Chapter 28 Pathogenesis and Classification of Elbow Stiffness
Introduction
Motion of the elbow is important for positioning the hand in space. While the shoulder places the hand on the surface of a sphere of space, the elbow can change the radius of that sphere.1 Forearm motion can help position the hand for the most effective manipulation of the environment and is particularly important for tool use. Unfortunately, shoulder and wrist motion have a limited ability to compensate for stiffness of the elbow and forearm. Morrey et al. demonstrated that most activities of daily living can be performed within a 100° elbow flexion arc from 30° to 130° of flexion and a 100° rotation arc from 50° of supination to 50° of pronation; however, small contractures can affect specific functional tasks.2 The elbow is prone to stiffness after injury, but congenital abnormalities, degenerative and inflammatory diseases, and neuromuscular problems can contribute to loss of mobility.
Pathogenesis
Osseous and articular anatomy
The elbow is one of the most congruent, and constrained synovial joints in the body, providing both intrinsic osseous stability as well as a relatively large range of motion. With the evolution from quadrapedal to bipedal locomotion, enhanced stability of the ulnohumeral articulation has led to the upper limb becoming less adapted for weight-bearing and more adapted for tool use and dexterity. Ultimately, the hominid elbow developed articulations that can tolerate little distortion without losing either stability or motion.3
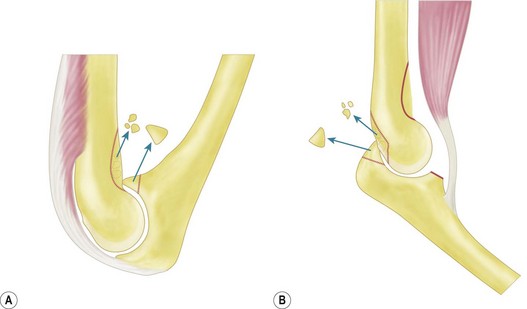
Distortion of the coronoid, radial and olecranon fossae of the distal humerus are common reasons for stiffness. These fossae accommodate the structures for which they are named at the extremes of elbow motion. Implants, scar tissue, fracture callus, malunion, or ectopic bone can obstruct these fossae and thereby limit motion.4 Similarly, malunion of the structures that fit into the fossae can cause stiffness (Fig. 28.1).
Loss of the anterior translation/angulation of the articular surface of the distal humerus can limit elbow flexion. This translation facilitates elbow flexion by allowing clearance of the coronoid with respect to the humeral diaphysis as well as providing space for the muscles and soft tissues when the elbow flexes.1
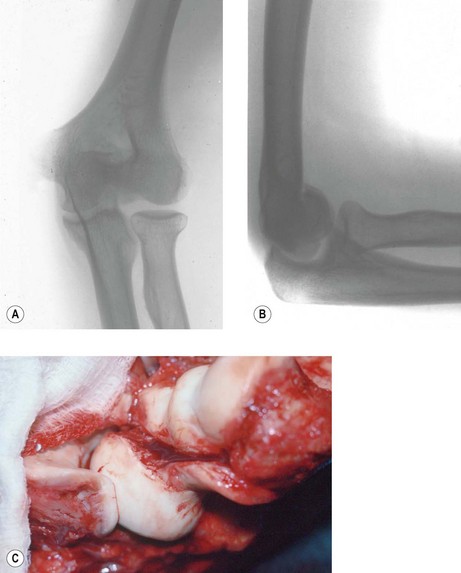
Incongruity of the articular surface (including slight subluxation) is a known contributor to loss of motion via arthrosis in the long term, but can also limit elbow motion acutely. This is particularly true for malunited fractures of the radial head, which can limit forearm rotation and malunited fractures of the capitellum and trochlea, which can limit flexion and extension (Fig. 28.2).4–6 Malunion of the coronoid leads to subluxation of the ulnohumeral joint, and progressive arthrosis and loss of motion.7 Arthrosis is limited after a simple olecranon fracture, perhaps because the fractures typically occur in a relatively non-articular portion between the coronoid and olecranon articular facets.
Soft tissue contracture
The aetiology of soft tissue contracture about the elbow is multifactorial and incompletely understood. The elbow has the largest capsular capacity in 70° of flexion and any intra-articular effusion, some believe, will cause the patient to assume this elbow position to decrease pressure and pain.8 The capsule responds by thickening, further limiting motion9 (Fig. 28.1B).
In animal models, ligament and capsular trauma has been shown to lead to increased levels of transforming growth factor β and increased numbers of myofibroblasts that have intrinsic contractile properties.10,11 Other changes include increased collagen cross-linking and decreased water content that manifests as thickened and less compliant tissue.12
Musculotendinous units can contribute to stiffness by either limiting excursion or adhering to bone. After trauma and immobilization, both the elbow flexor and extensor musculature will co-contract and be less elastic. In rat models, sarcomere shortening was seen after only 1 week of immobilization.13 Additionally, direct muscle injury may play a role by starting the inflammatory response cascade with possible upregulation of a growth factor that contributes to ectopic ossification around the elbow.14,15 Lastly, spasticity of muscles about the elbow can be seen after central nervous system injury. Electromyography (EMG) studies in head injury patients have shown the elbow flexors to be more spastic than the extensors, which might contribute to flexion contracture.16,17 However, despite all of this research data, the exact pathogenesis remains unclear.
Although contracture of the skin is rarely a problem after closed trauma, it can be a major factor after suffering thermal burns (Fig. 28.3) and may be relevant in congenital aetiologies such as pterygium cubitale where cutaneous webs may create contractures.18 The elbow is the second most common contracture in burn patients, second only to contractures of the shoulder.19
Heterotopic ossification
The elbow is particularly predisposed to HO, but most HO around the elbow does not contribute appreciably to loss of motion. HO is most commonly associated with direct trauma to the elbow and may correlate with its severity: HO is seen in 3% of simple elbow dislocations and up to 20% of fracture elbow dislocations.20,21 Additionally, HO is associated with neural axis trauma with formation seen below the level of spinal cord injury, specifically on the side of hemiplegia.22 The greatest risk, however, is seen in patients with concomitant head and elbow trauma with up to 80% developing HO.23 Thermal injury, organ transplantation, early surgical insult and forced manipulation may also predispose the elbow to HO formation.24
The mechanism of formation of this amorphous bone is believed to involve pluripotent cells that come from the surrounding muscle and differentiate into osteoblasts. Though incompletely understood, trauma and inflammation may start this process. Immature heterotopic bone contains woven bone and mineralized bone surrounded by fibroblasts and skeletal muscle cells.25 Mature heterotopic bone is identical to other lamellar bone but is more metabolically active and does not have a true periosteal layer. This picture is consistent with the hypothesis that myositis ossificans represents fibrous replacement of muscular hematoma, though it has not been reproduced in animal studies.26 Most of the heterotopic bone in the elbow that forms after trauma, severe burns, or central nervous system injury forms between the capsule and muscle.27 Attempts to isolate systemic inductive factors in closed head trauma patients has been unsuccessful to date.1,15
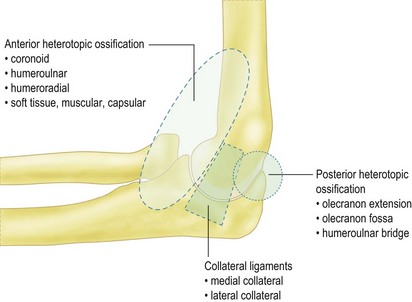
Classification of heterotopic ossification
HO can be classified by either its anatomical appearance or its functional effect (Fig. 28.4). In our experience, HO is most commonly seen posteromedially in burn patients and sometimes encases the ulnar nerve. HO can, however be seen in all anatomical distributions about the elbow in these patients and in patients with central nervous system injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree