33 SUBSTANCE ABUSE AND TRAUMA CARE
The use of mind-altering (psychoactive) substances has been a part of the human experience for thousands of years. Historical evidence indicates that opium has been used medicinally for at least 3,500 years and cannabis is mentioned in writings in ancient China and India. Many references are made to alcohol consumption in various early societies and accounts of problems related to the use of alcohol and other substances can be found in the Bible and in ancient Egyptian hieroglyphics.
The total economic cost of alcohol and other illicit drug abuse (not including nicotine) has been estimated to be more than $300 billion per year, with more than half the cost attributed to alcohol. The cost of underage drinking alone has been estimated to be in the order of $53 billion annually spent on the consequences of alcohol-related crashes, drownings, fires, suicide attempts, violent crimes, fetal alcohol syndrome, and treatment for alcohol use disorders.1 More important, in addition to monetary costs, the less tangible emotional cost to the affected individuals and their families and friends is incalculable.
TERMINOLOGY AND CLASSIFICATION
Addiction is the term commonly used synonymously for drug or alcohol dependence. The American Society of Addiction Medicine (ASAM) defines addiction as a primary, chronic, neurobiologic disease with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving.2
The Diagnostic and Statistical Manual of Mental Disorders IV–Text Revised (DSM IV-TR)3 classifies substance-related disorders into two categories: (1) substance use disorders and (2) substance-induced disorders. The substance use disorders are divided into substance abuse (Table 33-1) and substance dependence (Table 33-2). According to the DSM-IV-TR, “the essential feature of dependence is a cluster of cognitive, behavioral, and physiological symptoms indicating that the individual continues substance use despite significant substance-related problems.” This diagnostic scheme places a heavy emphasis on the effect that the substance use has on an individual’s life, not just the presence or absence of physiologic dependence. An individual can meet criteria for dependence without having physical dependence, and a person with only physical dependence does not necessarily meet criteria for dependence. Thus the cancer patient on high doses of opioids for pain but with no signs of impairment or uncontrolled use would not be diagnosed with opioid dependence. Because physical dependence is not necessarily required, a qualifier of “with physiologic dependence” or “without physiologic dependence” is used.
TABLE 33-1 Criteria for Substance Abuse
Reprinted with permission from American Psychiatric Association: Diagnostic and statistical manual of mental disorders, 4th ed, text revision, Washington, DC, 2000. Copyright © 2000, American Psychiatric Association.
TABLE 33-2 Criteria for Substance Dependence
Reprinted with permission from American Psychiatric Association: Diagnostic and statistical manual of mental disorders, 4th ed, text revision, Washington, DC, 2000. Copyright © 2000, American Psychiatric Association.
The World Health Organization’s (WHO) International Statistical Classification of Diseases and Health Related Problems, Tenth Revision has a category “dependence syndrome” that is similar to the DSM-IV-TR diagnosis of dependence. It does not include a category “abuse” but does include “harmful use,” which is different than DSM-IV-TR abuse in that it focuses on mental and physical health and specifically excludes social impairment. The WHO also uses the term “hazardous use” to describe an individual who is at risk for adverse consequences from substance use.4
The National Institute on Alcohol Abuse and Alcoholism adds other terms for the purposes of screening for alcohol use problems (see assessment considerations below). “At-risk drinking” is used to describe a person who exceeds recommended alcohol consumption levels (more than 14 drinks per week or four drinks per occasion for men, more than seven drinks per week or three drinks per occasion for women) but does not meet DSM-IV-TR criteria for alcohol abuse or dependence.5 “Problem drinking/use” is a term often used to indicate problems related to substance use that do not meet criteria for abuse or dependence. “Substance misuse” is another term used to describe the use of a prescribed medication in a manner not prescribed for that individual.
SUBSTANCE USE AND INJURY EPIDEMIOLOGY
The Substance Abuse and Mental Health Services Administration reports that approximately half of all Americans aged 12 years or older report having consumed alcohol in the month before the survey (126 million U.S. residents). Approximately 22.7% engaged in at least one episode of binge drinking, defined as consumption of five or more drinks on one occasion (i.e., at the same time or within a couple of hours of each other). Further, 6.6% (or 16 million persons) were estimated to be heavy drinkers (five or more drinks per occasion on 5 or more days in the previous 30 days).6
The same survey found that an estimated 7.8% of the U.S. population aged 12 years or older (approximately 19.7 million people) used an illicit drug in the month before the interview. There were an estimated 136,000 current heroin users, 2.4 million current cocaine users, and 14.6 million current marijuana users. As for the nonmedical use of prescription medications, an estimated 4.7 million reported nonmedical use of pain relievers, 1.8 million tranquilizers, 1.1 million stimulants, and 0.27 million sedatives. Additionally, 71.5 million Americans, 29.4% of the population, use tobacco.6
In 2005, an estimated 10.5 million persons reported driving under the influence of an illicit substance during the previous year. This corresponds to 4.3% of the population aged 12 years or older. The rate was highest (13.4%) among young adults aged 18 to 25 years, a decrease from 14.7% in 2002.6 It is important to point out that all the above figures are likely to be underestimates because this survey does not include homeless persons who do not use shelters, military personnel on active duty, and individuals institutionalized in prisons or hospitals.7
Underage drinking continues to be a huge problem in America, to the point that it has been identified as one of the main areas of focus for the Healthy People 2010 initiative.8 It has been associated with negative effects on academic performance and increases in teenage pregnancy, risky sexual behavior, sexual assault, acquaintance rape, delinquency, unintentional injury, and death. Initiation of drinking before the age of 14 years is also associated with an increased risk of lifetime alcohol abuse or dependence.9 It is estimated that approximately 20% of all alcohol consumed in the United States is consumed by minors, who spend an estimated $22.5 billion on alcoholic beverages.10
ALCOHOL AND TRAUMA
Studies of patients from trauma centers and university hospitals have reported alcohol and psychoactive drug use rates from 25% to 60%.11–15 The National Safety Council estimates that in the United States there is an average of one injury every 2 minutes involving an alcohol-related crash.16 There are well-documented relationships among increasing blood alcohol concentration (BAC) and level of impairment in cognition and motor coordination, likelihood of injury, and severity of injury. Intoxicated patients in one study were shown to have significantly higher Injury Severity Scores than those not intoxicated, and within groups, those at the higher end of the range had correspondingly higher BACs.17 Habitual drunken drivers have an increased risk of dying in an alcohol-related crash.18
Alcohol abuse has been associated with all types of injuries. Studies evaluating mechanism of injury and alcohol use have reported that 32% to 47% of motor vehicle crash (MVC) victims had positive BACs.12 Rates of positive BAC for injured motorcyclists were comparable at 33% to 39.3%.19,20 The risks associated with walking under the influence of alcohol are underappreciated. The reported incidence of positive BACs among injured pedestrians treated in trauma centers is 31% to 49%.12,21 Alcohol also plays a major role in intentional interpersonal violence. Sixty-one percent of firearm homicide victims in one study were intoxicated22 and 31% of the intentional injury victims from another had positive BACs.12 Alcohol has also been linked to 30% of fire fatalities, 48% of drownings, and a tenfold increase in deaths from boating incidents.23–25 It is also associated with a significant number of bicycle crashes.26
A number of researchers have investigated the incidence of alcohol dependence among trauma patients. Rivara et al21 determined that 75% of acutely intoxicated trauma patients have positive scores on the Short Michigan Alcohol Screening Test and that 25% to 35% of them had biochemical evidence of chronic alcohol use. Soderstrom et al27 found that 54% of acutely intoxicated trauma patients could be diagnosed as alcohol dependent, along with 11% of trauma patients who had negative BACs.27
Alcohol is present in nearly one third of injured adolescents, a population for whom alcohol is an illegal substance. Studies of adolescent trauma patients found that 20% to 30% tested positive for alcohol or other drugs at the time of admission.28,29 MVCs are the leading cause of death for 16- to 20-year-olds in the United States. The National Highway Traffic Safety Administration reports that in 2005, 5,699 drivers in this age range were killed in MVCs with an additional 432,000 injured; alcohol was involved in 21% of these.30 The National Survey on Drug Use and Health reported that 8.3% of 16- to 17-yearolds and nearly 20% of 18- to 20-year-olds reported driving under the influence of alcohol in the past year.6
Research remains inconclusive regarding whether alcohol intoxication results in less favorable outcomes after trauma. Although animal studies have documented alcohol’s adverse effects on degree and outcome of injury,31 such results are inconclusive in humans.32,33 Studies of trauma patients from Level I trauma centers demonstrated no increased risk of complications from acute intoxication15,34 but found a twofold increase in risk of complications in patients with behavioral and biochemical markers of chronic alcohol abuse. Some researchers have suggested that the more severe outcomes seen in patients with a positive BAC are the result of correlates of alcohol use such as high speed and not using seat belts.33 Hospitalization costs and length of stay are substantially higher for drinking drivers than for those who had not been drinking.34 Alcohol intoxication is a significant risk factor for sustaining traumatic brain injury and may impair rehabilitation and recovery.35
OPIATES AND TRAUMA
The incidence of positive opiate tests in patients admitted to urban trauma centers has been reported to be 5% to 16%.13,14,36 A prospective study of patients treated at a regional trauma center conducted from 1984 through 1998 documented a 531% increase in the number of patients who tested positive for opiates.36 An Australian study of injection heroin users found that more than 50% of the subjects reported having driven soon after using heroin or other opioids in the preceding month and that a third had had a crash related to their drug use.37
STIMULANTS AND TRAUMA
Cocaine use may be an underreported cause of trauma. Studies of trauma patients have demonstrated cocaine usage rates from 6% to 22%.13,14,38 A study of New York City fatalities (persons aged 15 to 44 years) found that 26.7% tested positive for cocaine metabolites. Two thirds of the cocaine-positive fatalities were the result of homicides, suicides, traffic collisions, or falls, making fatal injury after cocaine use among the top five causes of death.38 Soderstrom et al36 documented a 242% increase in the number of trauma patients who tested positive for cocaine between 1984 and 1998.
