Arthroscopic Management of Osteochondritis Dissecans of The Elbow
KEY POINTS
Osteochondritis dissecans (OCD) of the elbow is a disorder common in young repetitive-motion athletes.
Although often characterized by inflammation, pain, and loss of motion, the pathologic changes within the bone itself have no inflammatory cells.
Nonoperative management includes elimination of the secondary inflammatory changes by the use of anti-inflammatory modalities combined with elimination of the stress to the capitellum by rest and the use of an off-loading hinged elbow brace.
Nonoperative management is most effective when the cartilage cap overlying the lesion is intact.
Surgical intervention may take several forms when the disorder either does not respond to nonoperative management or is discovered in a later stage.
Percutaneous fixation of nondisplaced lesions is an attractive option when there is enough bone in the loose fragment to allow purchase of the fixation device.
Arthroscopic removal of loose bodies, excision of an inflamed posterolateral plica, and microfracture of the residual defect may be of benefit in the intermediate stages.
In cases in which these options fail or in which there is extensive destruction of the bone and involvement of the extreme lateral cortex or “shoulder” of the capitellum, osteochondral grafting may be indicated.
Results of each treatment modality are quite good, with success rates reported between 66% and 95%.
The primary complications include loss of motion, early arthritis, and a failure to return to the same level of competition.
OCD is a localized condition involving the articular surface that results in the separation of a segment of articular cartilage and subchondral bone. Konig was the first to report on this condition in 1888 as an entity that produces loose bodies in the hip and knee in the absence of direct trauma. The term osteochondritis means an inflammation of bone and cartilage, whereas the word dissecans is derived from the Latin word “dissec,” meaning to separate. The use of this term has persisted despite the absence of inflammatory cells in histologic sections of excised osteochondral fragments.
Panner first described OCD in the elbow as a lesion that appeared similar to Legg-Calves-Perthes disease. The most common site of OCD of the elbow is the capitellum, with the lesion typically involving the central or anterolateral portion. However, lesions have also been reported in the trochlea, radial head, olecranon, and olecranon fossa.
The exact etiology of OCD remains unproven; however, most research suggests that repetitive microtrauma plays an integral role in the pathophysiology. There is also evidence to support an ischemic theory for the development of OCD. Haraldsson demonstrated that the immature capitellar epiphysis is supplied by one or two isolated vessels that enter the epiphysis posteriorly and traverse the cartilaginous epiphysis to supply the capitellum. No contribution was detected from the metaphyseal vasculature. The structure of this blood supply may predispose the capitellum toward osteonecrosis.
Elbow OCD typically occurs in athletes aged 11 to 21 years who report a history of overuse. Adolescent athletes engaged in repetitive stress activities such as baseball, gymnastics, cheerleading, and swimming are at highest risk for the development of OCD. Males are affected more frequently than females and symptoms are typically seen in the dominant arm.
Several authors have commented on the relationship between this condition, baseball pitching, and competitive gymnastics. The creation of compressive and/or shearing forces in the radiocapitellar joint is believed to be the common denominator. The radiocapitellar joint acts as a secondary stabilizer of the elbow, in addition to accepting up to 60% of the force of compressive axial loads. The valgus stress on the elbow during the cocking phase of throwing creates a substantial compressive load at the
radiocapitellar joint. This force may be responsible for the creation of subchondral fractures or the disruption of a tenuous blood supply to the capitellum.
radiocapitellar joint. This force may be responsible for the creation of subchondral fractures or the disruption of a tenuous blood supply to the capitellum.
CLINICAL EVALUATION
History
OCD is primarily a disorder of the young athlete. The usual age of presentation is 12 to 14 years of age, compared with 9 to 10 for Panner’s disease. Males are affected more often than females, but there is a high prevalence in young female gymnasts and competitive cheerleaders. The dominant arm is most often involved with bilateral involvement in 5% to 20% of patients. There is usually a history of overuse, most commonly throwing, repetitive impact, or overhead sports. Early on, the symptoms may be obscure, with pain location difficult to determine. It most often begins with some mild aching after activity. Most patients will try self-medicating with anti-inflammatory medicine and ice, which may provide some temporary relief. Symptoms will often worsen very slowly. On presentation, the history is most often that of pain that increases with increased activity, loss of motion, and swelling on the lateral side of the elbow. Additional complaints of popping, clicking, or sudden “giving way,” especially with load bearing, may also be present.
Physical Examination
The classic physical findings include loss of terminal extension and swelling along the posterolateral joint line along with inflammation of the normal posterolateral plica. Valgus extension overload testing will produce pain over the lateral aspect of the elbow and result in a measurable increase in the loss of terminal extension. This is one of the key differentiating factors in the physical examination of OCD. Most throwing or hyperextension overuse injuries when tested in valgus will have the primary component of pain along the medial aspect of the elbow: the medial apophysis, the medial ulnar collateral ligament, or the flexor-pronator muscle. These may coexist with the OCD, but in OCD patients these instability stress maneuvers, especially the moving valgus overload test, will result in pain more on the lateral than on the medial side.
Imaging
The initial testing involves standard PA and lateral radiographs. These will usually show the classic findings of radiolucency in the central aspect of the capitellum. There may be a small area of increased opacity in the center of the radiolucency (Fig. 33.1). In the later stages, loose bodies may be present.
Additional testing may be warranted early in the course of treatment. Computed tomography (CT), CT arthrograms, and ultrasound have all been utilized in the evaluation of these lesions. However, MRI has become the standard modality for evaluation of these lesions. The key points to evaluate that will assist in determining appropriate management include the extent of the bone involvement, the integrity of the overlying cartilage cap, and the presence of loose bodies. Early lesions will show change on T1-weighted MRI images, but no change on T2 sequences. The cartilage covering will be intact, indicating an improved prognosis. Advanced lesions will show changes on both T1 and T2 images and may demonstrate a loose in situ bone fragment (Fig. 33.2). Assessment of the
integrity of the cartilage cap remains paramount. As the condition advances, the cartilage cap is violated, allowing synovial fluid between the fragment and the remaining capitellum. This jeopardizes any chance at union with fixation and may result in one or more loose fragments being shed into the joint. However, the simple presence of loose bodies does not definitively define a rupture of the cartilage, so MRI assessment remains necessary. The lesion that advances to the lateral edge or “shoulder” of the capitellum is a much more severe injury that requires more extensive reconstructive surgery (Fig. 33.3). In the most advanced cases, three-dimensional (3D) imaging may be helpful to define the loss of this critical lateral cortex (Fig. 33.4A-C).
integrity of the cartilage cap remains paramount. As the condition advances, the cartilage cap is violated, allowing synovial fluid between the fragment and the remaining capitellum. This jeopardizes any chance at union with fixation and may result in one or more loose fragments being shed into the joint. However, the simple presence of loose bodies does not definitively define a rupture of the cartilage, so MRI assessment remains necessary. The lesion that advances to the lateral edge or “shoulder” of the capitellum is a much more severe injury that requires more extensive reconstructive surgery (Fig. 33.3). In the most advanced cases, three-dimensional (3D) imaging may be helpful to define the loss of this critical lateral cortex (Fig. 33.4A-C).
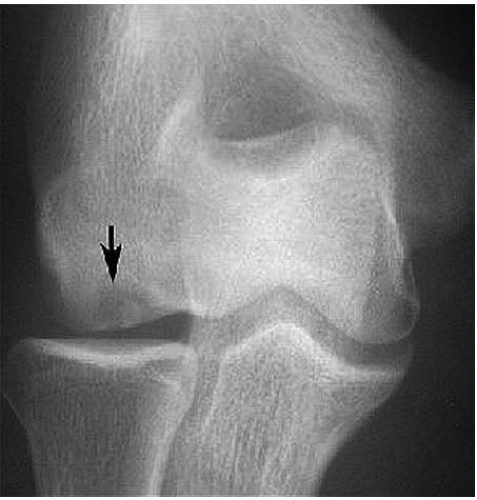 FIGURE 33.1. This posteroanterior view of the elbow delineates the area of radiolucency in the mid-capitellum, indicative of an early OCD lesion. |
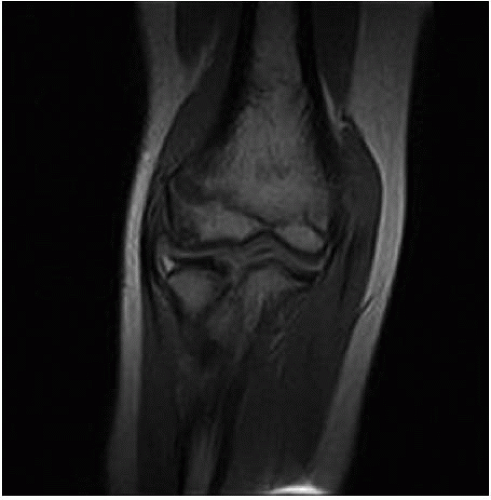 FIGURE 33.2. Magnetic resonance imaging may indicate either an intact or a disrupted cartilage cap as well as the presence of loose bodies within the defect.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





