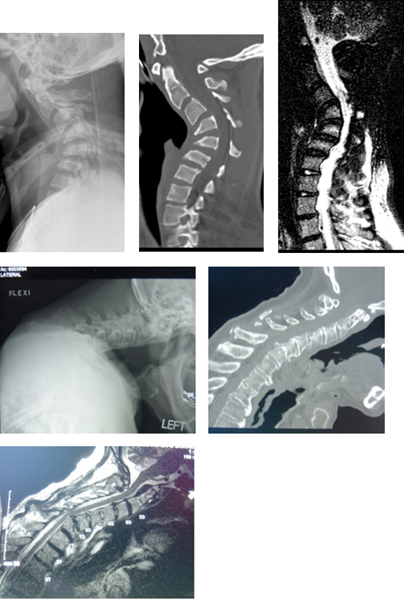
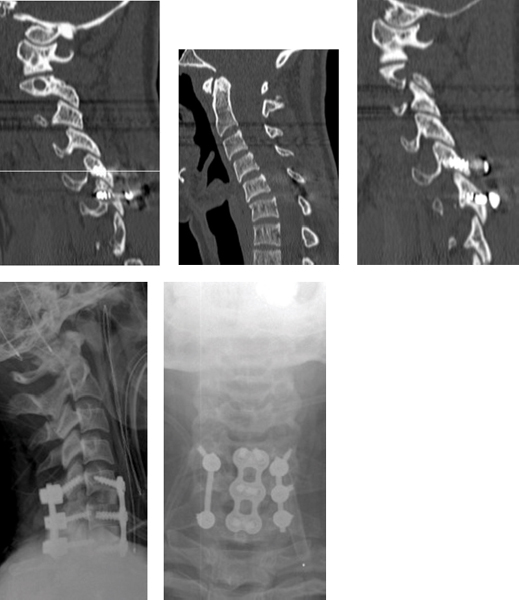
19 Key Points 1. The absolute indication for surgery for posttraumatic kyphotic deformity is progressive neurological deficit. Isolated progression of kyphosis more than 5 degrees is considered by some authors to be a relative indication for reconstruction for impending instability. 2. Anterior release and reconstruction facilitate mobilization of the spine and direct decompression of the neural elements. Posterior reconstruction enhances stability and restoration of lordosis. 3. The reported complication rate of circumferential reconstruction is 33% in the literature, with a 5% permanent complication rate usually related to anterior structures. Preoperative patient counseling is essential. Kyphosis is a common deformity after a variety of cervical spine traumatic injuries.1 The pathogenesis of kyphosis is an alteration of the biomechanics of the cervical spine. The normal cervical spine sagittal alignment is 40 degrees of lordosis, with the result that the weight-bearing axis of the spine lies in the posterior vertebral body and posterior elements.2,3 Kyphosis may lead to progressive kyphotic deformity, compromise of the adjacent spinal motion segments, and potentially even neurological symptoms. Kyphosis shifts the weight-bearing axis of the spine anteriorly, increasing the axial load on the vertebral bodies and disks. As kyphosis increases, so does the flexion movement, thereby increasing the likelihood of adjacent segment changes and progressive deformity. Cervical kyphosis may also result in compression of the anterior spinal cord against the posterior aspect of the vertebral body at the apex of the deformity (Fig. 19.1). This shift leads to increased mechanical stress on the anterior aspect of the spinal cord and possible ischemia.4,5,6,7 Clinically, a consequence of loss of bony ligamentous competence is often a loss of alignment. Kyphosis may develop after any injury morphology, including compression, distraction, or translation.8 Compressive injuries may result in insufficiency of the vertebral bodies to manage axial load. Distractive injuries may result in kyphosis, either gradually due to posterior ligamentous laxity, disk injury with resultant disk desiccation, and spondylosis, or acutely due to late dislocation and instability. Translation may result from flexion compression or flexion distraction injuries. Spondylolisthesis results in relative kyphosis of the motion segment. Fig. 19.1 Severe posttraumatic kyphotic deformities resulting in spinal cord compression at the apex of the deformity. (A–C) The patient sustained a cervical burst fracture and developed posttraumatic kyphotic deformity and spinal cord compression. (D–F) The patient developed a chronic facet subluxation resulting in kyphosis, spondylolisthesis, and spinal cord compression. The precise incidence of posttraumatic kyphosis is variable depending upon the injury and its treatment. The rate of kyphotic deformity appears to be highest after conservative treatment of cervical compressive injuries. Koivikko et al. reported on the radiographic outcome of conservative and operative treatment of cervical burst fractures.9 Mean kyphosis in the conservatively treated patients (12.6 ± 10 degrees) was greater than that in the anterior cervical decompression and fusion (ACDF)-plating group (–2.2 ± 13.9 degrees) (p = 0.00003). Furthermore, kyphotic deformity progressed late in 8/34 patients in the conservative treatment group and in 4/35 surgically treated patients. There were no neurological deficits reported with progression of kyphosis. Fisher et al. studied patients with flexion teardrop (compression) injuries and found increased mean kyphosis of 11.4 degrees (range, 0 to 35 degrees) in the halothoracic vest (HTV) group compared with the anterior cervical plating group (3.5 degrees, 0 to 14°).10 Furthermore, five patients in the HTV group were classified as failures, with average kyphosis of 4 degrees. Distraction injuries, conservatively or operatively managed, may result in loss of cervical lordosis. Lifeso and Colucci retrospectively reviewed the outcomes of 29 patients with cervical flexion distraction injuries and reported that, following posterior fusion, there was a 27% failure rate (3/11) related to late kyphosis.11 Of the 18 patients treated with an ACDF, there was no late collapse, pseudarthrosis, or persistent radiculopathy. Woodworth et al. report that 1 of 17 (5.8%) patients with posterior ligamentous injury treated with ACDF went on to a progressive kyphotic deformity.12 The patient remained neurologically intact and fused in a kyphotic position and required no further treatment. In a retrospective review of patients who underwent treatment for flexion distraction injuries, Johnson et al. identify a 13% incidence of radiographic failures after ACDF-plating associated with end plate fracture and facet fracture. Of the 11 patients who developed radiographic failure, nine had a pseudarthrosis and significant pain and two had a solid fusion and no pain. There were no neurological deficits associated with progression of radiographic deformity.13 Posttraumatic kyphotic deformity may develop as a result of iatrogenic removal of the posterior tension band (i.e., laminectomy). The development of postlaminectomy kyphosis secondary to multilevel cervical laminectomies has been well described in both the pediatric and adult populations, with frequencies as high as 50% and 14%, respectively.14,15,16,17 Clinical signs of posttraumatic cervical kyphotic deformity may include neurological deficit, neck pain, or change in posture. Any changes in neurological status or pain in a patient who has previously sustained cervical spine trauma should prompt aggressive clinical evaluation and imaging. The differential diagnosis of posttraumatic kyphotic cervical spine deformity includes infectious, neoplastic, Charcot degeneration, or compensatory changes as a result of trauma to contiguous and noncontiguous spinal levels. The gold standard for diagnosis of post-traumatic kyphotic deformity of the cervical spine is lateral upright radiographs. Pertinent radiographic findings include the nature of the deformity, whether it is focal or global, the presence of translational deformities, overall alignment and horizontal gaze, and compensatory deformities. The etiology of the deformity may be identified more clearly with magnetic resonance imaging (MRI) or computed tomographic (CT) scan. MRI offers superior resolution of diskoligamentous injuries, which may guide treatment by illustrating the presence or absence of significant anterior thecal sac compression. MRI, due to its sensitivity, may also demonstrate injury to supportive soft tissue structures, such as the facet capsules, ligamentum flavum, or interspinous ligaments, and thereby allow for earlier treatment prior to the development of a spinal deformity. Lambiris et al. identified two cases of cervical flexion distraction injuries where an injury to the intervertebral disk would have been addressed if MRI had been used for diagnosis.18 However, by the time the posttraumatic kyphotic deformity develops, usually the injury to the disk or facet capsules is manifested by morphological changes, such as desiccation, ankylosis, or subluxation. Superior bony resolution is well visualized with the use of CT. The absolute indication for treatment of a posttraumatic kyphotic deformity is a progressive neurological deficit associated with spinal cord compression (Fig. 19.1). A relative indication for treatment of a kyphotic deformity involves progression of deformity over time. There is controversy over the best radiographic method to measure alignment and kyphosis.19 Some authors define progression of the Cobb angle measurement of more than 5 degrees as a potential indication for treatment of a kyphotic deformity.9,12 Based on White-Panjabi analysis, Johnson et al. defined radiographic failure of treatment operatively or nonoperatively as vertebral translation greater than 3.5 mm and/or a change in vertebral angulation greater than 11 degrees or device failure in the interval between the immediate postop film and the most recent follow-up radiograph.13 However, a recent meta-analysis of the literature found that the interobserver reliability of Cobb angle measurement is 0.74 for evaluation of cervical arthrodesis success after ACDF, compared with 0.95 for spinous process tip distance measurement.20 Thus, interspinous process distance may be a more reliable measurement technique for the assessment of posttraumatic kyphosis progression. The principle of treatment of posttraumatic kyphotic deformity is avoidance of tension on the spinal cord. In the setting of a cervical kyphotic deformity that requires surgical correction, there are three approaches: anterior, posterior, or a combined anterior-posterior approach. Deformity correction may be effected by shortening of the posterior spinal column and lengthening of the anterior spinal column with an axis of rotation within or anterior to the spinal cord. The anterior approach allows for the direct removal of ventral compressive lesions via diskectomy and/or corpectomy as well as release on the concavity side of the deformity via resection of osteophytes and the joints of Luschka. However, in the presence of an incompetent posterior tension band, anterior decompression and reconstruction alone has been associated with graft complications, such as displacement, pseudarthrosis, and postoperative instability.21,22 Reconstruction after diskectomy and fusion may be associated with improved lordosis and reduced risk of graft dislodgment compared with cervical corpectomy (Fig. 19.2). However, corpectomy offers an improved neural decompression, particularly in the setting of an ossified posterior longitudinal ligament behind the vertebral body, compared with diskectomy (Fig. 19.3). The posterior longitudinal ligament is preserved, if possible, to act as a hinge at the time of deformity correction so as to limit spinal cord lengthening.23 Anterior instrumentation may prohibit any further realignment following a posterior procedure. If there is significant instability or soft bone quality, then an additional anterior approach should be considered to “lock in” the construct once the realignment is complete. The main advantages of dorsal surgery are the relative ease of multilevel decompression and improved biomechanical strength of instrumentation. Reconstruction in the setting of kyphosis correction usually consists of posterior instrumentation two to three levels cephalad and caudad to the apex level of correction. Either cervical lateral mass screws, pedicle screws, or wiring may be used. Posterior instrumentation has been shown to be biomechanically stronger than anterior instrumentation in axial rotation and lateral bending. Pedicle screws extend anterior to the instant axis of rotation of the spine and may be biomechanically superior to anterior fixation in flexion and extension.24 Abumi et al. demonstrated that mild degenerative kyphosis can be corrected entirely posteriorly with cervical pedicle screw fixation.25 At follow-up, the average correction went from 30.8 to 0.5 degrees of kyphosis.26,27 Figure 19.4 is an example of a patient with posttraumatic kyphosis from a chronic facet dislocation who underwent posterior correction with pedicle screws and a localized osteotomy. Fig. 19.2 (A–C) A pseudarthrosis of the posterior elements associated with broken hardware and kyphosis after a posterior fusion for a distraction injury. (D,E) The attainment of postoperative lordosis following anterior and posterior reconstruction.
Posttraumatic Kyphotic Deformity of the Cervical Spine
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine
