7 Key Points 1. Performing the neurological examination at 72 hours following the injury provides a more accurate assessment and may be important with respect to therapeutic interventions and trials. 2. The greatest gains in motor skills occur in the first 3 months, with most recovery complete by 9 months; additional recovery, however, can also occur up to 12 to 18 months post-SCI. 3. The ASIA Impairment Scale (AIS) and ASIA motor scores are considered to be the best predictors of spontaneous recovery. Physicians and patients alike seek new and accurate information regarding the prognosis for recovery following a spinal cord injury (SCI). Having an awareness of the patterns of spontaneous recovery can help physicians in weighing risks and benefits and making treatment decisions regarding their patients with SCI. Accurate determination of injury severity and prognosis is important for proper planning of rehabilitation and allocation of appropriate resources. Recent studies reveal that a significant number of patients will spontaneously recover from SCI with no medical treatment at all.1 The American Spinal Injury Association (ASIA) Impairment Scale (AIS) and ASIA motor scores (see Chapter 6, this volume, for more discussion) are considered to be the best predictors of spontaneous recovery.2,3 Patterns of spontaneous recovery following SCI have become evident through analysis of the ASIA scores of control groups from recent SCI clinical trials.1 Additional information has been available from numerous databases, including the Model Spinal Cord Injury System (MSCIS) database and retrospective cohort studies. Ditunno, Waters, and Kirshblum have written a great deal regarding prediction of neurological recovery after SCI, and their work should be reviewed for more comprehensive examination of this topic.2,4–16 The neurological level of injury (NLI) is defined as the lowest level of the spinal cord that shows normal bilateral sensory and motor function. It is recognized that segments with normal function may vary by modality (motor function vs sensory) and body side (right vs left). Therefore, the four different segments can be classified as right-motor, right-sensory, left-motor, and left-sensory. Often, however, a patient’s NLI is designated by a single motor level and a single sensory level. The zone of partial preservation refers to segments below the level of injury in patients with complete injuries, where there is partial preservation of motor or sensory function. It is often difficult to perform an accurate neurological examination immediately following an injury because the patient has suffered “spinal shock” and may be sedated, in addition to various other reasons. It is generally agreed that performing the neurological examination at 72 hours following the injury provides a more accurate assessment and may be important with respect to therapeutic interventions and trials.11 Many of the early studies used either 72 hours to 1 week or 30 days for the initial examination.11,12 The timing of the exam is important because differences in motor and sensory scores from sequential neurological examinations are a predictor of the patient’s expected recovery (or deterioration). Various retrospective cohort studies have revealed key factors that predict spontaneous motor recovery. Of utmost importance is whether the injury was complete versus incomplete, the level of injury, initial strength of muscles in the first caudal level below the injury, and presence of pinprick sensation in the sacral segments. Empirical findings are discussed in this chapter as they relate to patients with complete tetraplegia, complete paraplegia, incomplete tetraplegia, and incomplete paraplegia. Additional predictors of spontaneous outcome after SCI, including motor-evoked potentials, somatosensory-evoked potentials, and conventional and diffusion tensor magnetic