Chapter 104 Surgical Approaches in Total Knee Arthroplasty
Standard and MIS Techniques
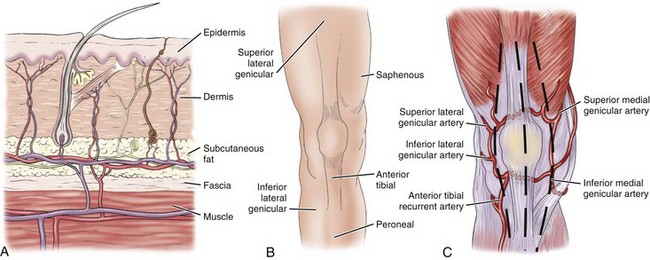
Critical to exposing the knee during total knee arthroplasty is a complete understanding of the local anatomy, which is described in Chapter 1. With such knowledge, the pathologic condition, anatomy, and planned surgery can be correlated. Although well-defined soft tissue layers provide reproducible planes of dissection,33,44,58 the blood supply to the skin should be respected, especially when previous incisions are present or multiple incisions are planned. Most of the blood supply to the skin arises from the saphenous artery and the descending geniculate artery on the medial side of the knee (Fig. 104-1).18,60 The vessels perforate the deep fascia and form an anastomosis superficial to the deep fascia. Continuing through the subcutaneous fat to supply the epidermis, little communication occurs in the superficial layer. Therefore, dissection should be deep to the fascia to maintain the blood supply to the skin.59 The blood supply to the skin should not be confused with the blood supply to the patella.
Many incisions and approaches to the knee joint were originally designed for open meniscectomy and reconstructive procedures before the advent of arthroscopy and are mainly of historical value.1 The intent of this chapter is to detail the surgical approaches that are useful for total knee arthroplasty. Many planned approaches are extensile but have been modified for performing minimally invasive surgery.20
Anterior Approaches
Skin Incisions
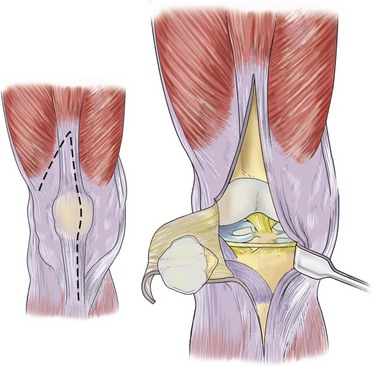
The anterior midline skin incision has provided a utilitarian extensile approach to the knee (Fig. 104-2). With proximal and distal extension of the skin incision, large flaps can be developed to expose the anterior, medial, and lateral supporting structures.27 If the midline skin incision is moved medially, it will be parallel to Langer’s cleavage lines and subject to less tension and disrupting force than would an anterior midline incision.57 Incisions parallel to the cleavage lines heal faster, gain strength more quickly, and result in a finer scar.31 No evidence indicates that this position creates any more hypoxia in the lateral skin margin than an anterior midline incision does.
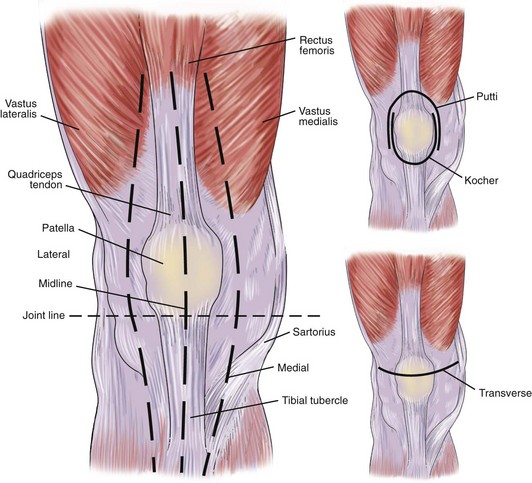
Figure 104-2 Anterior approaches to the knee.
(Redrawn from Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 56.)
The anterior Kocher U incision31 and the Putti inverted U incision42 have become obsolete, primarily because of complications associated with vascular compromise to the surrounding skin. The anterior transverse incision may be cosmetically pleasing, but it does not allow extensile exposure (see Fig. 104-2).57
Arthrotomy
The medial parapatellar arthrotomy, or anteromedial approach, has been the most used approach for exposure of the knee joint. It provides extensive exposure and is useful for open anterior cruciate ligament reconstruction, total knee replacement, and fixation of intra-articular fractures. Because this approach has been implicated in compromise of the patellar circulation (see Fig. 104-1C),51,52 some authors have advocated the subvastus, midvastus, and trivector approaches for exposure of the knee joint. Whereas these approaches expose the knee from the medial side, the anterolateral approach exposes the knee joint from the lateral side. With careful planning and arthrotomy selection, the anterior aspect of the joint can be fully exposed with these arthrotomies.
Medial Parapatellar Arthrotomy
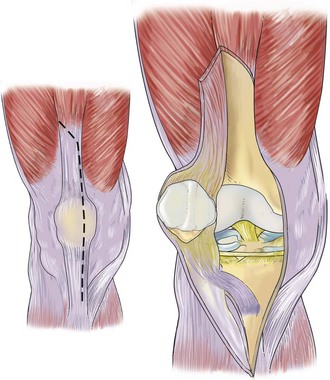
A medial parapatellar arthrotomy allows excellent exposure to most structures of the knee joint (Fig. 104-3). Von Langenbeck57 originally described dissection of the vastus medialis from the quadriceps tendon with distal extension through the medial patellar retinaculum and along the patellar ligament. The synovium is divided in line with the capsular incision, and the fat pad is retracted or incised. Because dissection continues to the joint line, one must be aware of the anterior horn of the medial meniscus, as well as the transverse ligament between the medial and lateral menisci. Completion of this arthrotomy permits the patella to be everted or subluxated laterally. When the patella is dislocated and the knee is flexed, care should be taken to avoid avulsing the patellar tendon from the tibial tubercle. If difficulty is involved in dislocating the patella laterally, the proximal quadriceps tendon incision should be extended superiorly or the patellar tendon carefully reflected subperiosteally along the medial border of the tibial tubercle to its crest. The patellar tendon must not be detached from the tibial tubercle.
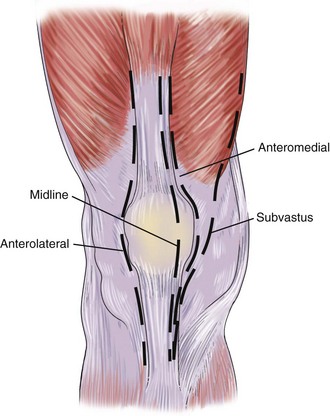
Figure 104-3 Preferred anterior approaches to the knee.
(Redrawn from Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 57.)
Insall23 modified the split patella approach, as described by Sir Robert Jones, because of damage to the patellar articular surface (Fig. 104-4). The extensor mechanism is exposed through a midline skin incision, the quadriceps tendon is divided 8 to 10 cm above the patella, and the incision is continued distally in a straight line over the patella and along the medial border of the patellar tendon. The quadriceps expansion is peeled from the anterior surface of the patella by sharp dissection until the medial border of the patella is visualized. The synovium is divided, and the fat pad is split along the midline. The patella is then dislocated laterally. No internervous plane is used with this approach; however, both the rectus femoris and the vastus medialis are supplied by the femoral nerve proximal to this incision.
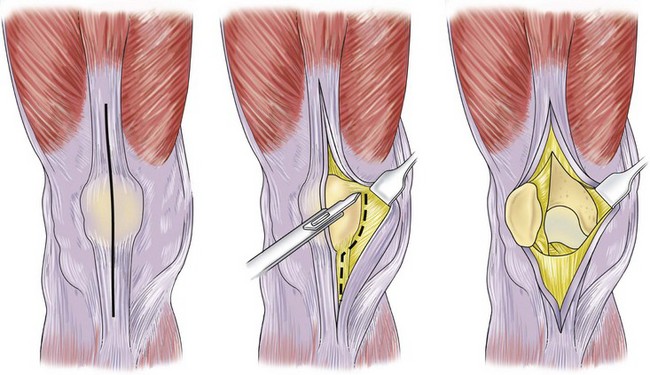
Figure 104-4 Insall’s anterior approach.
(Redrawn from Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 57.)
When the anteromedial approach is performed, the infrapatellar branch of the saphenous nerve comes into view (see Fig. 104-4, center). The saphenous nerve travels posterior to the sartorius muscle and pierces the fascia between the tendons of the sartorius and gracilis muscles, where it becomes superficial to the medial aspect of the knee. At this level, the infrapatellar branch of the saphenous nerve arises to supply the skin over the anteromedial aspect of the knee. Kummel and Zazanis,32 as well as Chambers,7 noted variation of this infrapatellar branch and recommended protecting it at the time of surgery to avoid painful neuromas. Insall et al24 believed that neuroma formation is more related to the patient’s temperament than to an actual pathologic condition.
Subvastus Approach
The subvastus approach, which allows direct access to the anterior knee joint, has been heralded as being more anatomic than the medial parapatellar arthrotomy (Fig. 104-5).21,39 The subvastus approach is applicable to most reconstructive procedures of the knee, with the exception of lateral unicompartmental replacement.
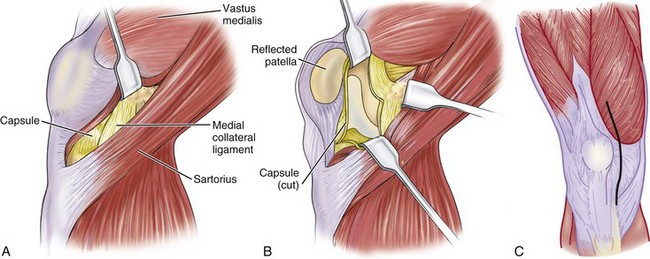
Figure 104-5 A and B, Subvastus approach. C, Trivector-retaining arthrotomy.
(A and B, Redrawn from Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 58; C, redrawn from Scuderi GR, Tria AJ: Surgical techniques in total knee arthroplasty, New York, 2002, Springer Verlag.)
Midvastus Approach
The midvastus muscle-splitting approach is performed through a standard anterior midline skin incision. The incision is carried down through subcutaneous tissue and deep fascia to expose the quadriceps musculature. The vastus medialis is identified, along with split full thickness, parallel to its muscle fibers. The quadriceps tendon is not incised. The incision is extended to the superior medial corner of the patella and then is continued distally along the medial patella and the patellar tendon to the level of the tibial tubercle. As with the subvastus approach, the capsule of the suprapatellar pouch is divided, so that the patella can be everted or subluxated laterally. Advocates of this approach believe that it is easier to evert the patella with the midvastus approach than with the subvastus approach because of the reduced bulk of the vastus medialis. In addition, this approach splits the muscle well away from its neurovascular supply.14
Trivector-Retaining Arthrotomy
The quadriceps musculature is exposed through an anterior midline skin incision. The trivector-retaining arthrotomy begins with transection of the vastus medialis obliquus muscle fibers 1.5 to 2 cm medial to the quadriceps tendon. Because the quadriceps tendon is not incised with this approach, the incision is extended distally 1 cm medial to the patella and the patellar tendon to the level of the tibial tubercle. It is recommended that this approach be performed with the knee flexed 90 to 110 degrees, so that the quadriceps musculature is under maximal tension during the incision. To evert the patella or subluxate it laterally, the capsule of the suprapatellar pouch must be divided.5
Anterolateral Approach
The anterolateral approach, as described by Kocher,31 consists of a lateral capsular incision that begins approximately 8 cm proximal to the patella at the insertion of the vastus lateralis muscle into the quadriceps tendon and continues distally along the lateral retinaculum (see Fig. 104-3). The incision can be extended distally through the fat pad for visualization of the lateral compartment and ends just distal to the tibial tuberosity. This approach is less favorable than the anteromedial approach because it is more difficult to subluxate the patella medially than laterally.
Lateral Parapatellar Approach
In performing this approach, a curvilinear midline skin incision or a laterally placed anterior skin incision is made and extended distally over the lateral border of the tibial tubercle. The joint is entered through a lateral parapatellar incision that extends from the lateral border of the quadriceps tendon, over the lateral margin of the patella, and continues distally into the anterior compartment fascia, 1.5 cm from the tibial tubercle, and for a distance of 3 cm from the tibial tubercle. To dislocate the patella medially and expose the joint, a thin segment of the tubercle is osteotomized with the attached patellar tendon. A medial periosteal hinge is maintained along with the infrapatellar fat pad, which is used for later closure of the lateral retinacular defect.6,29
Extended Approaches
Quadriceps Turndown
Coonse and Adams12 originally described a quadriceps turndown. They used a paramedian skin incision that begins at the lower end of the quadriceps tendon along the patella and extends along the medial border of the patellar tendon. Skin flaps are developed, the quadriceps tendon is split down the middle, and about 1 cm above the patella the incision is swung both medially and laterally and continues along the patella and the patellar tendon. The patella and the patellar tendon can be turned down to allow complete exposure of the joint (Fig. 104-6).
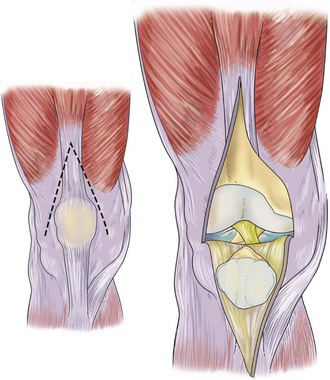
Figure 104-6 Coonse-Adams quadriceps turndown.
(Redrawn from Scott WN: The knee, vol 1, St Louis, 1994, Mosby-Year Book, p 66.)
Further modification of the patellar turndown approach26 involves the use of an anterior midline incision. A medial parapatellar arthrotomy is performed, and a second incision is made at an inclination of 45 degrees from the apex of the quadriceps tendon and extended laterally through the vastus lateralis and the upper portion of the iliotibial tract. This lateral incision stops short of the inferior lateral geniculate artery to preserve the blood supply (Fig. 104-7).
Quadriceps Snip
The full patellar turndown is now rarely necessary because cutting the quadriceps tendon proximally yields excellent soft tissue exposure, and functional reconstruction is possible (Fig. 104-8). This technique has been called the quadriceps snip by Insall.26 Following a long medial parapatellar arthrotomy, an oblique incision is made at the proximal apex of the quadriceps tendon. This incision is approximately at a 45-degree angle across the quadriceps tendon and directly in line with the fibers of the vastus lateralis. This extended approach relieves tension on the extensor mechanism and the tibial tubercle. As the tibia is externally rotated and the patella subluxated laterally, the joint is exposed.
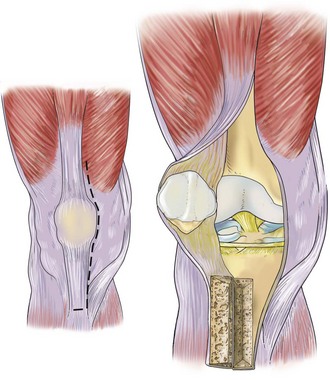
Tibial Tubercle Osteotomy
An anterior midline incision is made that extends 8 to 10 cm below the tibial tubercle. The medial parapatellar arthrotomy extends from 6 cm above the patella and distally along the tibial tubercle and anterior crest (Fig. 104-9). Whiteside and Ohl58 used this exposure for difficult total knee arthroplasty, and they recommend using an oscillating saw to transect the tibial crest 8 to 10 cm below the tibial tubercle while elevating the tibial crest from the tibia. The lateral periosteum and musculature structures are left attached, as is the lateral aspect of the quadriceps mechanism. Fernandez15 recommends tibial tubercle osteotomy for bicondylar tibial fractures. He uses a straight anterolateral parapatellar incision. Large medial and lateral subcutaneous flaps are developed. The osteotomy of the tibial tubercle is performed with an oscillating saw and osteotomes. The osteotomy is trapezoidal, 5 cm long, 2 cm wide, and 1.5 cm wide distally. Once the tibial tubercle and the anterior tibial crest are freed, the entire extensor mechanism is elevated proximally, and the retropatellar fat pad is divided to expose the entire joint.
Minimally Invasive Total Knee Arthroplasty
Total knee arthroplasty (TKA) has been performed for decades by using a traditional extensile approach. Historically, surgical exposure was achieved through an 8- to 10-inch skin incision and a long medial parapatellar arthrotomy, although some authors used a midvastus14 or a subvastus approach.21 This was followed by extensive soft tissue dissection and eversion of the patella. With improvement in the techniques of ligament balancing, adjustments in the overall alignment, and flexion-extension gap equalization techniques, good to excellent clinical outcomes have been reported in long-term follow-up studies for TKA completed using an extensile approach.*
The introduction of minimally invasive surgery (MIS) for unicondylar knee replacement45,47 encouraged interest in applying a similar approach to standard TKA. Various minimally invasive approaches, including limited medial parapatellar, limited midvastus, limited subvastus, and the quadriceps-sparing approach, are considered a continuum of traditional extensile approaches. The surgeon can shorten the skin incision as he or she becomes more familiar with the surgical technique, progressing along on the scale of complexity, and finally can become competent in performing quadriceps-sparing MIS TKA. The MIS approach can be easily converted to a traditional approach if required. Potential benefits of less invasive surgery include reduced blood loss, reduced pain, less morbidity, and faster recovery.34,50,55 The primary objective in MIS TKA is to limit surgical dissection without compromising component position, ligament balancing, or overall limb alignment. Modification of TKA instrumentation has facilitated the procedure, but appropriate patient selection remains critical for a successful outcome. The ideal candidate for MIS TKA is a patient with minimal deformity and good preoperative motion, who is of small to average stature. Our patient selection preference has evolved to include patients with less than 15-degree varus, 20-degree valgus, or 10-degree flexion contracture, with a minimum of 90-degree range of motion. Short, thin females with low body mass index and narrow femurs are good candidates for this approach.50 Muscular males with prominent vastus medialis and wider femurs often are better served by a more traditional approach. Patients with a compromised soft tissue envelope or a short patellar tendon, and those with severe deformities requiring extensive release, tend to need a standard approach. Moreover, patients with diabetes mellitus or rheumatoid or inflammatory arthritis and those who are obese tend to be less favorable candidates for MIS TKA.55
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree