Chapter 29 Sports Medicine
Sports medicine includes a rapidly expanding core of knowledge related to medical issues in sports and exercise for which the primary care sports medicine physician is uniquely trained. Primary care sports medicine is a subspecialty designation obtained through completion of an accredited sports medicine fellowship and passing the Certificate of Added Qualification examination. Many practicing primary care providers also gain vast experience in sports medicine through office treatment of orthopedic injuries, event coverage, and preparticipation screening evaluations. Musculoskeletal problems account for up to 20% of all primary care office visits (Urwin et al., 1998; Woodwell and Cherry, 2004), and approximately 90% of all sports injuries are treated nonsurgically. Thus, a sound clinical foundation in the evaluation and treatment of musculoskeletal disorders is critical to primary care providers and helps guide appropriate referral to orthopedic and rehabilitative specialists.
This chapter focuses on both the medical aspects of sports medicine and common orthopedic injuries in athletes. Detailed reviews cover the preparticipation physical evaluation, cardiac disorders in athletes, concussion assessment and management, cervical spine injuries, on-the-field assessment of the injured athlete, facial trauma, environmental influences such as exertional heat illness, common infections in athletes, and a systems-based review of dermatologic, pulmonary, hematologic, gastrointestinal, and genitourinary disorders in athletes. Orthopedic areas common in primary care sports medicine are also included, such as athletic low back pain, muscle strains, tendinopathy, shin pain, stress fractures, and issues unique to the pediatric or female athlete. See Chapters 30 and 31 for a comprehensive review of additional musculoskeletal problems relevant to sports medicine and the care of exercising individuals.
Preparticipation Physical Evaluation
A preparticipation physical evaluation (PPE), or “sports physical,” is frequently required for medical clearance before participation in organized sports. The Preparticipation Physical Evaluation monograph, first introduced in 1992, provides recommendations for the content and format of the evaluation (AAFP et al., 2005). The third edition of the monograph, updated in 2005, is supported by six national medical societies: American Academy of Family Physicians (AAFP), American Academy of Pediatrics, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, and American Osteopathic Academy of Sports Medicine. The fourth edition published in 2010 also includes collaboration with the American Heart Association (AHA) regarding the preparticipation cardiovascular evaluation.
The primary objectives of the PPE include the following:
Secondary objectives of the PPE include the following:
The PPE history focuses on symptoms related to exercise, such as exertional syncope, lightheadedness, chest pain, palpitations, dyspnea, wheezing, or fatigue with less than expected activity (Box 29-1). A past medical history of preexisting cardiac or pulmonary conditions, murmurs, hypertension, coronary artery disease risk factors, asthma, concussions, illicit drug use, prior orthopedic injuries, or other medical conditions that place an athlete at risk of injury should be noted. Specific questions to identify a family history of premature death, cardiovascular disease, and hereditary cardiac disorders, such as hypertrophic cardiomyopathy, Marfan’s syndrome, and long QT syndrome, are also recommended.
Box 29-1 Preparticipation Physical Evaluation (PPE): Cardiovascular History Questions
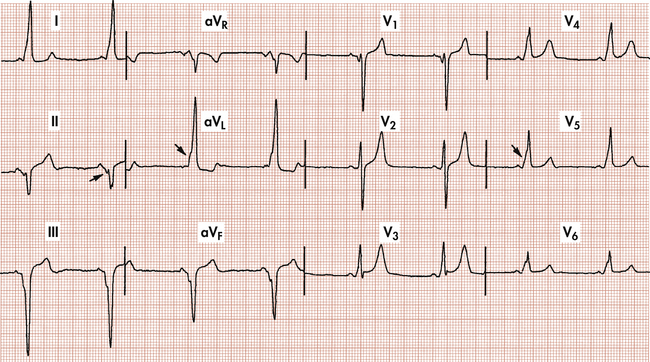
The PPE examination consists of both medical and musculoskeletal components. The cardiovascular examination is a major focus of the medical evaluation and consists of a blood pressure measurement, palpation of the radial and femoral artery pulses, cardiac auscultation with the patient both supine and standing, and recognition of the physical manifestations of Marfan’s syndrome (Maron et al., 1996b; Maron et al., 2007). Any heart murmur detected should be further assessed during the Valsalva maneuver or while moving the patient from a squatting to a standing position. These maneuvers decrease venous return and may accentuate the murmur of hypertrophic cardiomyopathy, the leading cause of sudden cardiac death in young athletes. However, hypertrophic cardiomyopathy is difficult to detect on examination alone because outflow tract obstruction, which causes the harsh systolic murmur, is present in only about 25% of patients with the disorder (Maron, 1997) (Fig. 29-1).
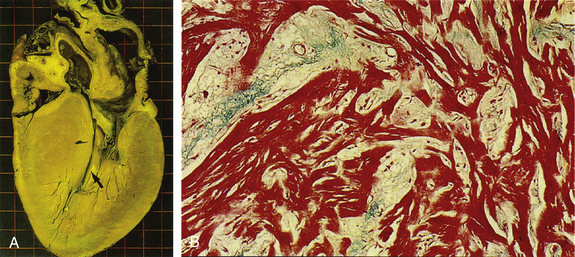
(From Braunwald E. Essential Atlas of Heart Diseases, 3rd ed. Philadelphia, Current Medicine, 2000.)
The musculoskeletal assessment serves as a screening evaluation of the spine and upper and lower extremities. Joint range of motion, strength, and stability should be tested. Several functional tests, such as hopping, squatting, and “duck walking,” assess many anatomic areas at once and make the evaluation more efficient. Previous orthopedic injuries can also be evaluated in more detail to detect problems that require further rehabilitation or protective bracing before sports participation.
Limitations of Cardiovascular Screening
Despite efforts to standardize the format and approach to the PPE, several limitations of the screening process still exist. In 2007, only 19% of U.S. states used forms that were considered adequate by AHA, and 35% of states allowed practitioners with limited cardiovascular training to perform the evaluation (Glover et al., 2007). Unfortunately, recommendations to use a comprehensive personal and family questionnaire to guide the PPE are not widely adopted, and recommended screening protocols are often incompletely or inadequately implemented. In addition, the PPE is screening for medical conditions that place an athlete at increased risk of sudden death, and no outcomes-based research has demonstrated that the PPE is effective in preventing sudden death or potentially catastrophic events, or for identifying athletes at risk. A complicating feature of the screening process is that athletes who harbor underlying structural heart disease may be asymptomatic until the sudden cardiac arrest. In a review of 134 cases of sudden cardiac death, only 18% of athletes had symptoms of cardiovascular disease in the 3 years before their death, and only 3% were suspected of having a cardiovascular condition after PPE (Maron et al., 1996a).
Cardiac Disorders in Athletes
Arrhythmias
Athletes with symptomatic Wenckebach block, such as presyncope or syncope during exertion, require further evaluation by a cardiologist and often placement of a permanent pacemaker and restriction of activities. Higher degrees of heart block, such as Mobitz II second-degree and complete third-degree AV blocks, are always pathologic in any individual, including athletes (Fig 29-2). Mobitz II and complete heart blocks signify marked disease in the His-Purkinje system and are generally accepted as a class I indication for permanent pacemaker placement, even in the absence of symptoms (Link et al, 2001).
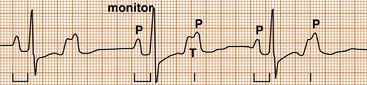
Figure 29-2 Mobitz II second-degree atrioventricular block. Note that every alternate P wave is blocked.
(From Goldberger E. Treatment of Cardiac Emergencies, 5th ed. Philadelphia, Saunders, 1990.)
Tachyarrhythmias in the athlete are abnormal and require further evaluation and treatment before participation in strenuous exercise. The treatment of many supraventricular tachyarrhythmias has been greatly advanced by the use of radiofrequency (RF) ablation, which might offer an actual cure and obviate the need for lifelong pharmacologic treatment.
Atrioventricular nodal reentrant tachycardia (AVNRT) is characterized by abrupt onset and termination of symptoms, a narrow QRS complex, and no evidence of atrial activity on the ECG during the tachycardia. AVNRT caused by an accessory bypass tract, known as Wolff-Parkinson-White (WPW) syndrome, may be evident on the ECG by the characteristic delta wave (slurred upstroke of QRS complex), short PR interval, and prolonged QRS complex (Fig. 29-3). Athletes with WPW may be at risk of sudden death and should be strongly considered for RF ablation. Radiofrequency ablation for both AVNRT and WPW offers cure rates higher than 95% (Link et al., 2001; Manolis et al., 1994).
Sudden Cardiac Death
Sudden cardiac death in athletes is a catastrophic event and the leading cause of death in exercising young athletes (Maron et al., 2009) The estimated incidence of sudden cardiac death in high school and college athletes is 1 in 100,000 to 200,000 athletes per year (Maron et al., 2009; van Camp et al., 1995). However, these studies are limited by the lack of a mandatory reporting system for juvenile sudden death and their reliance on electronic databases and media reports to identify cases of sudden death. Thus, current reports likely underestimate the true incidence of sudden cardiac death in athletes.
The cause of sudden cardiac death in young athletes (<35 years) is usually a structural cardiac abnormality, with hypertrophic cardiomyopathy and coronary artery anomalies representing 36% and 17% of U.S. cases, respectively (Box 29-2) (Maron et al., 2009). Commotio cordis, involving a blunt, nonpenetrating blow to the chest that leads to a ventricular arrhythmia, accounts for approximately 3% of cases. Commotio cordis is most common in younger athletes (mean age, 13 years) with compliant chest walls (Maron et al., 2002). Commotio cordis occurs most often in sports using a firm projectile, such as baseball, softball, hockey, and lacrosse, but can also occur from contact with stationary field equipment, the ground, or another player. In older athletes (>35), atherosclerotic CAD accounts for more than 75% of cases of sudden cardiac death.
Concussion in Sports
In 1966 the Congress of Neurological Surgeons proposed a consensus definition of concussion. Since then, both the definition and our understanding of concussion have been evolving. A concussion is defined as a traumatically induced transient disturbance in neurologic function, usually caused by a direct blow to the head, neck, or face (Aubry et al., 2002).
Symptoms and Incidence
A concussion usually results in the rapid onset of brief neurologic impairment that resolves spontaneously. Symptoms of concussion include loss of consciousness, amnesia, confusion, headache, vision problems, nausea, and balance problems (Box 29-3). A concussion may or may not be associated with a loss of consciousness. Over 90% of concussions are not associated with a loss of consciousness, and unconsciousness is not a marker of the severity of the injury (Lovell et al., 1999). Amnesia can include loss of memory of the events before (retrograde amnesia) or after (posttraumatic amnesia) the concussion, or both, and amnesia appears to be the best predictor of severity in athletic concussion (Collins et al., 2003). Conventional imaging studies such as computed tomography (CT) or magnetic resonance imaging (MRI) are normal in concussion, indicating that concussion is a functional rather than a structural injury (McCrory, 2001).
Return to Play
Most concussion guidelines designed to facilitate return-to-play decisions rely on loss of consciousness and the presence of amnesia to grade the severity of the concussion. This approach makes their usefulness limited because most sports-related concussions do not involve loss of consciousness or amnesia. Current recommendations suggest that management of concussion be based on symptoms and severity. The mildest concussion is one that involves transient symptoms that resolve quickly. More severe concussions involve persistent or prolonged symptoms and cognitive deficits on neuropsychological testing. Management of concussion includes both physical and mental rest, until all symptoms have cleared, and the neurologic examination, followed by a graded and stepwise program of exertion before return to sport (Box 29-4). Repetitive concussions, which take longer to return to baseline or that occur with progressively less trauma, are also considered of greater severity. Complex or recurrent concussions with persistent cognitive impairment, neurologic findings on examination, or prolonged symptoms may warrant advanced imaging and formal neuropsychological testing and should be managed by physicians with specific expertise in sports-related concussion.
Box 29-4 Graded Return to Play after Concussion∗
Modified from McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague, 2004. Br J Sports Med 2005;39:196-204.
∗ A player should never return to play while symptomatic from a concussion. In this supervised stepwise progression, the athlete can proceed to the next level if asymptomatic at the current level. If any postconcussion symptoms occur, the athlete should return to the previous asymptomatic level and try to progress again after 24 hours. Athletes with simple concussions may progress through these stages over several days. In cases of complex concussion, recovery is more prolonged.
Cervical Spine Injuries
KEY TREATMENT
Stingers
Stingers are always unilateral, a distinguishing feature from spinal cord injuries, which involve symptoms in multiple limbs. Athletes are safe to return to play when symptoms have fully resolved and the athlete can demonstrate full cervical ROM and a normal neurologic examination.
Catastrophic Cervical Spine Injury
On-the-Field Assessment
If transport is indicated, the athlete should be immobilized to a spine board. A supine athlete can be transferred to a spine board using a six-plus person lift technique, with one person responsible for stabilization of the head and neck (Inter-Association Task Force, 2001). To transfer an athlete who is facedown, a logrolling technique is recommended. Transport of a spine-injured athlete should be directed to a trauma center or medical facility with diagnostic and surgical capabilities for spinal injury.
KEY TREATMENT
Environmental Influences
Exertional Heat Illness
Heat stroke is the third leading cause of death in high school athletes (Lee-Chiong and Stitt, 1995). This is tragic because these deaths should be largely avoidable.
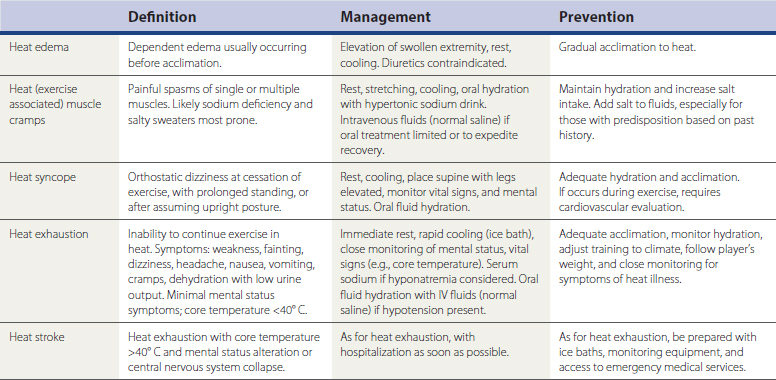
Heat illness is classified as heat edema, heat cramps, heat syncope, heat exhaustion, and heat stroke (Table 29-1) (Binkley et al., 2002; Eichner, 1998). Heat stroke is of the greatest concern, with hallmark features of an elevated core temperature higher than 40.5° C (105° F) and associated mental status changes. Any athlete exhibiting mental status changes and participating in an environment conducive to heat illness requires immediate removal from participation and active cooling. An ice-water tub should be prepared in advance if rapid cooling may be necessary in high-risk events, and an affected athlete should be fully submerged, with only the head above water (Smith, 2005). Other methods of cooling, such as applying ice bags to the neck, axilla, and groin, or using cold-water spray combined with fanning, can be effective, but the rate of core body temperature loss is slower than in ice-water immersion. Close monitoring of mental status and vital signs (e.g., core temperature) is indicated, and athletes should be transported to the hospital if they do not exhibit improving mental status with normalization of vital signs. The National Athletic Trainers’ Association Exertional Heat Illness Position Statement is an excellent reference regarding proper preparedness for heat illness (Binkley et al., 2002).
Exertional Hyponatremia
Exertional hyponatremia (serum sodium <130 mmol/L), once considered a rare complication of exercise in the heat, is now recognized as more common and responsible for a number of exercise-related deaths (Almond et al., 2005). Controversy surrounds the exact pathophysiology, but the condition develops in the setting of excessive hypotonic fluid replacement while sodium is progressively lost in sweat (Levine and Thompson, 2005; Noakes, 2002). Typical victims are relatively inexperienced female marathon runners who tend to be light sweaters, finish in over 4 hours, and drink copiously throughout the race. Nonsteroidal anti-inflammatory drugs (NSAIDs) taken before the race may be a contributing factor (Hsieh, 2004). Athletes with a history of exercise-induced hyponatremia do not seem to be predisposed to water overload at rest, although there may be some physiologic mechanism beyond pure water overload that accounts for the condition in some susceptible individuals (Speedy et al., 2001). Symptoms are similar to those of heat exhaustion, including weakness, dizziness, headache, nausea, vomiting, and cramping, but the headache is more prominent and progressively severe, extremity swelling may be noted, and progressive mental status changes occur despite a core temperature lower than 40° C (104° F). Cerebral edema underlies the mental status changes, and pulmonary edema may also occur.
Cold Injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree