Chapter 20 Allergy
The allergic patient differs from nonallergic patients in several ways (Box 20-1). The cause is unknown, but these abnormalities clearly are associated with abnormal cytokine production (Table 20-1). The result of these abnormalities is that allergic persons suffer from diseases such as allergic rhinitis and allergic asthma.
Box 20-1 Abnormalities Described in Allergic Patients
Table 20-1 Cytokine Production Abnormalities and Effects in Allergic Patients
| Cytokine | Effects |
|---|---|
| Increased production of IL-4 | Enhanced IgE production |
| Increased production of IL-13 | Enhanced IgE production |
| Increased production of IL-5 | Enhanced eosinophil activity and prolongation of the life of eosinophils |
| Increased production of IL-9 | Bronchial hyperreactivity |
Ig, Immunoglobulin; IL, interleukin.
The other important phenomenon to recognize is that the major allergic diseases (allergic rhinitis, allergic asthma, and anaphylaxis) are all increasing in incidence. The cause is unknown, but several hypotheses have been proposed. The hygiene hypothesis postulates that the rise in allergic disease is related to infection control in infants and children (e.g., through vaccination) and improved public health (e.g., through hygienic measures). Another hypothesis is that the allergic response is the same response used to defend against parasites. With a reduction in parasitic disease in more technically developed countries, a population has arisen that is free from exposure to parasites but still maintains a vigorous antiparasitic immune response that is aberrantly directed against the normally harmless organic substances such as pollen, animal dander, and food. Regardless of the mechanism, the burden of allergic disease in developed countries has increased rapidly since the 1970s.
Allergic Rhinitis
Treatment
Nonspecific Measures
Inhaled fungal allergens in fungus-sensitive subjects can produce seasonal symptoms during situations that promote fungal growth, such as humid and rainy weather and exposure to hay, mulch, commercial peat moss, and compost. Indoors, areas of spore formation can be identified at sites of water condensation such as shower curtains, window moldings, and damp basements. In addition, cool-mist vaporizers can serve as sources of fungal contamination.
Control of Symptoms
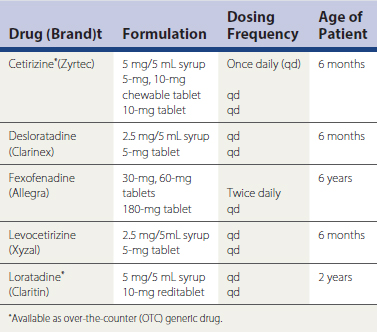
Antihistamines are effective for symptomatic control of allergic rhinitis, whether it is seasonal or perennial (Bousquet et al., 2008; Wallace et al., 2008; SOR: A). For optimal results, antihistamines should be used before exposure to the known allergen. Complete control might not be achieved when patients use antihistamines only sporadically. During the implicated season, around-the-clock administration provides maximal symptomatic relief. Because compliance is always an issue, the new second-generation antihistamines offer a convenient dosing regimen (Table 20-2). These groups of drugs, with specific binding properties, allow little to no penetration into the central nervous system (CNS), thus greatly reducing their side effects, primarily sedation. The second-generation antihistamines also have anti-inflammatory effects.
Topical intranasal glucocorticoids—beclomethasone, fluticasone, mometasone, triamcinolone, flunisolide, ciclesonide, and budesonide—are the most effective medication in the treatment of allergic rhinitis (Wallace et al., 2008; SOR: A). Their effectiveness is directly related to proper and daily use, posing problems with patient compliance. Side effects are related primarily to nasal dryness and epistaxis. Using saline as a moisturizer can relieve these side effects. The therapeutic effects are generally not immediate, and some patients must take these medications for 1 to 3 weeks before they achieve maximum benefit.
Specific Immunotherapy
KEY TREATMENT
Nonallergic Rhinitis
Allergy in the Eye
Conjunctivitis is the usual ocular reaction to airborne allergens. As in other forms of allergic inflammation, the mast cell plays a key role. Itching is the first symptom and may be associated with lacrimation. Dilation of the conjunctival blood vessels produces a “red” eye. Transudation of fluid through vessel walls results in edema of the conjunctiva, and exuded cells with increased glandular mucus secretions result in ocular discharge. In most atopic patients, conjunctivitis and allergic rhinitis occur together, but some patients are bothered only by eye symptoms. In contrast to other forms of conjunctivitis, the secretions contain eosinophils.
The usual therapy for allergic conjunctivitis is an oral antihistamine with a topical medication (Table 20-3). Cromolyn (Opticrom) and lodoxamide 0.1% (Alomide) are mast cell stabilizers. Topical H1 histamine blockers are also effective for treating allergic conjunctivitis. Ophthalmic histamine blocker solutions include emedastine (Emadine) and levocabastine (Livostin). Azelastine (Optivar), epinastine (Elestat), ketotifen (Zaditor, Claritin Eye, Zyrtec Itchy Eye) and olopatadine (Patanol, Pataday) are dual-acting drugs, preventing mast cell release and exerting antihistamine activity as well. Ketorolac (Acular) is a NSAID. Regular daily use is necessary to obtain maximum positive results with all topical agents. In severe cases and in vernal conjunctivitis, a soluble steroid such as fluorometholone ophthalmic solution (0.1%) is effective. The dose should be titrated to the minimum required to control symptoms. Use should be intermittent because glucocorticoids can lead to the development of cataracts, potentiate a secondary bacterial infection or a herpes simplex keratitis, and increase intraocular pressure. Steroid eyedrops should always be used under supervision by an ophthalmologist.
Table 20-3 Ophthalmic Solutions Useful in the Treatment of Allergic Conjunctivitis
| Drug (Brand) | Formulation | Dosage |
|---|---|---|
| Mast Cell Stabilizers | ||
| Cromolyn (Opticrom) | 4% | 1-2 gtt OU every 4-6 hr daily |
| Lodoxamide (Alomide) | 0.1% | 1 gtt OU qid |
| H1 Histamine Blockers | ||
| Emedastine (Emadine) | 0.05% | 1 gtt OU qid |
| Levocabastine (Livostin) | 0.5 mg/mL | 1 gtt OU bid |
| Combination Stabilizers/Blockers | ||
| Ketotifen (Zaditor) | 0.025% | 1 gtt OU bid 8-12 hr apart |
| (Zyrtec Itchy Eye) | 0.025% | 1 gtt OU bid 8-12 hr apart |
| (Claritin Eye) | 0.025% | 1 gtt OU bid 8-12 hr apart |
| Epinastine (Elestat) | 0.05% | 1 gtt OU bid |
| Olopatadine (Patanol) | 0.1% | 1 gtt OU bid 6-8 hr apart |
| (Pataday) | 0.2% | 1 gtt OU qd |
| Azelastine (Optivar) | 0.05% | 1 gtt OU bid |
| Nonsteroidal Anti-Inflammatory Drugs | ||
| Ketorolac (Acular) | 0.5% | 1 gtt OU qid |
OU, Each eye; gtt, drops; qid, four times daily; bid, twice daily; qd, once daily.
Asthma
The definition of asthma has undergone many changes over the years, but three elements are key to the diagnosis: reversible airway obstruction, airway inflammation, and increased airway responsiveness to a variety of stimuli. Physicians must remember that not all wheezing is asthma, and not all asthma has wheezing. Asthma is a chronic inflammatory disorder of the airways in which many different cells play a role. In patients with asthma, this inflammation causes breathlessness, chest tightness, recurrent episodes of wheezing, and cough, particularly at night. These symptoms are usually associated with variable airflow limitation that is partly reversible with treatment or sometimes spontaneously. This inflammation causes an associated increase in airway responsiveness to a variety of stimuli (Busse et al., 2007). Data from the Centers for Disease Control and Prevention (CDC) have shown an increase in the prevalence of asthma in the United States from 1980 to 2001. However, there has been no increase in mortality and hospitalization rates since 1997 (cdc.gov/asthma; see also Chapter 20).
Diagnosis
Because of the lack of any specific symptom or sign to define asthma by history or physical examination, some patients are mistakenly thought to have asthma. Numerous other diseases must be considered in the differential diagnosis of asthma (Box 20-2). Although parental history of asthma is present in half of children with asthma, the positive predictive value of this history ranges from 11% to 37% (Burke et al., 2003). The diagnosis of asthma should occur in three stages. First, suggestive symptoms referable to the chest with precipitating factors should raise the possibility of asthma. Second, further testing should be performed to confirm the diagnosis. Third, the patient should have symptomatic improvement with the appropriate asthma therapy (see Classification). When all the stages have been performed and meet the criteria, the diagnosis of asthma can be made.