resonance imaging, have been discussed in detail in other chapters (see Chapters 43 and 46) and will not be discussed here. The greatest gains in motor skills occur in the first 3 months, with most recovery complete by 9 months; additional recovery, however, can also occur up to 12 to 18 months post-SCI.1 Patients with higher initial ASIA impairment scores (indicating a less severe injury) experience greater degrees and faster rates of motor recovery. The majority of motor recovery occurs within the first level below the ASIA motor level. Little or no recovery occurs at more than two spinal levels below the initial ASIA level.1,12 Studies show that recovery is faster and more complete in muscles that have retained a degree of voluntary function. The prognosis for muscles in the zone of partial preservation with no function is poor. Kirshblum et al. reviewed 5-year data on 987 patients from the 16 MSCIS locations and showed that, after 5 years postinjury, 94.4% with ASIA A scores initially remained ASIA A.3 Additionally, it was noted that 3.5% improved from ASIA A to ASIA B, 1.05% improved each from ASIA A to C and to D3 (Table 7.1). Data show that only 20% of patients who received initial ASIA A scores (complete SCI) experience some level of spontaneous recovery within the first year.1 Between 15 and 40% of patients with initial ASIA B scores converted to ASIA C status, up to 40% of patients with initial ASIA B scores converted to ASIA D status, and 60 to 80% of patients with initial ASIA C scores converted to ASIA D status1 (Fig. 7.1A, B, C). Patients with initial ASIA A scores recovered ∼ 5 points during the first year, whereas patients with initial ASIA B scores gained ∼ 31 points.1 Table 7.1 Predictors of Good Motor Recovery
Spontaneous Recovery Patterns and Prognoses after Spinal Cord Injury
 Neurological Level of Injury
Neurological Level of Injury
 Timing of Exam
Timing of Exam
 General Aspects of Motor Recovery
General Aspects of Motor Recovery
Incomplete injury |
Presence of pinprick sensation at the level of injury, in the zone of partial preservation, or at sacral segments |
Antigravity strength in the first caudal level below injury level |
Presence of some recovery in the first month after injury |
Rapid rate of recovery in the first week to month |
Brown-Séquard and central cord syndromes have better prognosis than anterior cord syndromes |
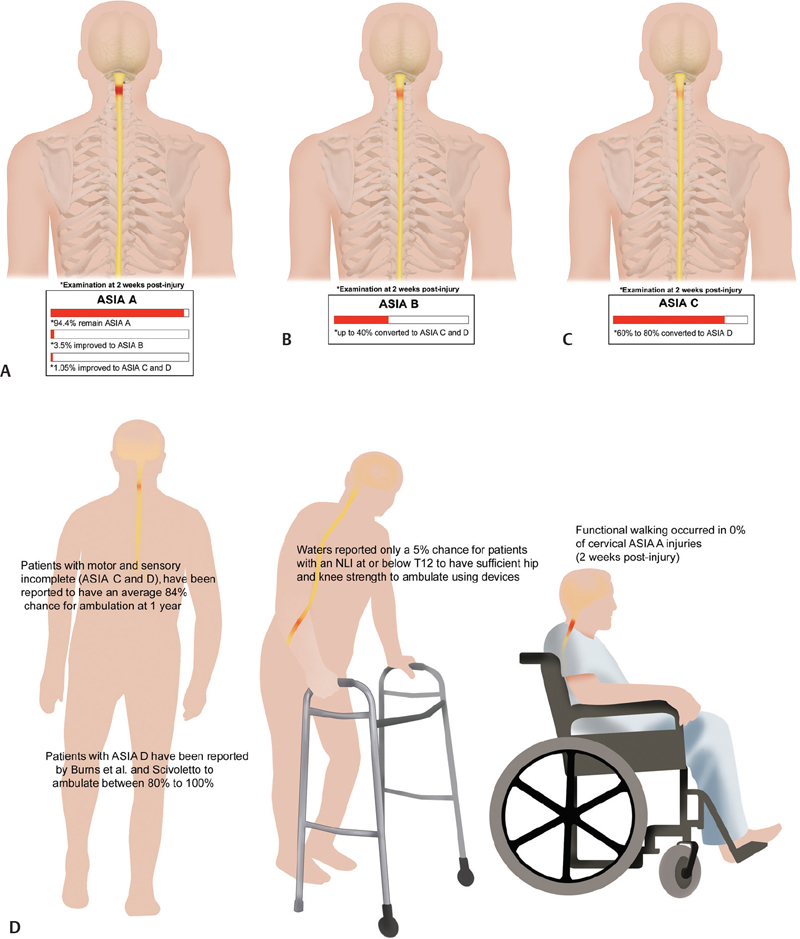
Fig. 7.1 (A–C) Spontaneous neurological rates based on 2 weeks postinjury ASIA scores. About 20% of ASIA A (complete SCI) patients experience some level of spontaneous recovery within the first year. Between 15 and 40% of patients with initial ASIA B scores converted to ASIA C or D status, and 60 to 80% of patients with initial ASIA C scores converted to ASIA D status.14 (D) Impact of injury severity and level on ambulatory function. Cervical ASIA A injuiries have worst prognosis with regard to likelihood of ambition. Patients with injury levels at or below T12 had 5% chance of ambulation with devices.4,5,11,22,29,35
 Recovery in Complete Tetraplegia
Recovery in Complete Tetraplegia
Most complete tetraplegia patients (66 to 90%) spontaneously regain one root level of function.4 C4-level injuries appear to have a lower rate of recovery in C5 biceps muscles compared with recovery of the next caudal neurological level in patients with C5 injuries. In one study, 33% of complete tetraplegia patients with a C4 injury with 0/5 biceps strength regained antigravity strength (3/5) at 6 months, 38% at 1 year, and 53% at 2 years.4 In comparison, 40% of complete tetraplegia patients with a C5 injury with 0/5 strength in wrist extensors regained antigravity strength at 6 months, 51% at 1 year, and 64% at 2 years.4 It is important to test the C5 muscles rather than C6 muscles when assessing recovery at the next caudal level in C4 tetraplegics in order not to underestimate the extent of recovery.2
The initial strength of the muscles is another important predictor of likelihood of achieving antigravity strength. Complete tetraplegics with no strength (0/5) at the next caudal level at 1 month follow-up were able to recover 27% of the time to antigravity strength, while patients with some strength (1 to 2/5) initially were able to recover 97% of the time to regain antigravity strength at the next caudal level at 1-year follow-up.2 In addition, the faster a muscle with no initial strength (0/5) recovers some strength (> 0/5), the better the prognosis is for recovery.15 Wu et al. noted that patients who developed certain milestones (1/5 at 1 month and 2/5 by 2 months) had a greater chance (86%) for recovery to antigravity or more by 1 year.15
Over all, Waters et al. found that motor score improvement averaged 8.6 ± 4.7 points in patients with a complete injury between C4 and C7, whereas the control group ASIA A patients (from the National Acute Spinal Cord Injury Study [NASCIS] II database) gained 4.6 points after 1 year.1,12
 Recovery in Complete Paraplegia
Recovery in Complete Paraplegia
The extent of recovery of lower extremity (LE) functioning in patients with complete paraplegia on admission appears to be related to the level of injury. In one study (N = 148), patients with an NLI above T9 did not regain any LE function 1 year postinjury, whereas 38% of patients with an NLI below T9 regained some LE functioning.9 Of patients who had complete paraplegia upon admission, only 4% rehabilitated to incomplete status, with half of these patients (2%) recovering bowel and bladder control.9
 Recovery in Incomplete Tetraplegia
Recovery in Incomplete Tetraplegia
Incomplete injuries are associated with a wider range of neurologic recovery.7 Although patients with complete lesions may improve one and sometimes two levels, individuals with incomplete lesions often have recovery at multiple levels below the neurological level of injury. Those with incomplete injuries will achieve a plateau of recovery to the next level more rapidly than complete lesions in 9 to 12 months. In comparison to complete injuries, patients with motor incomplete injuries had an average increase in motor score improvement of 10.6 ± 6.9.10 In the NASCIS II control group, patients with initial ASIA B, C/D injuries improved 31.3 and 12.9 points, respectively.1 The improvement in motor scoring, however, is limited by the “ceiling effect,” because the ASIA D patients can only recover a few points to normal strength. This “ceiling effect” has been described in the literature and is important to consider when trying to assess various therapies or to design clinical trials for patients with incomplete tetraplegia.8
The appearance of some motor function early (within 1 month) has been suggested as a predictor of better functional outcome. Waters et al. reported recovery from 1 month to antigravity at 1 year to be 20% for an initial 0/5 score, 73% for 1/5, and 100% for a 2/5 score.10 Ditunno et al. reported that recovery to at least grade 3/5 in the elbow flexors and extensors and the wrist extensors was more likely if the patient had exhibited voluntary movement in those muscles 1 week following injury.4 The presence of a muscle flicker in the lower extremities has been found to be a high predictor (86%) of recovery.17 Ditunno et al. also reported that the initial strength of a patient’s elbow flexors could predict a recovery of the individual’s wrist extensors.7
Within the category of incomplete tetraplegia, there are three separate incomplete syndromes: central cord syndrome, Brown-Séquard syndrome. and anterior cord syndrome, each with distinguishing motor and sensory loss patterns. Central cord syndrome is often seen in older individuals due to hyperextension of the neck. In central cord syndrome, motor loss is more severe in the upper extremities than in the lower extremities. These patients often have motor recovery comparable to other incomplete tetraplegics, although a relatively lower percentage of these patients achieve ambulatory ability.2,18 In one study,19 ASIA motor scores improved from a mean of 58.7 at injury to a mean of 92.3 at long-term follow-up (mean = 70 hours). Despite the large improvement in motor scores, significant disability and loss of functionality remained. The persistence of weakness in the upper extremities may compromise the patients’ ability to use ambulatory assistive devices.2
Brown-Séquard syndrome results from an ipsilateral hemisection SCI leading to ipsilateral hemiplegia and proprioceptive loss and contralateral hemianalgesia. These patients usually have a favorable prognosis, with 75% of patients achieving ambulatory capacity, with a 30 point increase in ASIA motor score in one study at long-term follow-up.2,20
Anterior cord syndrome involves a loss of motor function and pinprick sensation with preservation of light touch sensation and joint position sense.3 Anterior cord syndrome has a poorer prognosis than the other incomplete syndromes. Only 10 to 20% of patients experience motor recovery.2 In one study,21 patients with anterior cord syndrome recovered 22 motor points (final motor score, 38); those with a central cord syndrome gained 29 motor points (final motor score, 76); and those with Brown-Séquard syndrome gained 30 motor points (final motor score, 73).
 Recovery in Incomplete Paraplegia
Recovery in Incomplete Paraplegia
According to Waters et al., patients with incomplete paraplegia showed a spontaneous average gain of 12 lower extremity motor score points 1 year after injury. Further, of the 54 patients with incomplete paraplegia they evaluated, 76% were able to ambulate 1 year postinjury.22
 Sensory Recovery
Sensory Recovery
Sensory functioning for the ASIA scale is graded on a range from 0 to 2, with 0 being absent and 2 being normal. Studies show an association between sensory and motor recovery.14 In fact, motor recovery can be predicted by the maintenance of pinprick sensation post-SCI.23 Sensory and motor gains tend to occur within the same time frame. The extent of sensory recovery may be unrelated to motor recovery, in part due to the reliance upon the patient’s subjective assessment of sensory perception (as opposed to the more objective motor assessments).1 Usually, however, spontaneous recovery of sensation follows a time course pattern similar to that of spontaneous recovery of motor function.
For ASIA A patients (sensory complete, motor complete), the presence of some sensation at the level of injury increases the chances of recovery.24 Specifically, the presence of bilateral pinprick sparing has been noted to be a favorable predictor of motor recovery. Patients who are ASIA B (sensory incomplete, motor complete) who were noted to have intact bilateral sacral pin-prick sensation had a good likelihood (37%) of regaining lower extremity antigravity strength in at least one muscle.17,25 The correlation between spontaneous recovery and pinprick was also demonstrated by Poynton et al.26 in that muscles with 0/5 strength but pinprick preservation at the same level were associated with 92% recovery to antigravity for incomplete injuries, and 77% for complete injuries at 1 year. Conversely, if there was no pinprick preservation, recovery to antigravity or greater was 1.3% for complete and 3.9% for incomplete injuries at 1 year. In terms of specific motor recovery related to sensation, Browne et al. found that five of six patients who recovered to antigravity from 0/5 strength initially at C6 had C5 pinprick sensation, whereas only two of nine without C5 pinprick sensation recovered to antigravity.24 Over all, the presence of intact pinprick sensation at C5 was highly predictive of antigravity or greater motor recover at C6.
The Sygen study (GM-1 ganglioside or Sygen) results showed that patients with sacral pinprick sensation were more likely (results not statistically significant) to recover ambulatory function.1,27
The fact that pinprick preservation is a more important predictor of motor recovery than light touch is due to the anatomical proximity of pinprick fibers to the motor fibers in the spinal cord.2 The lateral spinothalamic tracts containing pinprick fibers are located just ventral to the lateral corticospinal tracts that contain the motor fibers. Preservation of pinprick would suggest an injury that probably spares the lateral spinothalamic tract and therefore likely spares the lateral corticospinal tract.
 Ambulation
Ambulation
Recovery of ambulation is an important goal for patients with SCI and is a significant milestone in rehabilitation. Some researchers have defined the motor requirements for ambulation to be antigravity (ASIA score > 3/5) in both the hip flexors on one side and the quadriceps on the contralateral side. Functional walking occurred in 0% of cervical ASIA A injuries and 8.5% of thoracic and lumbar ASIA A injuries.28,29 Waters reported only a 5% chance for patients with an NLI at or below T12 to have sufficient hip and knee strength to ambulate using devices.30 None of the complete tetraplegics achieved ambulatory ability.28,29 Of complete paraplegics, only 5% were able to ambulate at the community level at 1- and 2-year follow-up. All patients who recovered the ability to ambulate had an NLI at or below T12.9 Ambulation was reported from 0 to 89% in patients with ASIA B, depending largely on preservation of pinprick sensation.25 As already mentioned, pinprick sensation preservation predicts a more favorable prognosis. In patients with ASIA B, Crozier et al. found an 11% rate of ambulation, whereas Waters et al. reported 0%.25,31 However, ambulation ranged from 33 to 89% in those with pin-prick preservation.25,31
With respect to patients with motor and sensory incomplete SCI (ASIA C and D), the field has proven that spontaneous recovery of walking function occurs for a majority of patients.20,25,31–33 Specifically, Crozier et al. and Maynard et al. reported these patients to have an average 84% chance for ambulation at 1 year.25,33 However, practitioners should consider that age, timing of motor recovery, and lower/upper extremity strength are factors that influence the chance of ambulation in these patients. For example, in ASIA C patients older than 50, Scivoletto and Di Donna found that 25% and Burns et al. found that 42% had a chance of ambulation, whereas those younger than 50 had a 71% and 91% chance of ambulation, respectively.29,32 Scivoletto and Di Donna and Burns et al. reported ambulation between 80 and 100% in patients with ASIA D at discharge from inpatient rehab.29,32 Early recovery of a minimum of antigravity quadriceps strength in at least one quadriceps by 2 months was shown to be an excellent predictor of ambulatory recovery.34
Recently, predictive factors for ambulation were determined by Zörner and colleagues.35 Among predictors like age, gender, sensation, motor scores, and somatosensory evoked potentials, lower extremity motor score (LEMS) was identified as the single best predictor for walking. In combination with LEMS, somatosensory evoked potentials and ASIA scale scores increased the prediction of ambulatory outcome in tetraparetic subjects to 92% and 100%, respectively. This model, however, was less successful at predicting ambulatory outcome in paraparetic patients.35
The importance of the LEMS in predicting ambulation was also confirmed in previous studies.10 In incomplete tetraplegics, an initial LEMS of 20 or greater was associated with attainment of community ambulation at 1 year postinjury. Overall, patients with incomplete tetraplegia had a 46% chance of community ambulation at 1 year; patients with LEMS between 10 and 19 had a 63% chance of ambulation and patients with LEMS greater than or equal to 20 achieved a 100% rate of community ambulation.10 Ambulatory success depended on upper extremity motor score, with mean score of 16.1 in nonambulators versus 30.3 for community ambulators. In contrast, only 21% of patients with LEMS between 1 and 9 achieved community ambulation. In incomplete paraplegics, all patients with a 1 month LEMS of > 10 points ambulated at 1 year follow-up and 70% with LEMS between 1 and 9 ambulated at 1 year follow-up22 (Table 7.2).
 Demographic Factors That May Affect Recovery
Demographic Factors That May Affect Recovery
Gender
A few studies have examined the role of gender and SCI. Sipski et al. reviewed data from 14,433 patients from the MSCIS and found that women had greater changes in ASIA motor scores after 1 year than men.30 A functional outcome comparison, however, yielded higher functional independence measure (FIM) motor scores for men with ASIA A or B injuries, except for those with C1–4 and C–6 neurological levels. It should be noted that at the time of admission, men had more severe injuries (i.e., more likely to have complete SCI) than women. Interestingly, in this study, except for an increased risk for men to develop pulmonary embolus, there were no other gender effects on the development of other medical complications. Similarly, Furlan et al. found no gender differences in inpatient mortality associated with acute traumatic SCI.36
Table 7.2 Favorable Predictors of Ambulation
Age < 50 |
Injury level below T9 |
Preservation of pinprick sensation |
American Spinal Injury Association grade ≥ C |
Antigravity strength in at least one quadriceps by 2 months |
Lower extremity motor score > 10 at 1 month |
Initial lower extremity motor score of 30 or greater (community ambulation) |
Age
Several studies have examined the relationship between age and outcome after SCI. Scivoletto et al. reviewed 284 SCI subjects more than 50 years old and found that the younger individuals had better recovery in terms of their ASIA impairment levels and increased ASIA motor scores.37 Older individuals had more medical complications but also had shorter lengths of stay and performed better on a few activities of daily living (ADL). Younger individuals tended to have more favorable outcomes with walking and bladder/bowel independence. In another study by Fisher et al. that looked at 70 ASIA A patients, there was a trend toward better neurological recovery for patients under 24 years old.38 Van Hedel and Curt reviewed the records of 98 ASIA A/B subjects and found that functional outcomes, as measured by a spinal cord independence measure, decreased significantly with increasing age.39 It is hypothesized that older patients will have greater morbidity and mortality rates. Boakye et al., using the national inpatient sample, found that patients more than 45 years of age had a higher risk of in-hospital mortality following acute SCI.40
 Comorbidities
Comorbidities
Comorbidities affect morbidity and mortality after injury and hence may directly or indirectly influence recovery. Boakye et al. found that patients who had three or more medical comorbidities had a 1.8 times higher risk of mortality and were 1.45 times as likely to be discharged to an institution other than home than those with no comorbidities.40 In a retrospective cohort study (N = 297) of patients with acute traumatic SCI, Furlan et al. found that comorbidities confounded the age-related differences in mortality during initial hospitalization following an acute traumatic SCI.36 In addition, this study demonstrated that the Charlson Comorbidity Index (CCI) is a reliable and valid way to measure comorbidities for the purpose of predicting in-hospital mortality for patients with acute traumatic SCI after controlling for age. Thus, a measure of comorbidities (using the CCI) appears to be an important factor when one is drawing conclusions about mortality rates following SCI.
 Conclusion
Conclusion
It is important for health-care professionals to be knowledgeable about the patterns of spontaneous recovery in patients with SCI, as well as the factors that affect recovery after treatments for SCI. This information will assist physicians in properly informing patients of their likely prognoses, explaining the risks and benefits of interventions, and, most importantly, making treatment decisions.
Pearls
 Patients without initial motor or sensory function below the injury may still achieve excellent recovery.
Patients without initial motor or sensory function below the injury may still achieve excellent recovery.
 The most important factors are the completeness of injury, the initial strength of muscles at the first caudal level, and the level of neurological injury.
The most important factors are the completeness of injury, the initial strength of muscles at the first caudal level, and the level of neurological injury.
 The rate and extent of recovery are greatest within the first 6 months after injury, but recovery can continue for many months thereafter for up to 2 years.
The rate and extent of recovery are greatest within the first 6 months after injury, but recovery can continue for many months thereafter for up to 2 years.
 Preservation of pinprick sensation at the level of injury in the zone of partial preservation or in the sacral segments are favorable predictors of motor recovery and future ambulation.
Preservation of pinprick sensation at the level of injury in the zone of partial preservation or in the sacral segments are favorable predictors of motor recovery and future ambulation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


