Surgical Approaches to Patellar Malalignment
Donald C. Fithian
Robert A. Teitge
Samuel Ward
Robert Afra
BACKGROUND
The patellofemoral joint (PFJ) is a unique articulation with a complex architecture. Its motion differs from that of most other joints, in that, it is mostly comprised of sliding rather than rolling. This places unique challenges on the articular cartilage. The most common disorders of the PFJ are thought to occur as a result of alterations in the mechanics of this joint, leading to cartilage overload or gross instability.
It is worth pointing out that the objective of “offloading the patella” is very difficult to achieve by surgical means. The patella exists to improve the leverage of the knee extensor system, and it is necessary that the PFJ support compressive loads in order for the knee to function properly. Although it is true that anteriorization of the tibial tuberosity (TT), as described by Maquet (1), can reduce PFJ force while maintaining quadriceps-generated extension torque, the practical limitations of this procedure are well known. Surgical realignment in most cases, then, is directed at redistributing forces so that all joint surfaces and soft tissues in the knee wear out at a similar acceptable rate.
DEFINITIONS OF ALIGNMENT AND MALALIGNMENT
There are two common uses for the term “alignment” as it relates to the patellofemoral articulation: (1) position of the patella in the femoral groove, and (2) position of the patella and groove between the body and the foot. It is a common oversimplification to consider alignment as referring only to the position of the patella on the femoral trochlea. Although alignment of the patella on the trochlea (e.g., medial/lateral shift, alta/infera, and tilt) is important, this assessment should not distract us from the equally important consideration of how the position of the knee in space affects the location and magnitude of forces within the PFJ. Thorough workup requires evaluation of knee extensor alignment from both perspectives.
The concept of malalignment is based on several assumptions:
1. Mechanical systems have a theoretical optimal alignment, in which forces are well balanced, and no part of the mechanism wears out before any other part.
2. Forces that are applied off-center can be magnified many times by the moments they generate.
3. Any variation from optimal skeletal alignment may increase the force vectors acting on the PFJ, causing either ligament failure with subsequent subluxation or dislocation or cartilage failures as in chondromalacia or arthrosis.
Malalignment distributes abnormal stresses to both the ligaments and the joint surfaces in the misaligned limb. Ligament overload and subsequent failure may occur with a single traumatic episode or with chronic repetitive episodes of minor trauma. Skeletal malalignment may cause chondromalacia patella and subsequently arthrosis by generating forces on the PFJ that exceed the load-carrying capacity of the cartilage. Even if forces are not excessive, reduction in contact surface area caused by a small patella, patella alta, or patellar subluxation can increase the force per unit area (stress) beyond the load capacity of the articular cartilage, leading to cartilage failure (arthrosis). Similarly, excessive or abnormal gliding of the joint can increase shear stresses beyond the capacity of the articular cartilage, leading to cartilage failure. Anterior knee pain in the setting of a malaligned lower extremity may be the result of abnormal compression, tension or shear in the capsule, ligaments, synovium, or subchondral bone.
EFFECT OF ROTATIONAL MALALIGNMENT ON PFJ POSITION IN SPACE
Maximum gait efficiency with minimal stress is affected by normal limb alignment. Any deviation from normal limb alignment in any plane can lead to pain, much like when twisting a knee. These include femoral anteversion or retroversion, excess internal or external tibial torsion (ETT),
genu valgum or varum, hyperpronation and Achilles contracture. Twisting of the knee away from the limb mechanical axis (inward or outward) will change the direction and magnitude of the patellofemoral compression force, and will also add a side-directed vector to the patella. This vector is resisted by the soft tissues (both medial and lateral patellofemoral ligaments as well as accessory capsular ligaments). It is also resisted by the femoral trochlea, to a degree determined by its depth, length, and shape. The distribution of these constraining forces between retinaculum and trochlea is determined primarily by the shape of the trochlea: the greater its depth and length, and the steeper its medial and lateral walls (i.e., sulcus angle), the lower the resulting force in the soft tissues.
genu valgum or varum, hyperpronation and Achilles contracture. Twisting of the knee away from the limb mechanical axis (inward or outward) will change the direction and magnitude of the patellofemoral compression force, and will also add a side-directed vector to the patella. This vector is resisted by the soft tissues (both medial and lateral patellofemoral ligaments as well as accessory capsular ligaments). It is also resisted by the femoral trochlea, to a degree determined by its depth, length, and shape. The distribution of these constraining forces between retinaculum and trochlea is determined primarily by the shape of the trochlea: the greater its depth and length, and the steeper its medial and lateral walls (i.e., sulcus angle), the lower the resulting force in the soft tissues.
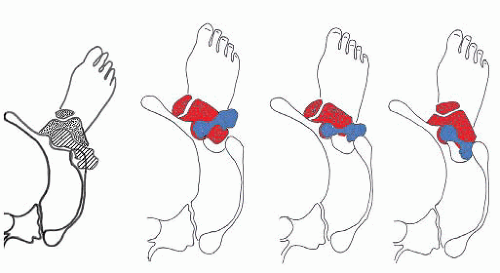
The foot progression angle (FPA) is generally defined as the angle between the long axis of the foot and the direction of body progression. It varies from 10° to 20° (2). It has been shown that despite congenital or acquired (after fracture) torsional deformities in the lower limb bones, the FPA remains unchanged (3, 4 and 5). It is hypothesized that the hip musculature plays a role in accommodating these deformities during gait. For example, in the presence of an internal femoral or external tibial rotational deformity with a normal FPA (Fig. 60.1A, B), the knee joint axis rotates inward and a side force vector is produced, acting on the patella so that both the strain on the medial patellofemoral ligament (MPFL) and compression on the lateral patellofemoral facet are increased. It is not well understood how the body accommodates rotational deformities during gait. Importantly, the compensatory options are limited and none of them is optimal from a mechanical point of view. For example, in the setting of pure femoral anteversion (Fig. 60.1C, D), if the body seeks to restore normal femoroacetabular alignment, the knee (and trochlea) will point medially across the midline. In this case, we see either an in-toeing gait and/or a compensatory foot pronation in order to achieve a normal FPA. If the body seeks the normal sagittal alignment of the knee joint and foot, the greater trochanter will be posteriorly positioned, which places the hip abductors at a mechanical disadvantage. In this case, we may see medial collapse (adduction and internal rotation) of the hip during weight-bearing.
ASSOCIATION BETWEEN SKELETAL MALALIGNMENT AND PFJ PATHOLOGY
In the frontal plane, malalignment has been shown to influence the progression of PFJ arthritis (6, 7). Varus alignment increases the likelihood of medial patellofemoral arthrosis progression, whereas valgus alignment increases the likelihood of lateral patellofemoral arthrosis progression. Fujikawa et al. (8) in a cadaveric study found a marked alteration of patellar and femoral contact areas with the introduction of increased varus alignment produced by a varus osteotomy.
Lerat et al. (9) noted a statistically significant correlation between increased femoral internal torsion (i.e., femoral anteversion) and both patellar chondrosis and instability. Janssen (10) also found that patients with a history of patellar dislocation had increased odds of internal femoral torsion compared with control subjects. They speculated that internal femoral torsion was responsible for the development of dysplasia of the trochlea and of the patella. Takai et al. (11) measured femoral and tibial torsion in patients with patellofemoral, medial, and lateral unicompartmental osteoarthrosis. They noted that patellofemoral osteoarthrosis was associated with increased femoral torsion (23° vs. 9° in controls), and concluded that excessive femoral torsion contributed to patellofemoral wear in these patients.
Turner (12) studied the association of tibial torsion and knee joint pathology. He observed that patients with patellofemoral instability had greater than normal ETT (25° vs. 19° in controls). Eckhoff et al. (13) found that the tibia in the extended knee was 6° more externally rotated than normal controls in a group of patients with anterior knee pain. Whether this represented an abnormal skeletal torsion or an abnormal rotation of the tibia on the femur due to knee joint soft tissue laxity or abnormal muscle pull is unknown.
EFFECTS OF ROTATIONAL MALALIGNMENT ON PFJ CONTACT AND MPFL STRAIN
Fixed rotation of either femur or tibia has been shown to have a significant influence on PFJ contact areas and pressures. Hefzy et al. (14) used a cadaveric model to
study the effects of tibial rotation on PFJ contact areas. The authors found that internal tibial rotation increased medial PFJ contact areas, whereas external tibial rotation increased lateral PFJ contact areas at all flexion angles. More recently, Lee et al. (15, 16 and 17) investigated the effects of rotational deformities of the lower extremity on PFJ contact pressures in a cadaver model. They simulated various types of rotational deformities of the femur and tibia by internally and externally rotating cadaver knees around the axis representing the distal third of the femur and the shaft of the tibia. They found that 30° of either internal or external femoral rotation created a significantly greater peak contact pressure respectively on the lateral or medial facet of the patella.
study the effects of tibial rotation on PFJ contact areas. The authors found that internal tibial rotation increased medial PFJ contact areas, whereas external tibial rotation increased lateral PFJ contact areas at all flexion angles. More recently, Lee et al. (15, 16 and 17) investigated the effects of rotational deformities of the lower extremity on PFJ contact pressures in a cadaver model. They simulated various types of rotational deformities of the femur and tibia by internally and externally rotating cadaver knees around the axis representing the distal third of the femur and the shaft of the tibia. They found that 30° of either internal or external femoral rotation created a significantly greater peak contact pressure respectively on the lateral or medial facet of the patella.
Lee’s findings have been confirmed in an independent study in whole cadaver limbs (including the femoral head and foot) stabilized by simulated quadriceps contraction. When the distal femur was internally rotated 30°, there was increased contact pressure on the lateral aspect of the PFJ and decreased contact pressure on the medial aspect of the joint. When the distal femur was rotated 30° externally, the opposite effect was observed (18).
Kijowski (Teitge et al., unpublished work) also studied the effects of femoral rotational osteotomy on strain in the MPFL. They found that 30° of experimentally induced internal femoral rotation (rotating the distal femur inward, simulating anteversion) of the femur resulted in significant increases in the strain of the MPFL. It is interesting to note that the effect of bony alignment on MPFL strain was much greater at 30° than at 60° or 90° of flexion. These observations corroborated Lee’s findings that medial patellofemoral retinacular strains were significantly affected only at low angles of knee flexion (16). The results of this study and Lee’s studies show that variations in femoral torsion cause alterations in the patterns of force transmission across the PFJ, including strain in the MPFL. Weight-bearing activity in individuals with an internally rotated femur could cause pain either by overload of the cartilage laterally or by abnormal strain in the MPFL. The MPFL could fail either acutely or by chronic overload in such knees.
Trochlear dysplasia alters the contact relationship between patella and trochlea. Since the contact area and thus the contact pressures are altered, trochlear dysplasia and patella shape should be evaluated when assessing malalignment. Trochlear dysplasia is an abnormality of the shape and depth of the trochlear groove (TG) mainly at its cephalad part, which has been associated with patellar instability, anterior knee pain, and early patellofemoral arthrosis (19, 20). Brattström (21) and others (22, 23) have studied trochlear geometry in recurrent dislocation of the patella and concluded that a shallow femoral groove (i.e., trochlear dysplasia) was the most common finding (Fig. 60.2). These and other authors, mostly in Europe, worked to develop strict and reliable protocols for radiographic evaluation in order to provide guidelines for the treatment of patients with patellar instability (24, 25). In the 1980s, Dejour et al. (23) defined several specific morphologic features commonly seen on radiographs of patients with patellar instability that were rarely seen in a population of control subjects (26, 27, 28 and 29). The fundamental anatomic feature distinguishing the two populations was the presence of trochlear dysplasia—a flattening or occasionally a convexity of the upper part of the TG—in a high percentage of recurrent patellar dislocators and in only 2% of control subjects.
 FIGURE 60.2. A: Normal trochlea. On the lateral view, the profile shows a sclerotic curved white line that corresponds to the floor of the trochlea (+). The curves representing the trochlear ridges (arrows) do not cross the curve of the trochlear floor. Note that accurate interpretation of the lateral view requires that the posterior condyles be aligned (B) and (C). B: The crossing sign is a simple and characteristic image, a qualitative criterion of trochlear dysplasia. The arrowhead indicates the point where the curve of the trochlear floor crosses the anterior contour of the lateral femoral condyle. By definition, the trochlea is flat at this level. This sign is of fundamental importance in the diagnosis. C: The prominence (bump) is a quantitative characteristic that is particularly significant in trochlear dysplasia. The prominence represents the distance between the most anterior point of the trochlear floor (dashed line) and a line drawn along the distal 10 cm of the anterior femoral cortex (solid line). (From Fithian DC, Neyret P, Servien E. Patellar instability: the lyon experience. Tech Knee Surg. 2007;6(2):112-123, with permission.) |
These studies provide strong circumstantial evidence to suggest that abnormal skeletal alignment of the lower extremity is an important factor in the pathogenesis of various disorders of the PFJ.
CLINICAL EVALUATION
Pertinent History
The knee extensor mechanism is a complicated and delicate system, the treatment of which is only further complicated by surgery if the surgeon has not clearly defined the pathologic basis of the presenting complaint. The chief complaint should guide the workup and the discussion of treatment options; this will help the physician to focus on the patient’s needs and expectations. For example, the patient who seeks help for relief of daily pain has a very different problem than one complaining of occasional sharp pain and giving-way. Although pain itself can result in knee instability (a symptom), it is important to differentiate painful knee giving-way from episodic pain due to patellofemoral laxity. Pain and catching in early flexion points to an articular lesion at the inferior patella or proximal trochlea; pain throughout the range indicates a more diffuse, perhaps extra-articular process. As the clinician develops an understanding of the symptoms and complaints, he or she can begin to develop one or more hypotheses, which can be tested in the physical examination and with subsequent imaging studies. The isolated complaint of pain, with no objective findings to suggest a specific source (pathology) representing an indication for surgery, should be treated nonoperatively.
 FIGURE 60.3. The step-down test is a simple test that can be done in the clinic to evaluate core and hip control. A: The patient on the left demonstrates pelvic weakness with hip adduction and medial collapse of the knee. B: Schematic showing the potential contributions of the various lower-extremity segments to abnormal alignment: (1) contralateral pelvic drop, (2) femoral internal rotation, (3) knee valgus, (4) tibia internal rotation, and (5) foot pronation. (From Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639-646, with permission.) |
Physical Examination
Owing to the complex and delicate interactions between the knee extensor system and the lower limb function, clinical evaluation of patellofemoral complaints can be challenging. After other disorders have been ruled out, specific testing for disorders of the PFJ can be performed. The patient should be first evaluated standing, walking, and stepping up and down from a small step, squatting, sitting, supine, running, and jumping (Fig. 60.3). Any hindfoot valgus, forefoot pronation, and/or heel cord tightness should be noted as they can affect tibial rotation and patellofemoral alignment (30).
Femoral and tibial rotation can be estimated by examining the patient prone with the hips extended, the knees flexed 90°, and the feet and ankles in a neutral, comfortable position with the soles of the feet parallel to the floor after the method of Staheli et al. (31) This position allows
estimation of femoral internal and external rotation limits as well as the foot-thigh angle (FTA) and/or transmaleolar axis (TMA). Kozic et al. (32) showed that on physical examination, femoral anteversion should be suspected if prone hip internal rotation exceeds external rotation by at least 45°. With respect to estimating FTA and TMA, Staheli et al. (31) reported a wide range of normal values, with mean values of 10° for FTA and 20° for TMA. Souza and Powers (33) also confirmed the reliability of the Staheli method for estimating femoral anteversion, though axial imaging was more precise. Our preferred approach is to use the prone physical examination to screen for torsion of the tibia and femur, and to obtain CT scan to assess rotational alignment if hip IR exceeds ER by at least 20° or if the prone foot-thigh axis or TMA is greater than 20°.
estimation of femoral internal and external rotation limits as well as the foot-thigh angle (FTA) and/or transmaleolar axis (TMA). Kozic et al. (32) showed that on physical examination, femoral anteversion should be suspected if prone hip internal rotation exceeds external rotation by at least 45°. With respect to estimating FTA and TMA, Staheli et al. (31) reported a wide range of normal values, with mean values of 10° for FTA and 20° for TMA. Souza and Powers (33) also confirmed the reliability of the Staheli method for estimating femoral anteversion, though axial imaging was more precise. Our preferred approach is to use the prone physical examination to screen for torsion of the tibia and femur, and to obtain CT scan to assess rotational alignment if hip IR exceeds ER by at least 20° or if the prone foot-thigh axis or TMA is greater than 20°.
The lines of action of the quadriceps and the patellar tendon are not collinear. The angular difference between the two is the quadriceps angle, or “Q-angle.” Because of this angle, the force generated by the quadriceps serves both to extend the knee and to drive the patella laterally, compressing the femoral trochlea in order to convert tension in the quadriceps into extension torque at the knee. The relative magnitude of the laterally directed force is related to the Q-angle. External rotation of the tibia, internal rotation of the femur, and increasing knee valgus all cause an increase in the Q-angle and thus an increase in the laterally directed force within the PFJ (Fig. 60.4) (30). However, use of the Q-angle alone grossly underestimates the complexity of patellofemoral alignment and often leads to errors of diagnosis and treatment. Furthermore, the Q-angle is highly variable and unreliable as a measurement (34, 35). These considerations have led the International Patellofemoral Study Group (IPSG) to recommend abandonment of clinical measurement of Q angle, preferring imaging studies to estimate the lateralizing vector at the PFJ (see TT-TG offset below under “Imaging”).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree