Chapter 2 Surgical Anatomy of the Elbow
Osteoarticular anatomy
Humerus
The shaft of the humerus ends distally in both lateral and medial ridges. Thereafter lateral and medial epicondyles are formed (Figs 2.1 and 2.2). They can be inspected and palpated during clinical examination, the medial part being better defined than its lateral counterpart. The flexion crease of the skin on the anterior aspect of the elbow is at the same level as a line joining the two epicondyles, 1 cm proximal to the elbow joint. The presence of an accessory origin of the pronator teres muscle, approximately 5 cm superior to the medial epicondyle on the anterolateral side of the humeral shaft, can be found in 1–3% of individuals. In these cases, the ligament of Struthers attaches to a bony prominence and can sometimes cause compression of the median nerve that travels beneath the ligament along with the brachial artery.
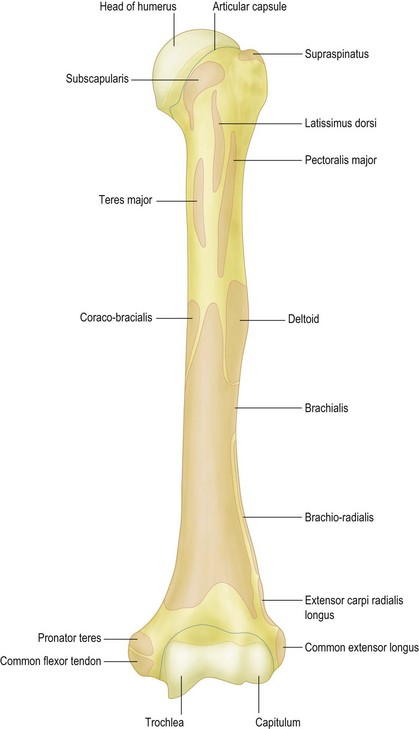
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.3 Fig. 207.
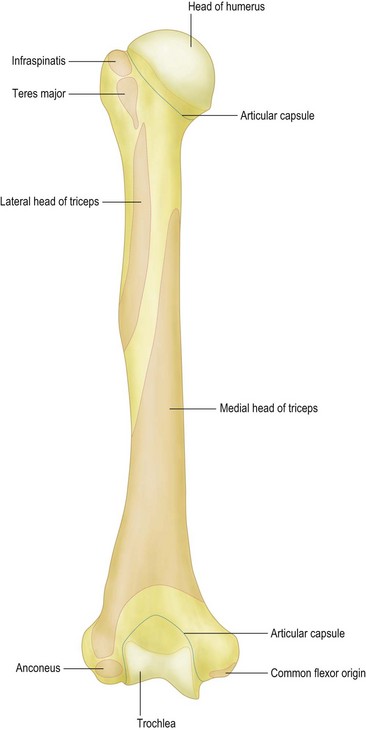
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.3 Fig. 208.
Two indentations on the anterior side of the humerus prevent impingement of the coronoid process and the radial head during flexion: the coronoid fossa is located medial to the smaller radial fossa. The olecranon fossa is located on the posterior side to allow space for the olecranon during extension of the elbow (Fig. 2.2).
The lateral epicondyle forms the capitellum. This is hemispheric in shape and articulates with the concave head of the radius. It is separated from the trochlea by a groove, which articulates with the rim of the radial head throughout flexion/extension and pronation/supination. The trochlear–capitellar articular axis is oriented approximately 5–7° internally rotated in relation to the humeral epicondyles; in addition, this axis has an approximately 6–8° valgus tilt in relation to the humeral axis.1 The capitellum is oriented anteriorly and cannot therefore be observed when the elbow is visualized posteriorly. When fixing transverse distal humeral fractures it allows the application of a plate more distally on the posterior side of the lateral column. The distal part of the humerus is angulated 30° anteriorly, such that the centres of the two condyles are collinear with the anterior humeral cortex on a lateral radiograph.
Ulna
The olecranon is the subcutaneous portion of the ulna and therefore the most prominent bony surface landmark of the elbow (Figs 2.3–2.5). It forms the trochlear notch (incisura semilunaris) on its anterior side with the coronoid process, a protuberance that demarcates the articular surface anteriorly. This coronoid process can fracture during dislocation of the elbow. The trochlear notch forms an arc of approximately 190°. While most of this articular surface is covered with cartilage, there is an area in the centre where either the cartilage is thin or absent. This is a normal finding and should not be interpreted as osteochondral damage. It is, however, a safe area through which an olecranon osteotomy can be performed. The shape of this notch is elliptical, with a longitudinal ridge articulating with a deeper portion of the trochlea. This affords bony stability.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 213.
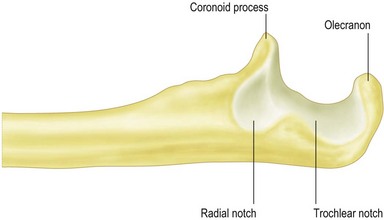
Figure 2.4 Left ulna, lateral view.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 212.
Redrawn with permission of http://www.graysanatomyonline.com, Elsevier Ltd. Chapter II. Osteology. 6a.4 Fig. 214.
The long axis of the ulna and the humerus determines the overall carrying angle of the elbow. Studies report a valgus angle ranging from 11° to 14° in men and from 13° to 16° in women.2
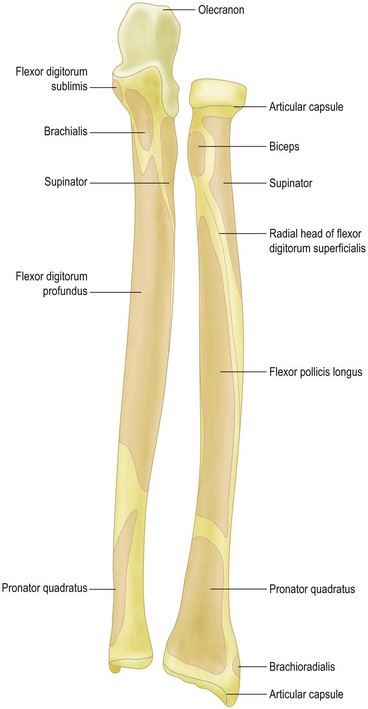
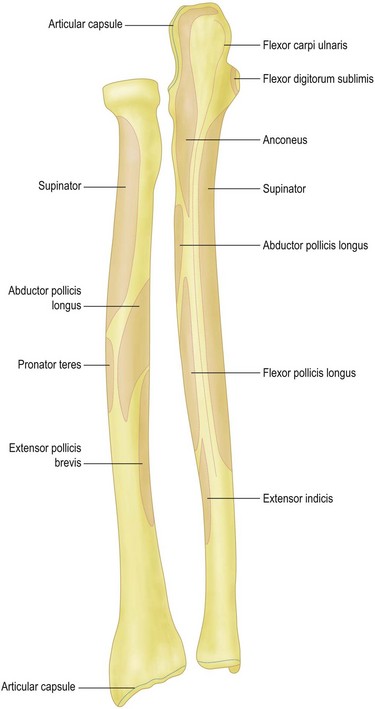
Radius
The radial head is shaped like a concave disc and is attached to the radial shaft by the radial neck (Figs 2.3 and 2.5). The proximal end articulates with the capitellum and the circumferential surface articulates with the lesser sigmoid notch. Therefore not only is the proximal end covered with articular cartilage but also a 280° arc about the circumference. The 80° arc that remains uncovered can be used to place screws in case of displaced radial head fractures. The angle between radial head and shaft is 13°. The radial head is not a perfect circle and is variably offset from the axis of the neck. This has important implications for reconstruction of the radial head.3,4 On the anteromedial side just distal of the radial neck lies the bicipital (also called radial) tuberosity: a bony tuberance into which is inserted the biceps tendon.5,6
Articulations
The elbow is one of the most congruent joints in the body. As mentioned before, there are three articulations in the elbow: ulnohumeral, radiohumeral (or radiocapitellar) and proximal radio-ulnar joint. The elbow has been called the trochleogingylomoid joint: the ulnohumeral is a hinge (ginglymus) joint that allows flexion and extension and the radiohumeral (or radiocapitellar) and proximal radio-ulnar joint are trochoid joints, allowing axial rotation or pivoting.1 The radial head and the ulna articulate during pronation and supination of the forearm at the proximal radio-ulnar joint.
Clinical Pearl 2.1
Capsuloligamentous anatomy
Joint capsule
The three elbow joints are surrounded by a joint capsule. The capsule attaches along the articular margin of the elbow. It includes the olecranon, the coronoid and radial fossae, but not the humeral epicondyles. On the anterior side of the elbow, it originates above the coronoid and radial fossae and inserts distally onto the anterior border of the coronoid and the annular ligament on the lateral side (Figs 2.1, 2.2, 2.3 and 2.5). Distal to the radial annular ligament, the joint capsule forms a recess to allow rotation of the radius. The posterior part attaches above the olecranon fossa proximally and distally along the medial and lateral articular margins of the greater sigmoid notch. Medial and lateral collateral ligaments reinforce the capsule.
Fat pads
Fat pads lie within the joint capsule in the coronoid, radial and olecranon fossae. These can become displaced from their respective fossae by intra-articular fluid accumulation. This displacement of the intra-articular fat pads results in positive radiographic fat pad signs.7
Medial collateral and the lateral collateral ligament complexes
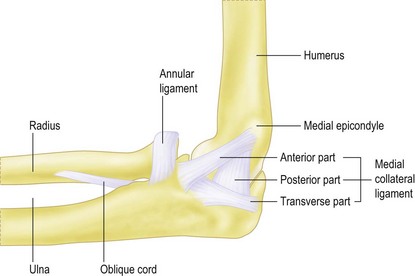
The medial collateral ligament consists of an anterior and a posterior bundle. In between lies a transverse ligament (Fig. 2.6). The anterior bundle is the primary restraint to valgus stress. It originates on the central two-thirds of the antero-inferior aspect of the medial humeral epicondyle. The anterior bundle inserts at the base of the coronoid on average 18 mm posterior from the tip. The width of its origin averages about 10 mm and involves 67% of the epicondyle In the coronal plane.8,9 Knowledge of the insertion sites is clinically important: for example, when medial epicondylectomy is being performed, only 20% of the epicondyle can be removed without violating the origin of the anterior medial collateral ligament. Also, its deep origin allows elevation of the flexor tendons off the medial epicondyle without detaching the ligament. The posterior location of the insertion site prevents damage to the ligament from fractures of the tip of the coronoid, although it does become detached with fractures at the base of the coronoid. The mean length of the anterior bundle is about 27 mm, with a width of 4–5 mm. Some studies have also shown that the anterior medial collateral ligament can be subdivided into anterior and posterior bands. These bands demonstrate a different tension in various positions of the elbow, due to a ‘cam effect’.10 Finally, some authors claim a third central portion which remains isometric throughout elbow movement. The latter can be used as a guide for ligament reconstruction.11 This deep bundle runs from 5 mm anterior to the distal tip of the medial epicondyle to the most prominent part of the sublime tubercle on the ulna. The posterior bundle of the medial collateral ligament inserts slightly posterior to the anterior medial collateral ligament and fans out along the base of the greater sigmoid notch. It has an average width of 8 mm and a thickness of 4–8 mm. The function of this ligament is to restrain valgus stress, especially during flexion.1,10,12
Microscopic evaluation has revealed distinct collagen bundles within the capsular layers. The anterior bundle has an additional ligament complex superficial to the capsular layer confluent with the flexor muscle mass.13
Four distinct bundles comprise the lateral collateral ligament complex: the lateral ulnar collateral ligament, the radial collateral ligament, the annular ligament and the accessory lateral collateral ligament (Fig. 2.7). It is a key stabilizer for varus stress and posterolateral stability.
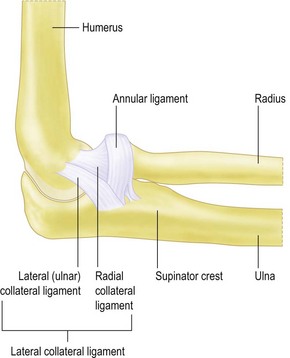
Figure 2.7 Lateral collateral ligament complex.
Reprinted with permission of Lockard L, J Hand Ther.20
The ulnar insertion of this ligament complex varies, being described as either a broad insertion blending the lateral and annular ligaments, or as being bilobed with more distinct insertions.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree