Periarticular Ganglion Cysts of The Shoulder
Ronald P. Karzel
David W. Wang
As MRI has become commonly utilized to diagnose shoulder pathology, scans may reveal the presence of periarticular ganglion cysts in some patients with shoulder pain. Many of these cysts are small and of uncertain significance. However, larger ganglion cysts can cause significant shoulder pain and weakness, particularly if the cyst compresses the suprascapular nerve.
Compression neuropathy of the suprascapular nerve is rarely included in the differential diagnosis by health care providers. Compression of the nerve at the suprascapular notch was first described in 1959. By the 1980s, entrapment at the spinoglenoid notch had been recognized as a more common cause of suprascapular neuropathy. Later authors noted that compression at the spinoglenoid notch could be caused by a ganglion cyst. However, prior to the advent of newer radiographic and surgical techniques, the diagnosis was generally made incidentally while performing an open procedure to decompress the nerve. Shoulder MRI studies now allow surgeons to confirm the diagnosis preoperatively and noninvasively and to plan the best approach to decompress the cyst. Likewise, many surgeons have described advances in arthroscopic techniques that now allow less invasive treatment of the cysts and associated labral pathology. In this chapter, we will review the relevant pathology and anatomy, diagnostic findings, and current trends in the treatment of ganglion cysts.
PATHOGENESIS
The pathogenesis of ganglion cysts has not been clearly defined. Ganglion cysts are characteristically found in close proximity to joints, leading some to postulate that injury to the capsule may lead to the formation of the ganglion. A ganglion may develop when a capsulolabral tear allows synovial fluid to enter the adjacent soft tissues but not return, creating a one-way valve mechanism. This mechanism is well accepted in the formation of cysts around the knee and wrist and is gaining support in the shoulder since capsulolabral pathology is commonly noted adjacent to cysts (1). Several authors have described the association of ganglion cysts with glenoid labral tears (1, 2, 3 and 4). Piatt (3) identified posterosuperior labral tears using MRI in 65 of 73 patients with spinoglenoid cysts. Moore et al. (2) found a labral tear in 10 of 11 patients undergoing arthroscopy for the treatment of a ganglion cyst causing suprascapular nerve compression. In our study of 14 patients at the Southern California Orthopedic Institute (SCOI) who had superior glenoid cysts associated with suprascapular nerve palsy, all had labral pathology, and seven required superior labral reattachment (4).
The presence of small ganglion cysts on shoulder MRI studies is not uncommon. Our study at SCOI of ganglion cysts about the shoulder found that cysts less than 1 cm in size rarely caused symptoms, except that such cysts may be a sign of associated labral tearing. If the labral tears are large enough to cause mechanical symptoms or instability, then treatment might be required for the labral tear itself. Generally, cysts greater than 1 cm can be symptomatic when they cause nerve compression.
The suprascapular nerve is particularly susceptible to compression by a ganglion cyst at the spinoglenoid notch because the nerve is relatively immobile as it traverses the lateral edge of the scapular spine and is in close proximity to the posterior glenoid. Also, the scapular spine forms a rigid medial border to this space, providing a block to further expansion of the cyst. This leads to a progressive increase in cyst pressure, which compresses the nerve between the cyst and the bone ultimately causing nerve dysfunction. Bigliani et al. (5) showed in their cadaveric study that the average distance from the posterior glenoid rim to the suprascapular nerve was 1.8 cm. Similarly, Warner et al. (6) demonstrated in a cadaver model that the motor branches to the infraspinatus were 2.1 ± 0.5 cm from the posterior glenoid rim. Not surprisingly considering these findings, Tung et al. (7) found that cysts associated with denervation had an average diameter of 3.1 cm and were significantly larger than cysts not associated with muscle denervation (7).
Authors have theorized that ganglion cysts follow the paths of least resistance causing the cysts to dissect along the fibrofatty tissue overlying the suprascapular nerve and between the infraspinatus and the supraspinatus muscle
bellies. This dissection directs the cysts toward the spinoglenoid notch and the adjacent suprascapular nerve (Fig. 28.1). Given the relatively high frequency of superior labral tears compared with other labral tears, cysts may also be more likely to arise in this location. Presumably, an inferior labral injury could similarly result in fluid dissecting into the quadrilateral space. In fact, a case report showed a patient who developed axillary nerve compression from a paralabral cyst associated with an inferior labral tear (8). Successive MRIs over 5 years showed an increase in the size of the cyst associated with progressive muscle atrophy and fatty infiltration of the teres minor muscle.
bellies. This dissection directs the cysts toward the spinoglenoid notch and the adjacent suprascapular nerve (Fig. 28.1). Given the relatively high frequency of superior labral tears compared with other labral tears, cysts may also be more likely to arise in this location. Presumably, an inferior labral injury could similarly result in fluid dissecting into the quadrilateral space. In fact, a case report showed a patient who developed axillary nerve compression from a paralabral cyst associated with an inferior labral tear (8). Successive MRIs over 5 years showed an increase in the size of the cyst associated with progressive muscle atrophy and fatty infiltration of the teres minor muscle.
ANATOMY
A knowledge of the anatomy of the suprascapular nerve is critical to interpretation of this clinical presentation. The suprascapular nerve is a mixed motor and sensory peripheral nerve derived from the upper trunk of the brachial plexus formed by the C5 and C6 roots at Erb’s point. The nerve travels through the posterior triangle of the neck, deep to the brachial plexus and trapezius muscle, and enters the supraspinatus fossa through the supraspinatus notch. The nerve passes below the superior transverse scapular ligament, whereas the suprascapular artery and vein travel above the ligament. The space available for the suprascapular nerve at this location depends on the shape of the suprascapular notch and the size and structure of the transverse scapular ligament. This is a common location for suprascapular nerve compression to occur, and several authors have recently advocated arthroscopic techniques to decompress the notch.
The suprascapular nerve then supplies motor innervation to the supraspinatus muscle and receives sensory afferent signals from the coracoclavicular and coracohumeral ligaments, the acromioclavicular joint, and the subacromial bursa. Next, the suprascapular nerve travels toward the lateral border of the scapular spine, where it receives sensory input from the glenohumeral joint capsule.
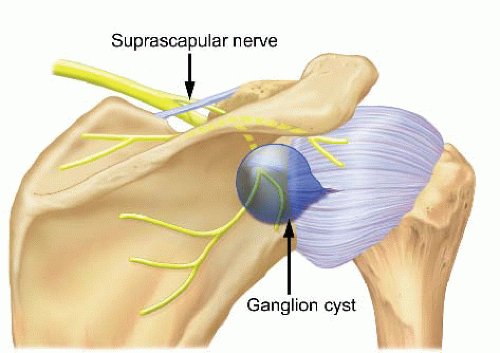 FIGURE 28.1. Cysts arising from the posterior superior labrum can enlarge and compress the suprascapular nerve against the spinoglenoid notch. |
The suprascapular nerve continues around the scapular spine, through the spinoglenoid notch, where it is relatively fixed in location by the inferior transverse scapular ligament. This ligament, also referred to as the spinoglenoid ligament, has been reported to have variable morphology and prevalence. When present, the ligament causes the suprascapular nerve to be relatively immobile as it passes through fibro-osseous tunnels at the spinoglenoid notch.
After the nerve passes through the spinoglenoid notch, it then terminates by giving two to four motor branches to the infraspinatus muscle belly (Fig. 28.2). A thorough knowledge of the anatomy of the suprascapular nerve allows the surgeon to correctly interpret the clinical findings and to determine the appropriate site for surgical intervention.
CLINICAL EVALUATION
History and Physical Examination
The diagnosis of suprascapular nerve compression by a ganglion cyst can be difficult to make on clinical exam alone because findings on the history and physical exam overlap significantly with other more common disorders, such as rotator cuff or labral pathology. However, some clinical findings are suggestive of suprascapular nerve compression due to a ganglion cyst. Cysts compressing the nerve at the spinoglenoid notch cause denervation of the infraspinatus muscle only. This may be seen clinically as isolated atrophy of the infraspinatus muscle. In contrast, compression of the nerve at the suprascapular notch causes denervation of both the supraspinatus and the infraspinatus. For this reason, patients should always be examined in attire that will allow the inspection of both shoulder girdles to search for asymmetry in muscle bulk that may be present with nerve entrapment (Fig. 28.3).
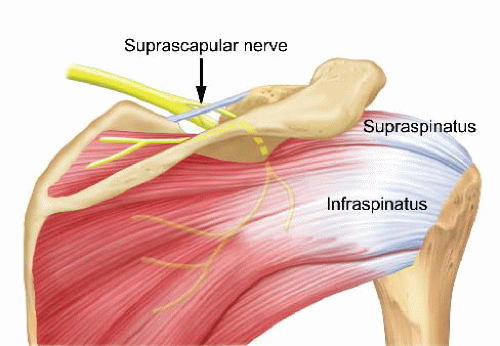 FIGURE 28.2. The suprascapular nerve innervates the supraspinatus muscle before passing around the spinoglenoid notch and sending branches to the infraspinatus muscle. |
There is often a history of trauma or some type of overuse, particularly overhead activity. Sports activities that have been implicated include volleyball, baseball, tennis, swimming, weightlifting, and other types of throwing. Regardless of the mechanism, most patients develop a capsulolabral injury that allows a cyst to develop. The presenting complaint is often nonspecific pain that is exacerbated by overhead activity. The pain may radiate medially and upward into the neck and laterally down the arm due to pressure on the sensory nerve branches. Suprascapular neuropathy often presents as vague, aching shoulder pain with varying degrees of abduction, and external rotation weakness. Although these complaints are more commonly due to rotator cuff disease or impingement syndrome, the orthopedist must consider neuropathy of the suprascapular nerve in the differential diagnosis. However, given its rarity, the lack of reproducible signs on physical exam, and the overlapping symptoms with other shoulder problems, this disorder is easily overlooked.
As the nerve compression progressively increases, the patient will often describe chronic pain and weakness that become constant, severe, and interrupt sleep. Patients may have pain to palpation in the spinoglenoid notch posteriorly or the suprascapular notch superiorly. Cross-body adduction has been described to localize pain to the posterior shoulder as the nerve is placed on stretch (9). If there is an associated labral tear, signs such as painful catching or locking may be present. Patients may present with painless infraspinatus wasting because the sensory portion of the suprascapular nerve may be unaffected in the distal spinoglenoid notch. A very common finding in these patients is marked weakness to resisted external rotation, tested with the arm at the side, without significant pain. In contrast to the patient with a rotator cuff tear, these same patients generally exhibit good strength to resisted supraspinatus testing with the arm in a forward elevated position. Such problems are relatively infrequent in women compared with men. This may be due to the generally lower incidence of superior labrum anterior and posterior (SLAP) lesions in women compared with men or with differences in the anatomy at the spinoglenoid notch.
Diagnostic Imaging
Plain radiographs, including AP, axillary, and supraspinatus outlet views, should be obtained to rule out any fracture, osseous compression, or erosion that might be present. The increasing use of MRI to evaluate shoulder conditions has demonstrated the presence of cystic lesions in patients with and without symptoms of suprascapular neuropathy. A cyst appears as a well-defined, smoothly marginated mass with low signal intensity on T1 images, which are better seen as high signal intensity masses on T2 images (Figs. 28.4, 28.5 and 28.6). MRI is also helpful for detecting associated intra-articular lesions such as labral pathology. Tirman et al. (1) found that all 20 patients reviewed retrospectively after arthroscopy had abnormal signal intensity of the labrum near the cyst. Another study found 89% of MRI scans of patients with cysts had associated pathology of the superior labrum, usually posterosuperior.
The sensitivity of MRI for associated labral pathology can be improved with MR arthrography (MRA). MRA has been shown to be the most sensitive technique for detecting labral tears. In a study by Chandnani et al., (10) MR arthrography with gadolinium injected intra-articularly was shown to have a sensitivity of 96% for detecting both labral tears and detachments in comparison with 93% and 46%, respectively, with standard MR imaging. Tung identified 60% of labral tears with paralabral cysts by standard MRI. However, with MR arthrography, contrast dissected into discrete labral tears in 100% of these patients (7). These findings support the theory that the paralabral cyst is probably a secondary sign of a labral tear in most patients, requiring treatment of the labral pathology to minimize recurrence.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









