Inside-Out and Outside-in Meniscus Repair
Peter R. Kurzweil
As our knowledge of the role the meniscus plays in knee function increases, preserving it becomes increasingly important. Even a small partial meniscectomy can significantly alter joint biomechanics. Removing less than a third of the meniscus will increase contact pressure greater than 350%. Arthroscopic inside-out repair techniques gained popularity in the early 1980s. Outsidein procedures were subsequently developed to decrease the risk of neurovascular injury. All-inside methods are increasingly performed due to ease of technique, reduced operative times, and even lower risk of injury to the neurovascular structures. The goal of this chapter is to provide a comprehensive overview of suture repair of the meniscus with the outside-in and inside-out techniques.
The medial and lateral menisci are not mirror images of each other. The medial meniscus has extensive peripheral attachments to the capsule and medial collateral ligament (MCL). The lateral meniscus has fewer capsular attachments, none at the popliteal hiatus, and no contact with the lateral collateral ligament (LCL). The lateral meniscus is more mobile and can translate up to 1 cm with knee range of motion.
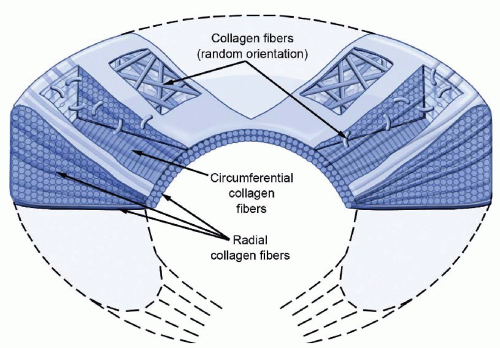
The meniscus is 90% type I collagen, with the majority of the fibers aligned circumferentially (Fig. 57.1). This orientation permits absorption of the hoop stresses generated when the joint is loaded. Radially oriented fibers act to bundle together the circumferential fibers, adding strength to the overall construct. The vertical mattress stitch configuration, which mimics the path of the radially oriented fibers, has a greater repair strength than other suture orientations.
It is important to understand the vascularity of the meniscus when considering the healing potential of a tear. It is generally thought that increased vascularity correlates with better healing potential. Branches of the medial and lateral genicular arteries perforate the menisci at the capsular attachments. In the lateral meniscus, the popliteal hiatus lacks any peripheral blood supply and is essentially avascular in this region. For clinical purposes, the repairable zone of the meniscus is generally within 5 mm of the peripheral rim. This is the so-called red-red or red-white zone.
CLINICAL EVALUATION
A thorough evaluation including the patient’s history, physical exam, and imaging studies can lead to an accurate diagnosis of a meniscus tear in most cases. Meniscal tears in younger patients are typically caused by a traumatic event that involves twisting or hyperflexion. Older patients may have degenerative changes in the menisci, resulting in tears with less dramatic events or even no history of injury. Symptoms typically include knee pain, swelling, locking, catching, and giving out. In the acute phase patients often limp and cannot squat.
Although several tests focus specifically on meniscal injuries, no single physical exam finding can reliably predict the presence of a tear. A recent meta-analysis found a sensitivity and specificity of 60% to 70% for the McMurray’s and Apley’s tests and joint line tenderness. Nevertheless, taken all together, these specific meniscal tests can give the examiner a fairly reliable method to determine whether a tear is present.
The first finding to observe is knee extension. A locked knee (with a fixed flexion contracture) is typically caused by mechanical block and is commonly seen with a bucket-handle meniscus tear. Specific focal joint line tenderness can be another clue, particularly when an effusion is present. Joint line tenderness is best assessed with the patient relaxed (sitting or supine) and the knee gently flexed close to 90°. There are three provocative maneuvers that we routinely use, although doing them depends on the patients level of guarding. The McMurray test may be too painful with an acute knee injury. In chronic situations, it can reproduce the patient’s symptoms. However, if knee pain and guarding precludes performing a McMurray test, then we do an Apley’s test. The patient sits with the legs dangling over the side of the exam table, and the knee is twisted internally and externally by rotating
the foot and ankle. A positive test refers pain to the joint line. Finally, in more chronic cases, the Thessaly test is extremely helpful. This test requires a single leg stance with the leg slightly bent. The patient is then asked to twist back and forth through the knee. This frequently reproduces the knee symptoms. We typically ask the patient to perform this maneuver on the good leg first, to make sure they can do it and that it is painless.
the foot and ankle. A positive test refers pain to the joint line. Finally, in more chronic cases, the Thessaly test is extremely helpful. This test requires a single leg stance with the leg slightly bent. The patient is then asked to twist back and forth through the knee. This frequently reproduces the knee symptoms. We typically ask the patient to perform this maneuver on the good leg first, to make sure they can do it and that it is painless.
Diagnostic Imaging
Imaging begins with the standard 4-view series of the knee, which includes weight-bearing anteroposterior (AP) and tunnel (45° posterior-anterior view), lateral, and sunrise views. Unless there is chondrocalcinosis, the menisci are not visualized. Nevertheless, plain radiographs provide valuable information regarding knee alignment, preservation of joint space, and other possible sources of knee pain.
MRI has become the gold standard for meniscal imaging, although it should be remembered when interpreting the study that the number of patients with asymptomatic tears increases with age. The MRI can also provide information regarding tear size, location, and configuration. A recent retrospective review showed that the preoperative MRI scan could accurately predict more than 90% of the time when a tear is reparable. We typically prefer not to use intra-articular contrast when imaging the menisci for tears on routine studies. The one situation that we request its use is when there is a need for assessing whether a prior meniscal repair may have retorn.
TREATMENT
Once a patient has been diagnosed with a symptomatic tear of the meniscus, several parameters should be considered when assessing the reparability of the tear. Many of these factors are best judged arthroscopically, including vascularity, size, instability, tear orientation, and tissue quality. Knee stability is another factor to consider when contemplating meniscal repair. Studies have repeatedly shown that a concomitant anterior cruciate ligament (ACL) reconstruction enhances the success rate of meniscus repair while healing rates are less than 30% in an ACLdeficient knee.
Nonoperative
Not all meniscus tears require surgery. As discussed, several studies have shown that the incidence of asymptomatic meniscal tears increases with age. If one such patient sustains a knee injury and an MRI is obtained, the scan will show a meniscus tear. However, there was no way to discern whether or not the tear was preexisting from the scan. It is important to correlate the patient’s symptoms, mechanism of injury, and exam with the MRI. Patient education is also important in this scenario, as patients have come to suppose that the diagnosis from the MRI reading is “right” and subsequently expect an arthroscopic surgery. We have successfully treated numerous patients in this situation, where we concluded that the symptoms were not arising from the meniscus tear seen on MRI.
Once in surgery, not all meniscus tears are repaired or resected. Partial or small (<5 mm) tears that are judged to
be stable are typically left alone, especially when located near the peripheral rim. Also, stable tears posterior to the popliteus tendon generally do not need to be resected or repaired when seen at the time of ACL reconstruction.
be stable are typically left alone, especially when located near the peripheral rim. Also, stable tears posterior to the popliteus tendon generally do not need to be resected or repaired when seen at the time of ACL reconstruction.
The protocol for nonsurgically treated meniscus tears includes a short period of restricted weight bearing and immobilization. Following resolution of the effusion and pain from the acute injury, a rehabilitation protocol is implemented that includes strengthening and range of motion. We restrict squatting and twisting activities until symptoms have resolved.
Operative
Before considering a repair, the patient should understand the postoperative restrictions that will be necessary for a successful outcome. We counsel patients and their families that despite adhering to the rehabilitation protocol, there is a 20% chance of failure that would require a second procedure. The possibility of needing additional small incisions and neurovascular risks is also discussed. Furthermore, despite the best intentions of repairing the meniscus, not all tears are reparable, and the ultimate decision regarding treatment is made in surgery. If these factors are not acceptable to the patient, they may request a meniscectomy, with a more reliable short-term outcome and quicker recovery.
TECHNIQUE
With the goal of avoiding scuffing of the articular cartilage, complete relaxation with general anesthesia facilitates instrumentation of the tear site. It would not be possible to apply a significant valgus force to the knee to open the medial compartment with local anesthesia. There would also be concern about discomfort when making accessory incisions for the repair if patients were awake. Prolonged positioning in the Figure 57.4 position, which opens up the lateral side would also be uncomfortable. Local anesthetics containing epinephrine are injected around the portals and accessory incision sites, but we are reluctant to use large doses of intra-articular local anesthetics, which would be required for surgery under local anesthesia.
A nonsterile tourniquet is applied to the proximal thigh, but rarely inflated. Avoiding tourniquet use allows better assessment of the vascularity of the tear. Gravity inflow is used, as the higher pressure from the fluid pumps may hinder bleeding at the tear site and could also lead to excessive joint swelling postoperatively.
Meniscal Preparation
Preparation of the tear, like a fracture, includes freshening the edges, reducing it anatomically, and (sometimes) insertion of provisional fixation prior to final fixation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree