Double-Bundle Acl Reconstruction
James R. Romanowski
Verena M. Schreiber
Freddie H. Fu
Anterior cruciate ligament (ACL) injuries continue to be one of the most common problems that orthopedic surgeons encounter. With an annual incidence of about 1 in 3,000 knees, approximately 100,000 ACL reconstructions are performed each year (1, 2). Management of these ligament ruptures varies, but ranges from nonoperative modalities to various methods of surgical reconstruction. Significant resources have been committed toward studying every aspect of the ACL including the anatomy, biomechanics, intra- and extraarticular reconstruction methods, as well as synthetic ligament substitutes and optimization of allograft and autograft sources. With such a multifaceted commitment toward research, it is not surprising that the management of these injuries has evolved as the understanding of the ACL has improved.
A primary tenant of orthopedic surgery is anatomy. Without a clear understanding of the affected structure and the associated function, accurate restoration of function with surgical reconstruction will fail. Originally described in 1938, the ACL consists of two bundles: the anteromedial (AM) and the posterolateral (PL) (3) (Fig. 71.1). An occasionally recognized anatomic variant includes a third, or intermediate (IM) bundle. The nomenclature is based on the tibial insertion of each bundle. These individual areas of insertion provide important functional contributions to both anterior-posterior (AM bundle) and rotational stability (PL bundle) (4).
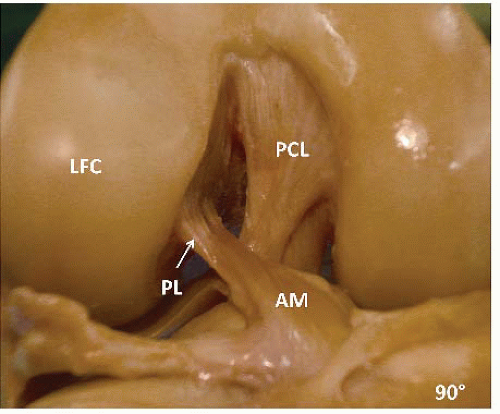 FIGURE 71.1. Right knee showing the ACL with the AM and PL bundles. LFC, lateral femoral condyle; PCL, posterior cruciate ligament. |
The primary goal of surgical intervention is to restore function. Every patient has a unique ACL footprint, therefore, it is of paramount importance to respect anatomic landmarks for proper identification of the origins and insertions of each ACL bundle. It is this uniqueness that precludes generalization to a particular “o’clock” or set millimeter reference for tunnel placement. Furthermore, there is a significant risk of tunnel mismatch, that is, PL tibial tunnel to AM femoral tunnel. Most surgical reconstructions for ruptured or dysfunctional ACLs have been single-bundle reconstructions. Single-bundle techniques have enjoyed relatively successful outcome in terms of stability and return to sport, but long-term results have revealed several shortcomings and only approach normal International Knee Documentation Committee (IKDC) scores in 61% to 67% of patients (5).
As the understanding of the ACL evolves, optimizing each functional component will allow for continued improve patient outcomes.
CLINICAL EVALUATION
As with any patient complaint, it is necessary to perform a thorough history and physical evaluation.
Pertinent History
The patient with a torn ACL typically presents with one of two scenarios. A noncontact injury sustained during pivoting or cutting activities, or from traumatic contact. Establishing the mechanism of injury remains important as it may suggest other pathologies, particularly with varus or valgus loads with subsequent injury to the MCL, LCL, PL corner, and menisci. Failure to recognize additional structural injuries will result in higher failure rates regardless of the reconstructive method (6). Oftentimes, a “pop” is described and an effusion present. Some patients
will attempt to return to activities before seeking treatment and may complain of persistent instability. For those that deny instability but have an isolated ACL tear, this may be a significant factor in the decision-making process and avoid surgery.
will attempt to return to activities before seeking treatment and may complain of persistent instability. For those that deny instability but have an isolated ACL tear, this may be a significant factor in the decision-making process and avoid surgery.
Age is also an important consideration. Within the preadolescent and teenager population, it is critical to evaluate growth plates, and those with advanced age have increased risk of degenerative joint disease that may preclude surgical intervention.
Lifestyle should also be evaluated as a sedentary individual may not have the same functional demands as an elite athlete. Prior surgical procedures or infections of the affected extremity must be considered as there are associated surgical risks.
Physical Examination
Most patients are evaluated in the office setting, however, evaluation at the time of injury can provide valuable information as there is little/no swelling present. The patient is asked to wear shorts to allow for direct visualization of both lower extremities and comparison throughout the examination. The affected knee is first inspected noting any joint effusion, bruising, or atrophy. The overall alignment is also observed as significant angular deformities may need to be addressed. The range of motion is measured and followed as this needs to be optimized prior to any surgical intervention. Palpation of all bony prominences as well as the joint line and parapatellar region helps identify associated meniscal, ligamentous, and patellofemoral injuries. Tests specific for the ACL ruptures are performed including the Lachman, anterior drawer, and pivot shift maneuvers. Although more sensitive, the pivot shift may be difficult as patients tend to guard especially in the acute setting. Supplementing the examination, the McMurray, varus and valgus stress at 0° and 30°, Dial, reverse pivot shift, and posterior drawer testing are performed for completion.
Objective methods are also employed as part of the evaluation and include the KT-2000 arthrometer. Dysfunction or disruption of the ACL is suggested with sideto side differences greater than 3 mm.
Imaging
Radiographs remain a key component during the workup of ACL-injured patient and help to identify tibial spine avulsions or rule out associated fractures, evaluate limb malalignment, and assess with open growth plates. Standard radiographs include the weightbearing full extension and 45° posteroanterior X-rays, nonweightbearing lateral, and merchant views. For patients where the physical examination suggests lower extremity malalignment, a bilateral long cassette view is obtained for further assessment. The need for an MRI is arguable, but patients often present having already had the study and within our practice an MRI is obtained for further identification associated injuries.
CT scans are not necessary for primary ACL reconstruction, but have a preoperative role in revision cases.
Decision Making
Persistent instability that causes functional limitations with either activities of daily living or with sports remain critical aspects when deciding whether or not to pursue surgical intervention.
TREATMENT
Nonoperative
Sedentary or low demand patients who can modify their activities may pursue conservative management.
Operative Indications
Surgery is typically reserved for individuals with persistent instability or symptoms associated with the ACL tear or dysfunction. Candidates include patients with functionally demanding employment, high-level athletes, and individuals who are limited in their activities of daily living secondary to the ligamentous compromise. Age is a consideration that is related to the presence of open growth plates in children and adolescents, and the potential for degenerative arthritis in older individuals. Double-bundle reconstructions should be avoided with open growth plates because the technique involves a larger area of the tibia, theoretically increasing the risk of growth arrest. Double-bundle constructs should also be avoided in multiligamentous injuries, advanced knee arthritis, active sepsis, and in noncompliant patients that cannot follow postoperative rehabilitation protocols.
Timing
Considerable debate remains over the appropriate timing of surgical reconstruction after injury to the ACL (8). Although there is no consensus, it is generally agreed upon that the patient should regain range of motion (0° to 120°) and reestablish quadriceps control preoperatively to avoid postoperative arthrofibrosis (9). Acute reconstruction (<3 weeks) has been associated with significantly increased rates of arthrofibrosis, with some series reporting up to 37% of patients experiencing loss of motion versus only 5% in individuals with delayed intervention (10, 11). Delay in surgical intervention has been found to increase the risk of cartilage damage 1% per month of surgical delay (8). Furthermore, there is a higher risk of secondary meniscal tears and degenerative arthritis in individuals that delay surgery greater than 12 months from the time of injury (12). Our current practice is to perform subacute reconstruction (>3 weeks) after successful preoperative rehabilitation.
TECHNIQUE
Anesthesia
Prior to surgery, the surgeon identifies, initials, and marks the operative site with a “yes.” A discussion is held between the surgeon, anesthesiologist, and the patient to develop an appropriate anesthesia regimen. Typically, peripheral nerve blocks involving the femoral and sciatic nerves are performed by an experienced anesthesiologist utilizing ultrasound guidance. In combination with “light” sedation, these temporary nerve blocks provide adequate intraoperative pain control and helps minimize postoperative narcotic use.
Setup and Examination under Anesthesia
The patient is brought back to the operating suite and placed supine on the OR table. After adequate anesthesia and analgesia, an examination under anesthesia is performed. Specific tests include the Lachman, pivot shift, anterior drawer, posterior drawer, varus/valgus stress, Dial testing, and range of motion. The foot of the table is maximally flexed, allowing for. The nonoperative limb is comfortably place in a well-padded leg holder with the hip and knee flexed to 80° to 90° and positioned in abduction. A tourniquet is placed proximally on the operative thigh and secured with a bolster. All neurovascular and bony prominences are cushioned and protected. Securing the leg in slight hip flexion (10° to 20°) allows for increased knee flexion for later femoral tunnel creation. The operative knee should have a range of motion from 0° to at least 120° (Fig. 71.2).
Surface Landmarks and Incisions
Critical to the success and limited invasiveness of arthroscopic ACL reconstruction are appropriately placed skin incisions. With properly placed portals, a notchplasty is not required and all tunnels may be created with careful portal placement. The anatomic landmarks are identified and marked, including the inferior pole of the patella, medial, and lateral borders of the patellar tendon, medial joint line, tibial tubercle, and anterior and posteromedial borders of the tibia. Additional incisions may be required for meniscal repair depending on the chosen technique. The leg is elevated and an esmarch is used to exsanguinate the leg for tourniquet insufflation.
With the knee in 90° of flexion, the anterolateral portal (LP) is established just lateral to the origin of the patellar tendon on the inferior pole of the patella. A no. 11 blade scalpel is used to make the vertical incision. The arthroscopic trocar is then used to enter the joint and sweep under the medially lying fatpad. This portal is used primarily for visualization of the tibial ACL footprint.
Again with the knee in 90° of flexion, the central medial portal (CMP) is established. A no. 18G spinal needle is used to determine the trajectory of the instrumentation and visualization pathway from the CMP. The needle typically follows the course of the normal ACL. The skin incision should be tangential to the medial border of the patellar tendon and just superior to the anterior horn of the medial meniscus. This position allows for optimal visualization of the notch and femoral footprint. It also allows for adequate working space for the third arthroscopic portal—the Accessory medial portal (AMP). A no. 11 blade scalpel is used to make a vertical incision in the skin, carefully cutting away from the underlying medial meniscus. Prior to placement of the AMP portal, it is often necessary to debride the fatpad and improve arthroscopic visualization to optimize the portal placement (Fig. 71.3). The accessory medial portal is perhaps the most critical of all the portals as the trajectory must capture the AM and PL ACL origins of the femur while avoiding damage to the cartilage surface of the medial femoral condyle. If the portal is placed too medial, then the femoral AM tunnel entrance angle may be too acute and risk posterior wall blowout of the lateral femoral condyle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