Methamphetamine is also associated with increased trauma and increased length of hospital stay.39 Because of the caustic nature of the chemicals involved, the manufacture of methamphetamine can lead to significant burn and inhalational injuries.40
MARIJUANA AND TRAUMA
Although several studies in Level I trauma centers have documented rates of 21% to 35% positive toxicology for tetrahydrocannabinol, the main psychoactive chemical in marijuana,13,14,41 there is no consistent evidence demonstrating marijuana use as being causative. One study found that the higher rate of traffic incidents in marijuana users is likely reflective of characteristics of the young users rather than the effects of cannabis use on driving performance.42 Another study found that patients who tested positive for marijuana had an additional length of hospital stay that averaged 1.3 days.11
ETIOLOGY OF SUBSTANCE USE DISORDERS
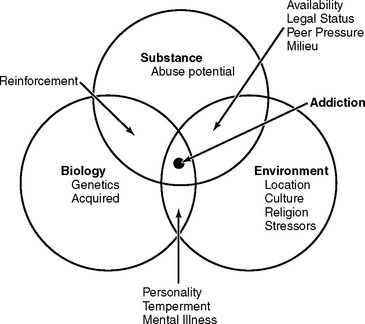
Substance use disorders are complex phenomena with biologic, psychologic, social, and cultural determinants (Figure 33-1). Current etiologic theories emphasize the role of genetic influences, learned behavior, neurobiology, and environmental stressors. It appears that environmental influences along with a genetic predisposition is required for the development of addictive behaviors.43–45
Familial, twin, and adoption studies all indicate that genetics contributes approximately 50% of the risk for development of substance use disorders.44–50 Genetics appears to influence susceptibility to most categories of illicit drugs, with heroin showing the strongest influence.49–51 Children of parents with alcohol dependence have an increased incidence of alcoholism compared with the children of nonalcohol-dependent parents. Males appear to be more susceptible to genetic influence than females, although female children of alcoholics appear to have an overall higher incidence than the general population.52 One study found that sons of alcohol-dependent parents have less intense subjective and physiologic reactions to ethanol.53
Animal studies have detected physiologic differences between levels of neurotransmitters and receptors in alcohol-preferring and non-alcohol-preferring animals.54,55 In humans the dopaminergic and serotonergic systems of the brain are implicated in susceptibility to addiction, although causative links to specific genotypes have not been found.56,57
Environment also plays an important role in substance use and substance use disorders. Reactions to psychoactive drugs are determined in part by the user’s mental state before use and the environment or setting in which the use occurs. Studies comparing alcohol- and non-alcohol-preferring mice have induced alcohol-preferring behavior in the non-alcohol-preferring mice by subjecting them to environmental stressors.43 In humans, heroin use among Vietnam veterans followed a similar pattern.58 The majority of veterans who began using heroin while overseas stopped after they returned to the United States and the extreme stressors were removed.
Abusive environments in early childhood may be a substantial risk factor for later drug abuse through a complex interaction between the child, the environment, and the level of social support.59,60 A majority of patients in drug and alcohol treatment programs report being victims of childhood physical or sexual abuse.61
Various psychiatric conditions share a strong associated comorbidity with substance use disorders. These include schizophrenia, bipolar disorder, depressive disorders, anxiety disorders, posttraumatic stress disorder, the cluster B personality disorders (antisocial, borderline, histrionic, narcissistic), and attention deficit hyperactivity disorder.62,63
PHARMACOLOGIC, PHYSIOLOGIC, AND CLINICAL EFFECTS OF PSYCHOACTIVE DRUGS
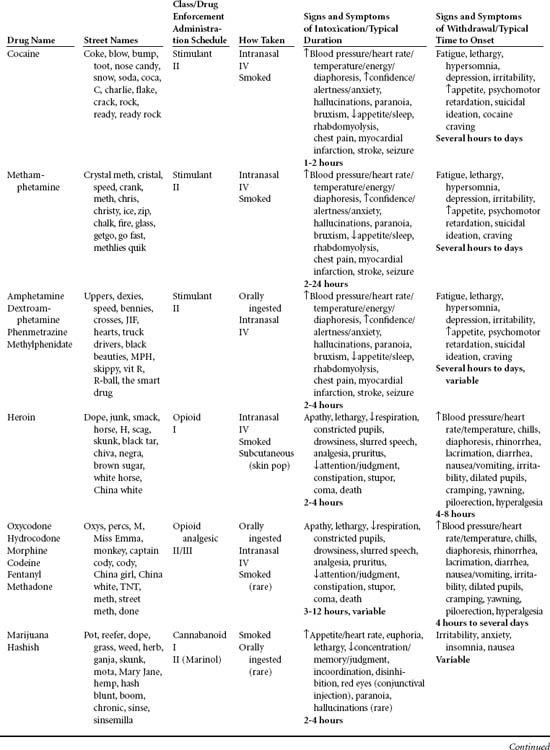
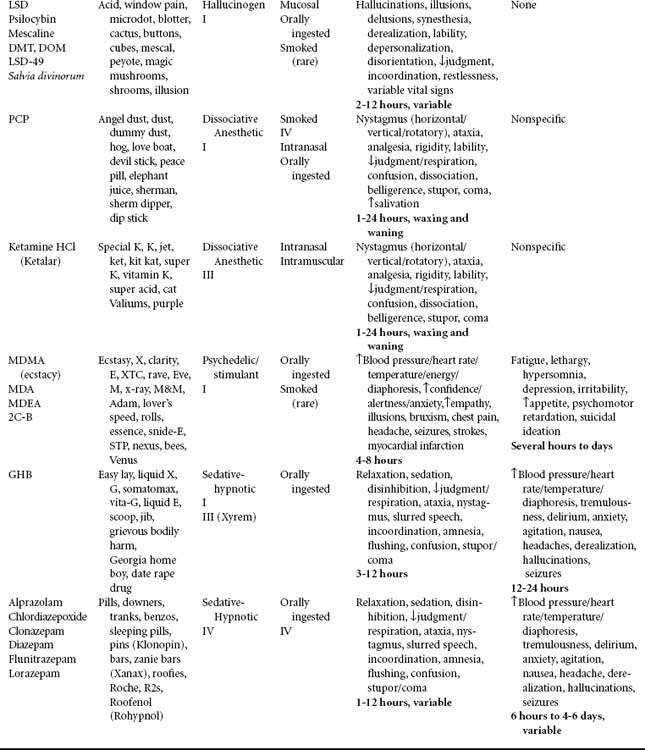
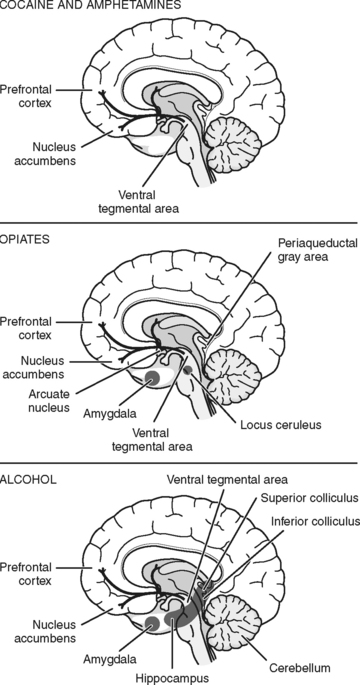
Psychoactive drugs (Table 33-3) generally exert their mood-altering effects by altering levels of neurotransmitters within the brain through a complex series of interactions among various transmitter systems. The release of one neurotransmitter may result in the release of a second neurotransmitter or direct stimulation of a receptor site, which may enhance or block neurotransmitter function. Either the direct or the secondary action can be responsible for the clinically evident psychoactive effects.64 These actions can prolong the effects of a given neurotransmitter, increase neurotransmitter release, or block receptor response to a neurotransmitter. This results in the various analgesic, hallucinogenic, stimulant, anxiolytic, or depressant effects, determined to some degree by the area of the brain containing the affected neural pathways. The reinforcing effects seen with most substances of abuse are felt to be related to a final common dopaminergic pathway involving the nucleus accumbens and ventral tegmental area (Figure 33-2).
TOLERANCE AND PHYSICAL DEPENDENCE
Withdrawal (or acute abstinence syndrome) is defined as the physical or psychologic disturbances that occur after the cessation or reduction in use of a substance to which the body has developed tolerance. It is marked by a fairly predictable (for a given class of drugs) constellation of signs and symptoms after the abrupt discontinuation of, or rapid decrease in, the dosage of a psychoactive substance. The acute abstinence syndrome for a given drug is typically an exaggerated response that is the opposite of the drug’s clinical effects.65
ALCOHOL AND CENTRAL NERVOUS SYSTEM DEPRESSANTS
Pharmacokinetics
Most of the alcohol consumed is metabolized in the liver by the enzyme alcohol dehydrogenase and to a lesser degree by the microsomal enzyme system.66 It is converted into acetaldehyde and then rapidly converted into acetyl coenzyme A, which can then be oxidized through the citric acid cycle or used in various anabolic reactions involved in the synthesis of cholesterol, fatty acids, and tissue constituents. This enzymatic step is the rate-limiting portion of the metabolic process. The metabolism of ethanol differs from that of most substances in that the rate of oxidation of ethanol remains relatively constant and is minimally affected by the ethanol concentration. The typical rate of ethanol metabolism is 0.3 to 0.5 ounces per hour. A “standard drink” (1.5-ounce shot of 80-proof liquor, a 5-ounce glass of wine, or 12 ounces of beer) contains about 0.6 ounces of ethanol. Women have lower levels of gastric alcohol dehydrogenase than men. This results in less alcohol being broken down in the stomach and more alcohol being absorbed by the stomach and reaching the peripheral circulation.67
Mechanism of Action
γ-Aminobutyric acid (GABA) is the primary inhibitory neurotransmitter in the CNS. Alcohol exerts its depressant effect primarily by binding with the GABA receptors of the brain. Alcohol shares this action with other CNS depressants, most notably benzodiazepines and barbiturates. Alcohol and other CNS depressants bind to different portions of the GABAA receptors and modulate their primary function of altering chloride influx through the ion channels of the cell.68 Chloride increases the resting membrane potential, hyperpolarizing the cell and rendering it less reactive.69
Alcohol also has a suppressant effect on the glutamate (NMDA) receptors within the CNS. NMDA receptors are excitatory, and suppression of the excitatory function results in further depression of the CNS. The reversal of these effects during acute alcohol withdrawal is thought to be responsible for the clinical manifestations of CNS hyperactivity.70 Alcohol’s action on glutamate receptors is thought to play a role in alcoholic blackouts and acute withdrawal seizures as well.70–72
Alcohol also has effects on the endorphin,73 serotoninergic,74 and dopaminergic75 systems within the brain, effects that are somewhat different from those of other CNS depressants. The stimulation of the endorphin system may account for alcohol’s weak analgesic effect. Patients sustaining minor injuries may not complain of pain until after their BAC has dropped. Stimulation of the dopaminergic system is thought to be responsible for the euphoric and reinforcing effects of alcohol. Findings also suggest that serotonin may mediate alcohol-seeking behavior in habituated individuals.56
Pharmacologic Effects
Central Nervous System.
As previously described, the clinical manifestations of CNS depressant intoxication are directly related to the drug’s effects on the CNS. The earliest effect of alcohol ingestion is to alter judgment, causing the drinker to become disinhibited and to behave uncharacteristically (e.g., laugh or talk loudly, become boisterous or argumentative). These manifestations appear with a BAC in the range of 50 to 150 mg/dl. As the blood level of the alcohol rises, cerebellar and vestibular functions become affected. Nontolerant individuals with a BAC in the 150 to 300 mg/dl range display significant motor symptoms, manifesting in slurred speech and an unsteady, ataxic gate. At still higher levels, they may become stuporous and eventually lose consciousness. At levels higher than 400 to 500 mg/dl, respiration can become impaired and the individual may become comatose. Protective gag and cough reflexes may be lost. BACs of 500 mg/dl or more can be fatal.76 Although behavioral and physiologic responses to increasing BAC occur in a fairly predictable fashion in the nontolerant individual, the level producing impairment will vary considerably in the tolerant individual. A BAC of 400 mg/dl, which would produce stupor in the uninitiated drinker, may result in minimal obvious impairment in the alcohol-dependent individual.
Other CNS effects of chronic alcohol use include alcoholic cerebellar degeneration, alcoholic dementia, and central pontine myelinolysis. Cerebellar degeneration is characterized by gait ataxia and mild degrees of limb impairment. The lower extremities are more commonly involved than the upper extremities. It can improve with adequate nutrition and abstinence from alcohol.
Cardiovascular System.
Alcohol has multiple effects on the cardiovascular system. Acute alcohol intoxication results in mild increases in heart rate along with depressed contractile function, increases in left ventricular end-diastolic pressure, decreased rate of left ventricular pressure development, and slowed relaxation time. The resultant decrease in cardiac reserve may have detrimental effects on the trauma patient. Acute alcohol intoxication has been shown to potentiate the physiologic and metabolic derangements accompanying hemorrhagic shock and may contribute to secondary brain injury as a result.77–79 Acute intoxication decreases myocardial responsiveness to several inotropic agents, including dobutamine, isoproterenol, and phenylephrine.80,81
Respiratory System.
Ethanol taken by itself has minimal respiratory depressant effects at levels of 200 mg/dl. Associated respiratory effects include a decreased responsiveness to carbon dioxide and slight reduction in vital capacity and expiratory reserve volume as BAC increases. In nondependent drinkers, respiratory arrest has been associated with BACs of 400 to 500 mg/dl. Studies indicate that alcohol increases pulmonary vascular resistance after soft tissue injury and may increase the risk of posttraumatic acute respiratory distress syndrome (ARDS).66
Hematologic System.
Long-term alcohol consumption can result in both folate deficiency and iron deficiency anemia.66 Alcohol also depresses bone marrow and vacuolizes red blood cell precursors. The alcoholic patient can present a challenge because multiple types of anemia may be present simultaneously.
Alcohol also interferes with the production and function of platelets. Long-term alcohol use may cause thrombocytopenia from decreased megakaryocyte production. Even brief periods of drinking can alter platelet function.82
Digestive System.
Alcohol produces toxic effects on several areas of the digestive tract. Many of these pathologic alterations have implications in the care of the trauma patient. Esophageal irritation from alcohol and regurgitation of acidic gastric contents result in esophagitis. Mallory-Weiss tears may occur from repeated episodes of vomiting, and esophageal varices are associated with alcoholic cirrhosis. Excessive alcohol ingestion may damage the gastric mucosa, causing chronic gastritis. Patients are also at risk for acute hemorrhagic gastritis.66
Alcohol is inherently hepatotoxic and can injure the liver in the absence of any nutritional deficiencies. Fatty infiltration of the liver is the first manifestation of hepatotoxicity and can begin after a few days of heavy alcohol consumption. This is followed by fibrosis, which sometimes manifests as alcoholic hepatitis.66 Eventually the fibrosis may progress to necrosis and inflammation, resulting in cirrhosis. The early fatty infiltration is reversible with cessation of drinking, but the latter stages of fibrosis are irreversible.
Alcohol interferes with the cytochrome P450 enzymatic system in the liver. Short-term alcohol use can impair the function of this system, consequently slowing the metabolism of drugs dependent on the system. This slows the rate of drug elimination, resulting in higher serum levels of agents metabolized by this pathway. In contrast, long-term use of alcohol may increase the rate of activity of the P450 system. Drugs are then more rapidly metabolized, resulting in lower-than-predicted serum concentrations.66
Trauma patients may have hepatic dysfunction significant enough to interfere with hemostasis through coagulopathy from impaired production of vitamin K–dependent clotting factors in the liver. Although serum transaminases may be elevated in liver disease, the prothrombin time is the most sensitive indicator of hepatic dysfunction.83
Long-term alcohol use can produce a form of chronic pancreatitis associated with irreversible structural and functional alterations in the pancreatic tissue. Episodes of acute pancreatitis can occur as well, with classic symptoms of midepigastric pain, nausea, vomiting, and anorexia, along with associated elevations of serum amylase and lipase.66 Some patients have pathophysiologic changes associated with chronic pancreatitis although they remain asymptomatic.84 Serum enzyme levels are often normal in individuals with subacute forms of pancreatitis. Diarrhea can develop from malabsorption syndromes caused by a loss of pancreatic exocrine secretions.
OPIATES
Opiates are drugs derived from the poppy plant, Papaver somniferum. Opioids are synthetic compounds that resemble the chemical structure of the naturally occurring substances. Morphine and codeine are naturally occurring opiates found in the resin of the poppy plant seed pod. Heroin (diacetyl morphine) is a semisynthetic compound that has undergone processing after being extracted from raw opium gum. Meperidine, oxycodone, hydromorphone, and methadone represent synthetic formulations. Naturally occurring opiates are the enkephalins, dynorphins, and endorphins, peptide molecules produced in the CNS and found in the brain, spinal cord, and exocrine glands.85
Opiate drugs can be ingested, injected subcutaneously (“skin popping”) or intravenously (IV), or inhaled either nasally or by smoking. Heroin, the most commonly abused opiate, historically has been injected IV. However, because of increased purity of heroin, use through intranasal and smoked (“chasing the dragon”) routes has increased. Rate of absorption, onset of action, and duration of action are dependent on the route of administration and the half-life of the particular drug used.85
Pharmacology
Stimulation of opiate receptors, of which three subtypes (μ, δ, and κ) have been identified, results in the familiar analgesic effects of these drugs.85 The overall effects of opiate neurotransmitters on the CNS include decreased awareness of and distress from pain, drowsiness, mental clouding, and, at higher doses, euphoria. The level of euphoria depends to some degree on which agent is used, the dose, and the route of administration. Clinically significant tolerance can occur with patients who have been on opiates for as few as 7 days.
There is also a group of synthetic drugs that possess both partial opiate agonist or mixed agonist/antagonist properties. They have analgesic actions similar to opiates when used alone but have antagonistic effects when used in conjunction with opiates.85 These compounds include pentazocine, buprenorphine, butorphanol, and nalbuphine. These drugs can precipitate acute withdrawal in the opiate-dependent patient.
Toxicity
Generally, opiates have little effect on the heart rate and blood pressure in the supine patient, although they produce some vasodilation that can result in hypotension in the volume-depleted patient.85 Adverse blood pressure and heart rate changes noted during administration of opiates may indicate that the patient requires further volume repletion.
Opiates can also cause adverse effects that impact the gastrointestinal and genitourinary systems. Opiate analgesics decrease gastric motility and can result in constipation and delayed or impaired gastric emptying. These drugs can cause nausea and vomiting as a result of a direct action on the chemoreceptor trigger zone of the medulla. Urinary retention is another possible adverse effect of opiates. Opiate-dependent patients typically develop tolerance to the respiratory depressant and emetic effects of opiates.85
COCAINE AND AMPHETAMINES
Pharmacokinetics
Cocaine hydrochloride is a derivative of the coca plant, Erythroxylon coca. There are basically two chemical forms of cocaine—hydrochloride salt and free base. The hydrochloride salt is a white powder that is water soluble and can be injected IV or snorted intranasally. Free base cocaine is processed by mixing cocaine hydrochloride with an alkali (e.g., baking soda) and water. This alkaloidal form of cocaine (crack) is more volatile at a lower temperature than the hydrochloride form, which allows it to be smoked. Regardless of which route is used for administration, cocaine enters the circulation rapidly. Once in the blood, it binds with plasma proteins and is rapidly transported to the CNS.86 Some of the drug remains unbound or free, this being the active portion of the drug. The onset of action for cocaine is variable, with IV and inhaled administration causing an almost immediate increase in blood pressure and heart rate. Peak effects occur 30 minutes after intranasal administration and are generally less intense but more prolonged than with the other routes. Cocaine is metabolized primarily in the liver and excreted by the kidneys.
Pharmacology
Cocaine acts on both the peripheral and central nervous systems. It blocks the reuptake of norepinephrine (NE) in the periphery. In the CNS, cocaine inhibits the reuptake of dopamine and causes central sympathetic activation. CNS outflow and the resultant increase in circulating NE are responsible for the signs and symptoms of sympathetic nervous system hyperactivity.87 Cocaine’s psychologic effects are caused by its blockade of dopamine reuptake within the CNS. The heightened sense of mental acuity, euphoria, and decreased fatigue associated with cocaine use are the result of the effect of excessive dopamine on the nucleus accumbens. The cocaine “high” is short lived, lasting 1 to 2 hours with nasal inhalation, 30 to 40 minutes with IV administration, and 5 to 10 minutes if smoked.86
Cocaine use can result in the rapid development of tolerance to the euphoric effects; however, only partial tolerance develops to the cardiovascular effects.87 There is some degree of cross-tolerance with other CNS stimulants. Long-term cocaine users have decreased numbers of dopamine receptors in their CNS, which may account for the depression seen during withdrawal from cocaine. Some users of cocaine also experience sensitization in which they experience increasing effects at lower doses of the substance.
Toxicity
Cocaine’s detrimental physiologic effects occur primarily during periods of active use. Toxic effects of cocaine are most commonly seen in its actions on the cardiovascular system. Increases in heart rate and blood pressure peak early during a binge and return to baseline despite continued increases in the serum cocaine level. Excessive NE can lead to generalized vasoconstriction, tachycardia, arrhythmias, mesenteric ischemia, and myocardial infarctions.88–90
Adverse effects of cocaine on the neurologic system include cerebrovascular accidents (CVA), seizures, and altered mental states. Cocaine use has been associated with altered cerebral perfusion and ischemic and hemorrhagic CVA, often in young persons with no known risk factors for cerebral vascular disease, although some cocaine-induced CVAs can be linked to underlying cerebrovascular abnormalities.91,92 Patients with cocaine-induced seizures typically have one generalized seizure after cocaine use by the IV route. These patients usually have unremarkable neurologic diagnostic workups after the seizure, although further workup to rule out traumatic brain injury is still warranted. The causes of cocaine-induced seizures remain unclear. Mental status changes associated with cocaine use range from anxiety to acute psychosis. Psychosis associated with cocaine use is typified by paranoid ideation, delusions, hallucinations (often tactile, called formication), and hypersensitivity to environmental stimuli.
Inhaled or smoked cocaine also has detrimental effects on the bronchial mucosa and ciliary-mucus clearance mechanisms. Alveolar macrophage function is impaired and ciliary clearance mechanisms are effectively paralyzed by the use of crack.93
Cocaine and ethanol are often used together and appear to form a unique compound, cocaethylene. Experimentally, this combination of drugs has resulted in increased cardiac toxicity in selected individuals.94 Heart rate increases with coadministration of cocaine and alcohol were significantly greater than those with either drug used alone.95
Methamphetamine
Methamphetamine is a CNS stimulant with physiologic and psychologic effects much like those seen with cocaine. Its euphoric effects are also the result of increased dopamine in the CNS, although this occurs by a slightly different mechanism than with cocaine. It can be ingested orally, snorted, injected IV, or smoked. Effects are felt 3 to 5 minutes after inhalation and 15 to 20 minutes after oral ingestion. Unlike cocaine, however, the effects of methamphetamine last from 6 to 24 hours. Psychologic effects include increased attention, euphoria, decreased fatigue, paranoia, hallucinations, and mood disturbances. Hyperthermia and seizures have been associated with acute methamphetamine use.96
NICOTINE
Physiologic Effects
The physiologic effects of nicotine include vasoconstriction and tachycardia as a result of catecholamine release from direct action on the adrenal medulla. Stimulation of CNS receptors results in tremor, and actions on the chemoreceptor trigger zone cause nausea or vomiting. Parasympathetic stimulation of the gastrointestinal tract by nicotine results in increased gastrointestinal motility. Digestive tract responses to nicotine include nausea, vomiting, and diarrhea, the latter as a result of the effect of nicotine on receptors in the large bowel.97
Psychologic Effects
Nicotine acts directly on nicotinic cholinergic receptors of the CNS. This stimulation in turn causes a release of dopamine within the mesolimbic system of the brain, which is thought to account for the pleasurable sensations induced by nicotine.64 Nicotine has both stimulant and depressant activities, which account for its reported paradoxic effects. Use of nicotine decreases subjective levels of anxiety, alters mood, and subjectively increases concentration.97
MARIJUANA
Marijuana is the common name for the dried flower buds, stems, and leaves of the Cannabis sativa plant. The drug is usually smoked but can be ingested. Δ-9-Tetrahydrocannabinol (Δ9-THC) is the major psychoactive ingredient in the plant, although more than 400 cannabinoids have been identified. The highest concentration of cannabinoids is in the resin of the plants’ flowering tops, where concentrations are five to ten times higher than the amounts found in the leaves.98 Hashish, or hash, is the dried resin collected from the plant tops.
Two types of endogenous receptors for Δ9-THC have been identified. Anandamide is a naturally occurring lipid neurotransmitter that has both peripheral and central activity.99,100 It binds with the cannabinoid receptor sites in the CNS.101
Pharmacokinetics
When marijuana is inhaled, Δ9-THC is absorbed rapidly into the bloodstream. Initial metabolism takes place in the lungs and liver. Although the pathway is similar for that of orally ingested marijuana, there is a more gradual increase in the Δ9-THC level over a period of 4 to 6 hours. This results in a delay in the onset of psychoactive effects. The peak serum levels of Δ9-THC are higher with oral ingestion than are those resulting from smoking.101
Because Δ9-THC is highly lipophilic, it is released slowly from the CNS and other lipid-rich tissues, resulting in a prolonged half-life. Half-life can vary from 18 hours to 4 days. Δ9-THC is converted into inactive metabolites in the liver and is excreted in the urine and feces.98
Physiologic Effects.
Cannabis use impairs gross and fine motor functions and delays reaction time. Despite these effects, no clear link has been established between cannabis use and vehicular crashes or fatalities.98 One reason is that cannabis users may tend to overestimate their degree of impairment and compensate by increasing their attention to driving, whereas drivers under the influence of alcohol tend to underestimate their degree of impairment.102,103 Acute marijuana use impairs short-term memory, impairing the ability to learn. These effects can persist up to 24 hours after smoking marijuana.104 Retrieval of previously learned material is largely unaffected. Effects of long-term cannabis use include impairment of organization and problems integrating complex information involving attention and memory.105 It is unknown whether these defects are permanent.
Long-term smoking of marijuana adversely affects the function of alveolar macrophages and alters the tracheobronchial epithelium.106 Pulmonary alterations from chronic use result in cough and sputum production similar to that observed in cigarette smokers.
Psychologic Effects
Marijuana induces a state of intoxication characterized by euphoria and relaxation. Psychic manifestations vary depending on user set and setting and can include heightened awareness of the external environment, drowsiness, increased hunger, and depression. At levels producing moderate intoxication, it adversely affects a wide range of behaviors, including simple motor tasks and complex psychomotor and cognitive tasks.107 Higher levels may induce panic, paranoia, and anxiety. Rarely, it may be associated with psychosis, usually in persons with underlying psychiatric disorders.
Although it was originally thought that marijuana use did not result in physiologic dependence, studies of long-term marijuana users have demonstrated sudden cessation after regular use of cannabinoids can cause a withdrawal syndrome.108 Tolerance can develop rapidly with regular marijuana use and sensitization has also been described.
RESUSCITATION PHASE
ASSESSMENT CONSIDERATIONS
Assessment of the substance-abusing trauma patient is complicated by several factors. As with any trauma patient, alterations in neurologic status as the direct effect of injury may obviate obtaining a medical history, including any information about substance abuse. Intoxicated patients may be stuporous and thus unwilling or unable to cooperate with history taking or physical assessment. Some trauma patients who are subjects of criminal investigations as a result of their injury or who are currently on probation or parole may give an inaccurate or incomplete history from fear of potential legal consequences. Further, it may be difficult to determine whether physical findings are the result of trauma or the substance abuse.109 It is imperative that complete assessment of the trauma patient be accomplished systematically and rapidly. Physical, historical, and laboratory findings consistent with substance abuse should be included in documentation of the physical examination and in the patient database.
Identifying the Patient with a Substance Abuse Problem
In light of the prevalence of substance use disorders in trauma patients and the emerging body of evidence that brief interventions are effective in reducing harmful drinking, the American College of Surgeons has recently adopted a recommendation that Level I and II trauma centers screen for substance use problems. In addition, Level I centers are expected to offer brief interventions for patients who screen positive for at-risk substance abuse. Despite the strong association between trauma and substance abuse, many trauma patients are still not screened for alcohol and other drug use.110
Trauma Database.
Substance-abusing trauma patients often have a history of previous injuries. Injury can be considered a symptom of substance abuse.111 Patients should be questioned about previous injuries, including falls, MVCs, assaults, and work-related injuries. Pertinent information can be obtained from family members if the patient is unable to provide information; the family can also be used to validate and supplement information received from the patient. Additionally, as much information as possible about the circumstances of the current injury episode should be collected from police officers, first responders, and other eyewitnesses at the scene. Reports of altered behavior or impaired judgment before or immediately after the injury can help identify the substance-abusing patient.
Physical Assessment.
Many of the sequelae of drug and alcohol use are manifested as alterations in the integument. Numerous bruises in various stages of healing over the lower extremities can be indicative of repetitive minor trauma caused by bumping into hard, fixed objects. Multiple small burns in various stages of healing are common as a result of dropping ashes while smoking. Abscesses and cellulitis are common integumentary manifestations seen with IV or subcutaneous drug injection. Patients who are using drugs IV often have “track marks,” lines of multiple injection sites along the course of peripheral veins. IV drug users may also have signs of phlebitis and sclerosis of veins. Patients occasionally display venous insufficiency caused by venous scarring, which may be seen in one or both upper extremities rather than in the lower extremities, as would be more common with other venous disorders. Patients may inject drugs subcutaneously (“skin popping”). These needle marks do not necessarily follow veins but are often found in fleshy parts of the body such as the thighs or upper arms. Intra-arterial injection of drugs has been associated with the development of aortic, iliac, and popliteal arterial thrombosis and arteriovenous fistulas or pseudoaneurysms.112,113
Drug use may result in respiratory depression and pathologic alterations in the upper and lower respiratory tract. Intranasal inhalation of cocaine often results in damage to the nasal mucosa and destruction of all or part of the nasal septum. This destruction results from the vasoconstrictive effects of cocaine and subsequent ischemia of the nasal mucosa and septum. Intoxicated patients and those using opiates may vomit and have aspiration pneumonia and the more severe consequence of ARDS. Alcohol-dependent patients may have chronic pneumonia as a result of frequent aspiration. Patients who smoke crack often have a cough productive of copious amounts of soot-stained sputum similar to that found in victims of smoke inhalation. Some patients who use drugs intranasally can have alterations in gas exchange related to various fillers and adulterants contained in the abused substance. Auscultation of breath sounds and observation of aspirated or expectorated sputum may provide evidence of inhalation drug use, chronic pneumonia, or other pulmonary conditions.114
Patients who use cocaine are susceptible to mesenteric ischemia or infarction and may have required exploratory laparotomy in the past. Patients sustaining blunt abdominal injury may have what appears to be an acute abdomen that cannot be distinguished between cocaine-induced ischemic injury and blunt hollow viscous perforation. A history of abdominal surgery in the cocaine-using patient should be explored carefully.115,116 Patients using alcohol or opiates may also have gastrointestinal symptoms, most commonly nausea, vomiting, constipation, and diarrhea. Alcoholic gastritis may cause acute mucosal lesions resulting in severe gastrointestinal bleeding. Chronic abdominal pain may result from pancreatitis, and patients may have hepatomegaly from cirrhosis or hepatitis.
Miosis, or pupillary constriction, is a common effect of opiates and occurs even in the tolerant user. Assessment of constricted, poorly reactive pupils may indicate recent opiate use.85 Care must be taken to rule out other causes for pupil findings. Conjunctival injection (i.e., red eyes) typically accompanies marijuana use. Marijuana also reduces intraocular pressure and decreases pupillary responsiveness to light, resulting in increased time for light accommodation.
Patients with recent cocaine use can have arrhythmias, hypertension, chest pain, cerebral vascular accidents, and electrocardiogram changes consistent with myocardial ischemia or infarction.117 Abuse of other psychoactive drugs may also cause adverse changes in heart rate and rhythm and blood pressure. Alcohol-dependent individuals may have secondary cardiomyopathy, and intravenous drug users frequently have bacterial endocarditis and subsequent valvular dysfunction.118 IV drug users and alcoholics may present with signs of congestive heart failure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree