Subtrochanteric Fractures
George Haidukewych
Key Points
Introduction
Subtrochanteric fractures occur in the proximal femur between the inferior aspect of the lesser trochanter and a distance extending about 5 cm distally. These fractures generally occur in two patient age distributions: the young, polytraumatized population from a high-energy injury, and the osteopenic older population, usually following a low-energy fall from a standing height.1,2 The subtrochanteric region of the femur is one of the most highly stressed zones in the human skeleton, and tensile or compressive stresses can exceed several multiples of body weight. The frequently short proximal fragments are deformed by the hip flexors and abductors, which may make accurate reduction and fixation challenging. Internal fixation strategies for managing these fractures fall into one of two categories: intramedullary fixation or some form of plating. Many specific challenges must be overcome to ensure stable proximal fragment fixation performed in a biologically friendly manner while accurate alignment and implant position are attained.
Indications/Contraindications
Surgical stabilization is the treatment of choice for subtrochanteric fractures in adults. Internal fixation and early patient mobilization to avoid the negative impact of prolonged recumbency are preferred. Although plates such as the angled blade plate or proximal femoral locking plates can be useful for unusually “short” proximal fragments, intramedullary techniques should be considered the preferred stabilization strategy because of their mechanical superiority and biologically friendly implantation methods. Several studies have demonstrated clinical superiority of nails versus plates. Although a detailed analysis of each of these studies is beyond the scope of this chapter, the reader is referred to extensive references on this subject at the end of this chapter for further reading.
Preoperative Planning
For young patients, attention should be focused on prioritization of treating life-threatening injuries using standard Advanced Trauma Life Support (ATLS) protocols. The fractured limb is examined with careful circumferential examination of the skin to rule out an open fracture. The neurovascular status of the limb should be documented. Elderly patients are medically optimized preoperatively.
Radiographic Evaluation
Quality anteroposterior and lateral radiographs provide enough information to guide treatment of the vast majority of subtrochanteric fractures. The length of the proximal fragment and the diameter of the diaphysis distally should be evaluated. A traction view may be helpful in defining fracture geometry and location, if the initial views are unclear. Any proximal fracture extension into the piriformis fossa or greater trochanter, or involvement of the lesser trochanter, can influence the choice of implant. If any concern is raised about fracture extension into the piriformis fossa or the greater trochanter, a computed tomographic scan can be obtained; however, the author finds these rarely necessary. Several classifications exist for subtrochanteric fractures; however, the author finds the Russell-Taylor method the most useful. The Russell-Taylor classification3 (Fig. 46-1) may guide the surgeon in determining the integrity of the proximal fragment, which historically has facilitated decision making regarding nail or plating choices. The classification is divided based on whether the piriformis fossa is involved and whether the lesser trochanter is involved. Previously, this information would guide decision making regarding standard locking of an intramedullary nail from greater to lesser trochanter or the need for so-called reconstruction nailing with cephalomedullary-type fixation. In the past, piriformis fossa extension proximally required plating techniques because surgeons were concerned about losing capture of the proximal fragment during a nailing using a piriformis fossa starting point; the nail could “fall out the back” of the proximal fragment.1,4 With more contemporary nailing techniques that enter the tip of the greater trochanter, these issues have become less problematic. The common theme for all the various classification schemes proposed is that fractures are classified based on the integrity of the proximal fragment. With modern nailing techniques, however, these classifications no longer influence a “nail versus plate” decision, but may influence the locking configuration. Typically, a standard greater to lesser trochanter locking screw configuration can be used for one-piece proximal fragments, and cephalomedullary locking is used for more complex proximal fragment involvement (Figs. 46-2 through 46-4).
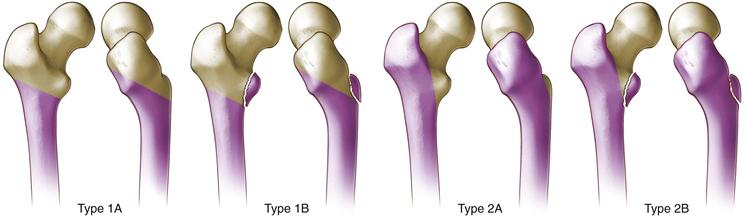
Figure 46-1 Russell-Taylor classification of subtrochanteric fractures of the femur. (Redrawn from Russell TA, Taylor JC: Subtrochanteric fractures of the femur. In Browner BD, Jupiter JB, Levine AM, Trafton PG [eds]: Skeletal trauma, vol 2, Philadelphia, 1992, Saunders, pp 1490–1492.)

Figure 46-2 Postoperative radiograph of proximal fragment fixation with an intramedullary nail.

Figure 46-3 Segmental subtrochanteric fracture in a young polytraumatized male.

Figure 46-4 Postoperative radiograph after reduction and intramedullary fixation.
Description of Technique of Intramedullary Nailing of A Subtrochanteric Fracture
The author prefers to position the patient supine on a fracture table with the involved leg in a traction boot and the other leg placed in the lithotomy position. The use of a fracture table greatly facilitates obtaining a clear proximal-lateral fluoroscopic radiograph, especially in heavy patients, and allows the surgeon to fine-tune the reduction, leg length, and alignment and hold the leg in place during the nailing procedure. Some have advocated the lateral position to facilitate starting point location and reduction by flexing the distal fragment to align with the proximal fragment deformity. This may be of benefit in heavier patients. The lateral position, however, may not be practical in polytraumatized patients. In general, a percutaneous approach is used for nailing. The author prefers to take a guide pin and place this along the skin laterally, proximal to the greater trochanter, to determine the appropriate nail trajectory and skin entry site to obtain entry into the tip of the greater trochanter. Once this trajectory is known, a stab incision is made in the proximal gluteal area. The incisions required to get the appropriate trajectory can be deceptively proximal. An incision is made in the proximal gluteal area, and a guide pin is placed down to the tip of the trochanter. The author prefers to treat these fractures with a starting point in the tip of the greater trochanter. The guide pin is placed into the tip of the trochanter or just a few millimeters medially.5 It is very important not to start even a little lateral to the tip of the trochanter, because this will tend to move the starting point farther laterally with canal preparation and may result in excessive varus of the proximal fragment. The guide pin is placed in the proximal fragment, and the appropriate starter reamer is passed using soft tissue protection sleeves. The guide pin is placed across the fracture.
For “low” (more distal) subtrochanteric fractures that have some intact diaphysis, reduction tools can be used to assist with guide wire placement. These maneuvers are useless if the proximal fragments are short and have large, capacious, osteopenic canals. Appropriate measurements are taken. It is important to avoid running the reamers until the reamer head is well inside the proximal fragment. This will avoid excessive reaming of the starting hole, which can lateralize the entry angle (the starting hole can become an oval). Reaming is performed, and the nail is inserted in the usual fashion. The author selects a nail 1 to 2 mm smaller than the reamer that provided first “chatter” in the diaphysis. Nail length is chosen based on surgeon preference. The author routinely uses long nails and locks them statically distally. Locking screw fixation is placed into the femoral head or neck or into the lesser trochanter based on the indications already discussed. True lateral fluoroscopic projections are used to guide center-center placement of cephalomedullary fixation. In reality, the author typically chooses some form of cephalomedullary fixation for these fractures, because it is difficult to rule out any proximal fracture extensions, and fixation of the femoral head and neck essentially avoids any potential problems with nail containment. Most modern nailing systems allow standard (“greater to lesser trochanteric”) or cephalomedullary locking with the same implant.
A “high” subtrochanteric fracture should never be reamed in an unreduced position. If the patient is positioned on the fracture table and significant deformity is still noted in the proximal fragment after gentle traction is applied, then the author typically will attempt some simple percutaneous technique to try to reduce the proximal fragment. This can involve a ball spike pusher placed from anterior to posterior, some form of joystick such as a Schanz pin placed in the lateral cortex, or, more commonly, a percutaneous clamp placed through a very small incision over the lateral femur. The proximal fragment is then reduced, moving it into an extended position, an adducted position, and an internally rotated position relative to its unreduced position. This “reversal” of deforming forces essentially moves the tip of the greater trochanter (or piriformis fossa) into an ideal position to gain access for a starting point, and a starting point can be made in an accurate fashion (Fig. 46-5A and B). Many different instruments can achieve the reduction; however, the author prefers a percutaneous clamp because it can be repositioned easily (unlike a Schanz pin) and typically will not slip easily (as a ball pike pusher will do). Additionally, a clamp typically does not require an assistant to constantly hold it in a reduced position. If one reams the fracture in an unreduced position, it will remain unreduced after the nail is passed because there is no reduction effect of passing the nail, unlike the situation when a diaphyseal femoral fracture is reamed. This typically results in a proximal fragment that is left in varus, external rotation, and flexion—a difficult deformity to manage. It is also important to note that small incisions to improve reduction should not be equated with large incisions with excessive stripping, evacuation of the fracture hematoma, and broad blunt retractors used to reduce the fracture under direct vision. This is not recommended because it will devitalize the tissues and may contribute to nonunion. Cerclage cables generally should be discouraged; however, they occasionally can be useful for supplemental fixation of long spiral or long oblique patterns because nailing these patterns can often leave them distracted. The entire construct is checked fluoroscopically under biplanar evaluation to ensure that excellent fixation and appropriate implant position and length are achieved. The distal femur is evaluated fluoroscopically, especially in the lateral view, in elderly patients with osteopenia and bowed femoral shafts to make sure no distal nail penetration of the cortex occurs anteriorly. The wounds are then irrigated and closed in layers in the usual fashion.


Figure 46-5 A and B, Typical flexion, abduction, and external rotation deformity of the proximal fragment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








