumoral bleeding. In addition to standard soft tissue and bony bleeding, epidural venous bleeding can be extensive. Patient positioning can minimize intraabdominal pressure, and the use of multiple hemostatic agents is helpful. Postoperatively, hematologic parameters should be monitored, as fluid shifts and blood loss via drains may be significant. Conversely, cancer patients are often hyper-coagulable, leading to disseminated intravascular coagulation, deep venous thromboses (DVTs), and pulmonary emboli (PEs). Intraoperatively, sequential compression devices (SCDs) are used during these often long procedures with the patient in the prone position. Postoperatively, consideration should be given to early mobilization, the continued use of SCDs, and the use of anticoagulants such as subcutaneous heparin. This is especially important in patients who have suffered neurologic deterioration and recent loss of mobility. A low threshold for lower extremity Doppler ultrasound to investigate possible DVTs and aggressive treatment with intravascular filter placement and anticoagulation are indicated. Similarly, surgeons should have a low threshold for investigation of suspected PEs and should aggressively treat them upon diagnosis. Tumors, especially vascular lesions, are often difficult to cauterize and do not stop bleeding until they are completely resected. Certain lesions may benefit from preoperative embolization to decrease intraoperative hemorrhage, not only to reduce the physiological stress on the patient by decreasing blood loss,4 but also to make it easier for the surgeon to visualize and complete the procedure efficiently and safely. Specifically, renal cell carcinoma, follicular thyroid carcinoma, neuroendocrine tumors, and tumors of unknown histology with suggestions of hypervascularity on imaging studies should be considered for embolization.3 In other cases, if a vascular lesion is suspected and embolization is not possible, en bloc resection can be attempted to avoid violating the tumor (discussed in Chapter 4). An additional advantage to embolization is the ability to localize major spinal segmental feeding arteries such as the artery of Adamkiewicz. Rhizotomy or nerve root sacrifice at this level can lead to anterior spinal artery ischemia and spinal cord infarction and should be avoided if possible. Protection of both the central and peripheral nervous systems is imperative in metastatic spine tumor patients. Most patients are selected for surgical intervention due to spinal cord compression or instability resulting in neurologic compromise. Thus, care must be taken not to worsen spinal cord compression during positioning. Documenting a preoperative examination, obtaining preoperative electrophysiological monitoring baselines, and performing awake or fiberoptic intubation in cervical cases should be considered. Careful positioning, including log-roll or Jackson table sandwich techniques and pinions are especially important to protect the spinal cord. Postposition electrophysiological monitoring and wake-up tests to assess neurologic status and pre-draping imaging studies to assess preopeative alignment are helpful. Should any study demonstrate decreased neurologic function, the surgeon must consider reversing the positioning, waking the patient, and employing a set spinal cord injury protocol as discussed below (see Neurologic Injury). Oncology patients also require special attention to their peripheral nervous system. Many patients have been exposed to neurotoxic chemotherapeutic agents prior to undergoing surgical intervention. These agents may increase their risk of position-dependent injuries such as ulnar neuropathies; thus, special attention should be paid to table padding and straps. Finally, the operating room staff should note and protect any chemotherapeutic ports the patient may have in place for systemic treatment. The basic tenets of spine surgery are the key to a successful procedure in the oncology patient. Even in emergent situations, the surgeon must thoroughly understand the regional anatomy, obtain adequate exposure, and employ gentle tissue handling techniques. Most importantly, pathological changes in anatomy must be understood and regional structures of vital importance must be identified before proceeding. It is wise to work from normal to pathological anatomy to maintain orientation. Tumors are notoriously unpredictable in their behavior: ensuring that all structures are well visualized and protected in a systematic fashion allows a surgeon to react confidently in the face of unexpected complications such as sudden hemorrhage. Finally, respecting natural tissue planes, maintaining reasonable hemostasis, and ensuring that soft tissue remains vital and perfused will lessen the physiological stress of surgery and improve healing in patients who may be weakened by their primary disease and treatments. A thoughtful and deliberate approach to these technically challenging surgeries and complex patients will improve the chance of success. One of the major goals of spine surgery for metastasis is the prevention or potential reversal of neurologic deficit due to spinal cord compression. However, one of the most feared surgical complications is spinal cord injury. Preoperative, intraoperative, and postoperative practices may reduce the risk of neurologic deterioration. Additionally, appropriate intraoperative and postoperative response to suspected spinal cord injury may minimize or reverse potential deficits. Preoperatively, unless medically contraindicated, patients with new neurologic deficit who are undergoing preoperative medical and oncological workup should receive high-dose steroids to decrease spinal cord edema.5 Commonly, this takes the form of a loading dose and subsequent maintenance doses. The standard is now 10 mg of dexamethasone bolus and 4 to 6 mg every 6 hours is a reasonable starting point, although this standard remains controversial. Ultimately, following surgery, the drug is tapered down to oncologically useful doses. Intraoperatively, for cases involving spinal cord decompression, we commonly use somatosensory evoked potential (SSEP) and motor evoked potential (MEP) monitoring, and free-running electromyogram (EMG) can be used in cases of root compression. Prepositioning neurophysiological baselines should be obtained and maintained throughout the procedure. If signals are poor, consideration can be given to a postpositioning wake-up test. The surgical, anesthesia, and neuromonitoring teams should be well versed in their response to a decreased monitoring response.6 The surgical team should consider whether new or increased mechanical cord compression has occurred, such as hematoma, instrumentation malposition, or deformity correction, and consider decompressing or reversing it if possible. The anesthesia team should ensure that the patient is normothermic and hemodynamically resuscitated, and that there were no changes to anesthetic/medication delivery, and should consider raising mean arterial pressure to 90 mm Hg. The monitoring team should check its equipment and leads to ensure there is no technical problem with the device. Steroid bolus can be considered if not already given. Postoperatively, at the discretion of the surgical team, blood pressure may be artificially elevated and steroids continued in an effort to increase cord perfusion and decrease edema. This is especially helpful in patients with new deficits, or in instances where it is suspected that the vascular perfusion pattern of the spinal cord is altered, such as multiple nerve root and radicular artery sacrifices. Epidural tumor surgery may be complicated by injury to an adjacent structure. Surgical planning to minimize such transgressions includes understanding anatomy distortion through pathological processes, protecting adjacent structures (for example, placing ureteral stents or employing preoperative endovascular vessel sacrifice), and minimizing multiple-compartment surgeries (for instance, using an extra-cavitary approach to thoracic spinal lesions while avoiding the chest cavity). A plan for intraoperative iatrogenic adjacent organ injury should be considered preoperatively. Cerebrospinal fluid (CSF) extravagation may complicate wound healing and result in intradural tumor seeding (Fig. 9.1). Although best avoided, if dural tears occur in oncological cases, they should be aggressively treated in a similar fashion to those occurring in other spine surgeries.7 Dural rents should be repaired primarily or using a patch graft if the rent is too large for primary closure. Similarly, if rhizotomy is performed, the root should be tied or clipped securely to prevent CSF egress. Oversewing a muscle pledget or using a dural sealant can be considered. When a durotomy is irreparable, the use of a lumbar drain for several days will decrease the hydrostatic pressure on the repair. Additionally, CSF absorption may be compromised in irradiated tissue, thus even low-volume leaks are prone to wound healing problems.3 Fig. 9.1 Patient with inadequately repaired primary dural tear and improperly closed fascia who has developed a pseudomeningocele immediately prior to his first wound dehiscence. The patient required three surgical revisions including vascularized rotational flap, resulting in 4-month hospitalization. Two years later he has a palpable but stable pseudomeningocele and continued low-pressure headaches.
Surgical Complications and Their Avoidance
 Introduction
Introduction
 Patient Selection
Patient Selection
 Preoperative Evaluation and Preparation
Preoperative Evaluation and Preparation
Hemorrhage
Coagulation Abnormalities
Preoperative Embolization
Operative Positioning
 Intraoperative Complications: Prevention and Minimization
Intraoperative Complications: Prevention and Minimization
Neurologic Injury
Adjacent Organ Injury
Spinal Fluid Leak
Surgical Complications and Their Avoidance
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree