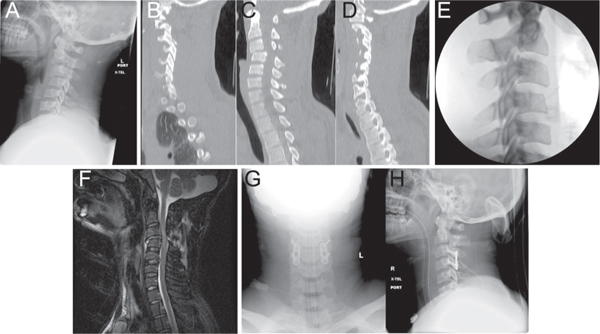
12 Key Points 1. The goals of surgical intervention are multifactorial and include decompression of the neural elements, establishing a stable spine to prevent painful deformity or neurological decline and to allow for early mobilization of the patient. 2. Unique classification systems exist for each different region of the spine and provide a mechanism for communication between clinicians. 3. Decompression alone of the injured spinal cord is often contraindicated and must be supplemented with a stabilizing or fusion procedure. 4. Evidence is accumulating that early decompression (defined as within 24 hours of the injury) and stabilization of a patient with spinal cord injury may lead to improved neurological outcomes. The earliest reports of spinal column injury with neurological deficits, referred to as spinal cord injury (SCI), date back to 2500 bc in the Edwin Smith Surgical papyrus.1 The view at that time that a SCI was “an ailment not to be treated” remained the attitude of physicians for centuries. In 1262, Theodoric of Bologna wrote a surgical text, Chiurgica de Theodoric,1 in which he discussed the surgical treatment of spinal column disorders. This text stressed the importance of the reestablishment of proper alignment by reduction and stabilization to heal these injuries. Contemporary spine surgeons uphold the philosophy of stabilization and decompression. Despite early recognition, SCI remains a significant cause of morbidity and mortality, with ∼ 10,000 to 12,000 cases occurring annually in the United States,2–4 primarily in younger adults.4 The financial and social costs associated with SCI are enormous; medical costs alone are in excess of US$7 billion a year.3 Such large figures clearly indicate the need to establish which injuries require surgical intervention and when such a procedure should be performed. With innovations in neuroanesthesia, the advent of antibiotics, and advances in surgical techniques and instrumentation, contemporary spine surgeons can be more confident in the ability to manage spinal trauma in an operative fashion than were their predecessors. Because of the wide array of injuries that can afflict the spinal column, the role of surgery is hard to define globally, and the decision to proceed operatively must instead be made on a case-by-case basis. Specific surgical goals in the management of all SCI should include (1) the establishment of a balanced and stable spine, (2) the preservation or improvement in neurological function, and (3) the quick return of the patient to an optimal level of functional capacity.5 In each case, the surgeon must evaluate whether the surgical risks outweigh potential benefits and judge whether surgery can achieve the aforementioned goals more effectively than nonoperative treatment. Historically, many physicians took the stance that spine surgery for acute SCI is warranted in only those patients who have progressive neurological deterioration or in those with gross spinal instability. Prior to the 1970s, the only operative treatment available was laminectomy without instrumentation, and this was avoided because of the higher incidence of neurological complications and worse clinical outcomes.6,7 Guttman8 advocated the use of postural techniques combined with bed rest to achieve reduction and spontaneous fusion of the spine. Dall,9 Harris et al.,10 and Bedbrook7 all indicated that neither spinal surgery nor anatomical alignment of the spinal column improved the neurological outcome in patients with acute SCI, with the exception of bilateral locked facets. Although many studies agreed in their findings about nonoperative treatment, these reports were retrospective case series and provided only Class III data. In addition, nonoperative treatment is not without risks: Up to 10% of patients with incomplete cervical SCI have neurological deterioration while being treated in an exclusively nonoperative manner.11 With improved surgical care, outcomes after surgical treatment of spinal trauma patients have improved and made the surgical treatment of SCI a viable option. Several factors weigh in favor of a surgical approach in many cases. For example, with modern techniques, surgery can accelerate the rehabilitation process by reducing the complications associated with prolonged immobilization, decreasing morbidity for the patient and indirectly decreasing the medical costs. Similarly, stabilizing the spine through instrumentation and fusion should prevent spinal deformity, which may manifest at a later time as progressive pain, loss of function, and neurological deterioration. The decreased length of hospitalization, quicker rehabilitation, and earlier return to society are all clear advantages to surgical intervention.12,13 In addition, operative intervention can decrease the cascade of secondary injury associated with SCI by decreasing the degree of neural compression.14,15 Acute SCI results from a combination of primary and secondary injury mechanisms. The primary injury is the initial insult that transmits direct mechanical trauma to the spinal cord and may involve a contusion, laceration, blast injury, ischemic event, or direct shearing of spinal cord axons. It often results in fragments of the vertebral body or disk material directly causing neural compression.14–16 This leads to a cascade of biochemical events known as the secondary injury mechanism, leading to ischemia, neurogenic shock, hemorrhage, vasospasm, edema, ionic derangements, neurotransmitter accumulation, production of free radicals, inflammation, and apoptosis. It is this secondary injury cascade that damages the neural elements in the hours after injury.14–16 Rabinowitz et al.17 demonstrated in canine studies that the severity of the pathological changes and degree of recovery were directly related to the duration of acute compression. In essence, persistent compression of the spinal cord is a potentially reversible form of secondary injury. Pharmacological treatment, closed fracture reduction, and surgical decompression are employed to reduce the zone of injury attributed to the secondary cascade.14–16 Class III studies have shown a benefit of surgical treatment at various time points. In their evaluation of early decompression, Wagner and Chehrazi18 found no difference in recovery but cited a study by Hamel et al. who retrospectively evaluated the role of surgical intervention on neurological outcome after acute SCI in the cervical spine. Those authors found that 53% of patients treated with surgical decompression and fusion retained the ability to walk, whereas only 23% of those patients treated conservatively retained this function. Surgery also appears to benefit patients with long-standing compression of the spinal cord, regardless of the duration of time from injury. Bohlman and Anderson19 described a series in which 58 patients who had remote cervical spine trauma with incomplete injuries underwent anterior decompressive and fusion procedures. Half of the patients demonstrated a marked improvement in their functional status. Fehlings et al. have presented the initial results of a large multicenter observational study (STASCIS) looking at 6- and 12-month outcomes following surgery and decompression for cervical SCI. Acute decompression, defined as decompression within 24 hours of the injury, led to a significant improvement in American Spinal Injury Association (ASIA) motor classification at 6 and 12 months. When completed, this study will provide strong level II evidence that early decompression is beneficial for long-term outcome in motor function.20 White and Punjabi21 defined stability as the “ability of the spine under physiologic loads to limit patterns of displacement so as not to damage or irritate the spinal cord or nerve roots and in addition to prevent incapacitating deformity or pain due to structural changes.” Any traumatic spinal injury that disrupts the biomechanical stability of the spine contributes not only to neurological injury but also to musculoskeletal injury that in turn will affect the functional status of the patient. Surgery helps to reestablish the alignment of the spine and subsequently stabilize the spinal column to prevent further neurological injury, deformity, and pain.22 Several classification systems have been developed that attempt to predict the degree of instability after spinal trauma. None of these systems has been universally adopted, and none has prospectively analyzed the ability to predict instability.23 What is inherent in all classification systems is that both osseous and ligamentous structures contribute to the stability of the spine and are not independent of one another, although instability in either alone can cause neurological deterioration.23 Kostuik24 demonstrated that disruption of the ligamentous structures in the cervical, thoracic, or lumbar regions without osseous injury predisposed to spinal deformity with associated neurological deterioration. This is most devastating in cases of occipitocervical dislocation, bilateral facet disruption, and transverse ligamentous disruption.25 Nonoperative management of spinal instability in the setting of trauma has not always been successful. Anderson and Bohlman26 prospectively studied a series of patients with cervical spinal injuries that were treated with halo vests and immobilization. In these patients, imaging in both the supine and the upright positions demonstrated intervertebral motion. The authors also noted that changes in body posture translated into either a compressive or a distractive force at the injury level while the patient was in a halo orthotic device. Because of the length of the spinal column and the different function of each region, unique biomechanical properties exist at each level of the spinal column. Thus we will consider the role of surgical intervention at each level separately. The degree of motion from the cervical spine is due to this region’s unique ligamentous and osseous anatomy. This unique anatomy, however, predisposes it to the risk of major injury and subsequent catastrophic neurological injury. Within the cervical spine, it is imperative in the setting of trauma to adequately visualize the cervicothoracic junction because this region accounts for 17% of all cervical spine fractures.27 The cervical spine is often viewed as two distinct regions, the upper cervical spine (occiput to C2) and the subaxial or lower cervical spine (C3–7). The upper cervical spine deals with flexion and extension between the occiput and the atlas and allows rotation of the head through the atlantoaxial junction. The ligamentous structures in this region are of critical importance because they provide most of the stability in this region. Many of the injuries of the upper cervical spine are not associated with SCI because of the generous canal size and the relatively small osseous volume at C1 and C2. This chapter concentrates on injuries of this region with a relatively higher incidence of SCI. The unique anatomy of the occipitocervical junction and the difficulty of approaching the upper cervical spine from an anterior approach make posterior stabilization and fusion the preferred choice for most injuries in this region. Occipitocervical dislocations are uncommon ligamentous injuries that result from hyperflexion and distraction during high-impact blunt trauma.28 These are unstable and frequently fatal injuries that cause neurological injury from stretching, compression, and distortion of the spinal cord, brain stem, and cranial nerves.29 Vertebral artery injury also accounts for significant morbidity and mortality in this region. Occipitocervical junction injuries were often recognized in a delayed fashion on routine cervical radiographs, but the use of routine computed tomographic (CT) scans in the polytrauma patient has led to more timely recognition of this injury.30 Initial management of these injuries focuses on immobilization to limit further injury, with or without a halo orthosis, and never with traction. Nonoperative management of these injuries does not provide definitive treatment because of the significant ligamentous disruption that cannot heal even with prolonged external immobilization. Operative stabilization involves an occipitocervical arthrodesis with rigid internal fixation after restoration of alignment. Transverse ligamentous injuries are unstable injuries that may result in SCI. Occasionally, these are isolated injuries, but often they are associated with C1 or C2 fractures. Integrity of this ligament is the key to stability of the C1–2 region.31 These injuries can be diagnosed by recognizing a widened atlantodental interval on lateral radiographs or displacement of the C1 lateral masses on an open-mouth odontoid view or coronal CT reconstruction. Transverse ligamentous injuries are classified into two categories based on their radiographic appearance.31 Type I injuries involve disruption of the midportion (Ia) or periosteal (Ib) insertion laterally. Type II injuries involve fractures that disconnect the C1 lateral mass tubercle from the transverse ligament through either a comminuted fracture (IIa) or an avulsion fracture (IIb). Type I fractures are purely ligamentous injuries that often do not heal by immobilization alone, so posterior C1–2 arthrodesis is indicated. Type II injuries have a 74% chance of healing with halo immobilization, so that may be tried before surgical intervention if the patient prefers.31 Isolated axis and odontoid fractures rarely cause significant compromise of the spinal canal or neurological injury and will not be discussed here. In the subaxial cervical spine (C3–7), the osseous and ligamentous structures play an equal role in stability. The spinal canal in this region is smaller than that in the upper cervical spine, which predisposes to SCI with any compressive or translational forces. As a result, those patients with congenitally narrowed cervical spinal canals are more at risk for devastating neurological injury with trauma. In 1982, Allen and colleagues32 described a mechanistic classification of subaxial cervical spine trauma. This classification divides mid- and low-cervical fractures into six groups based on force vector and incremental tissue failure. Abnormal sagittal alignment between adjacent vertebrae implies ligamentous failure, suggesting a shear force mechanism because ligaments do not fail with compression. The three most common injury types are compressive flexion, compressive extension, and distractive flexion. Vertical compression injuries occur with intermediate frequency, distractive extension and lateral flexion injuries occur the least. Neurological injury within all six subgroups is common.32 Compressive flexion injuries are caused by a ventral and axially directed load of increasing intensity. Compressive fractures without subluxation and facet injury are more stable injuries, whereas injuries with increased ventral osseous and dorsal ligamentous injury tend to be unstable. If the spine can be aligned in the sagittal plane, surgical intervention through an anterior approach with corpectomy and instrumented fusion with a structural graft is sufficient. If alignment requires direct reduction of the facet joint or there is significant posterior facet damage, a dorsal approach with stabilization is often warranted. Compressive extension injuries range from unilateral vertebral arch fractures to bilateral laminar fractures and finally to vertebral arch fractures with full ventral displacement of the vertebral body. The general surgical objective involves a dorsal approach with reduction and stabilization followed by adjunctive ventral reconstruction if there is significant vertebral body comminution and displacement. Distractive flexion injuries, also known as fracture dislocation injuries, are often devastating injuries (Fig. 12.1) and are caused by flexion and distraction forces with or without an element of rotation. These injuries include perched, jumped, and locked facets and have the potential for progressive neurological deterioration. Failure of all posterior ligamentous structures (ligamentum flavum, facet capsule, interspinous ligament) has been demonstrated in patients with both unilateral and bilateral facet dislocation.33 Most injuries within this spectrum are unstable and require surgical stabilization after reduction and decompression.32,33 Magnetic resonance imaging (MRI) is useful to identify a herniated disk fragment prior to open or closed reduction procedures, especially if the patient is unconscious and unable to be examined.33 Definitive management of facet injuries (unilateral, bilateral) begins with closed reduction through skull traction to restore proper alignment. If proper alignment is obtained, then a ventral decompression and stabilization is the preferred surgical approach; if proper alignment is not attainable, a dorsal decompression and stabilization is needed. Fig. 12.1 (A) Lateral x-ray of the cervical spine showing C3-4 fracture dislocation in a 22-year-old man. The patient had an American Spinal Injury Association motor score of 0 with some sensory sparing initially. (B–D) Computed tomographic scans of the cervical spine showing associated perched facets. (E) Despite the application of 80 lb of traction, the fracture could not be reduced, and the patient developed respiratory difficulty. (F) Sagittal short tau inversion recovery sequence magnetic resonance imaging showing significant posterior ligamentous injury with cord signal change and cord compression. The patient underwent posterior spinal fusion. Postoperatively, he recovered to 4/5 strength in his deltoids, but his sensory examination remained unchanged. (G) Anteroposterior and (H) lateral x-rays showing C3-4 posterior spinal fusion.
Principles of Surgical Management of Spinal Trauma Associated with Spinal Cord Injury
 Primary and Secondary Mechanisms of Spinal Cord Injury
Primary and Secondary Mechanisms of Spinal Cord Injury
 Spinal Stability
Spinal Stability
 Cervical Spine
Cervical Spine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


