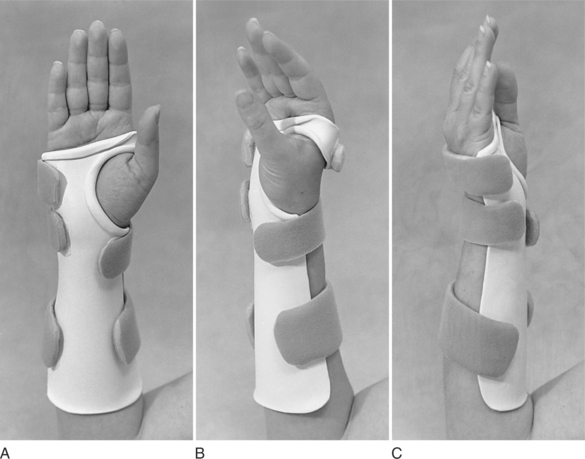
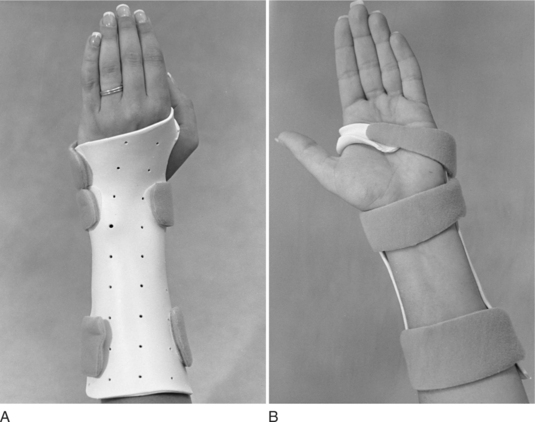
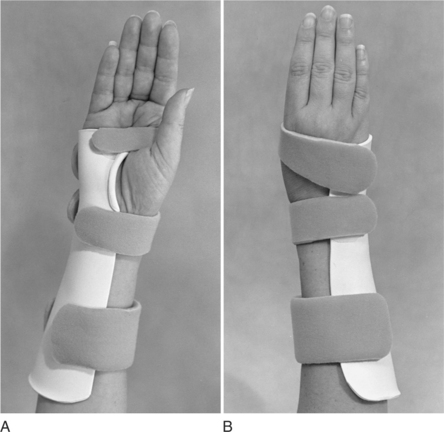
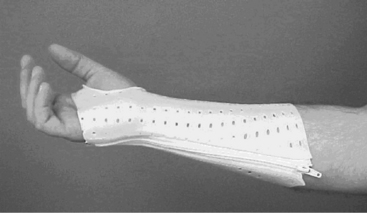
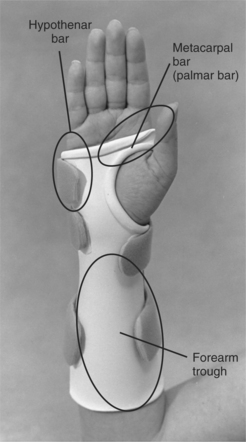
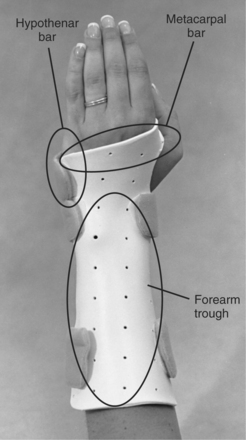
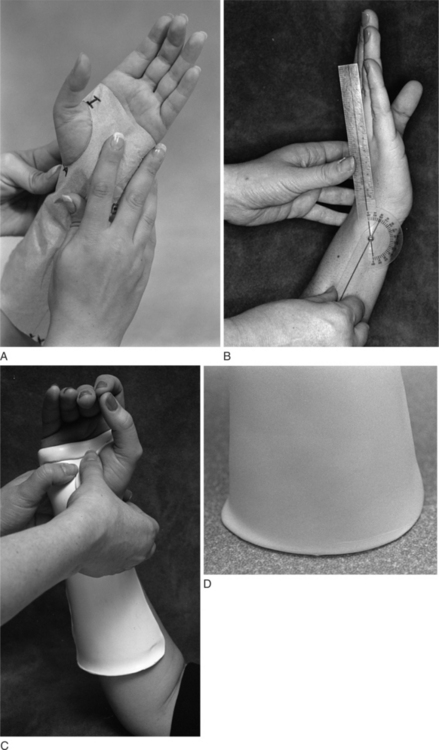
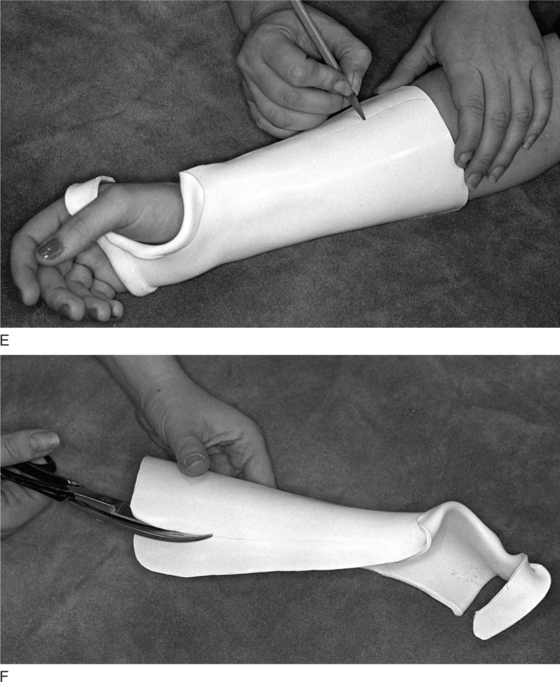
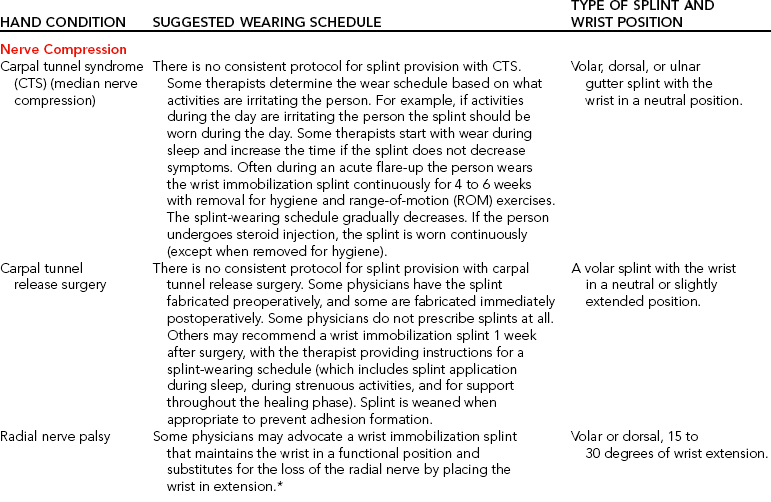
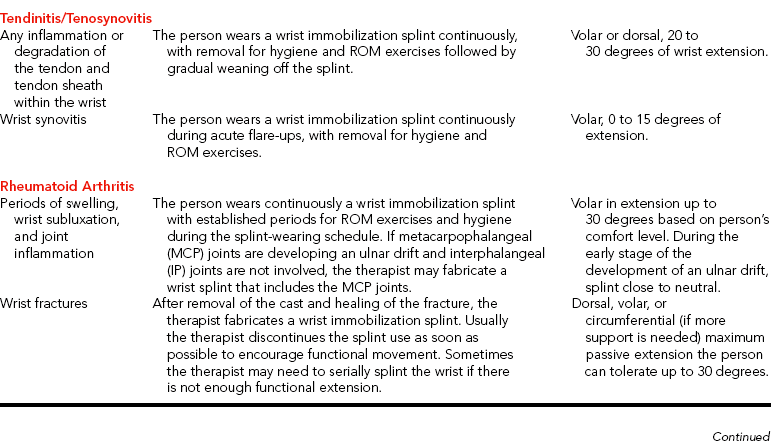
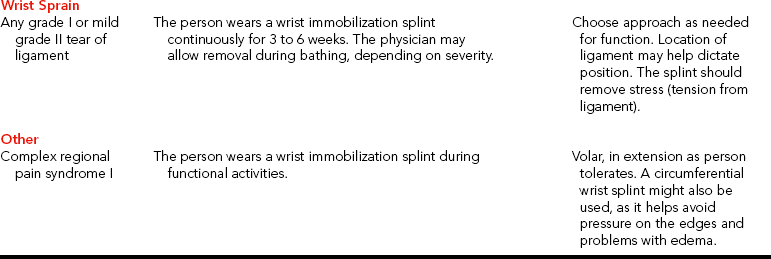
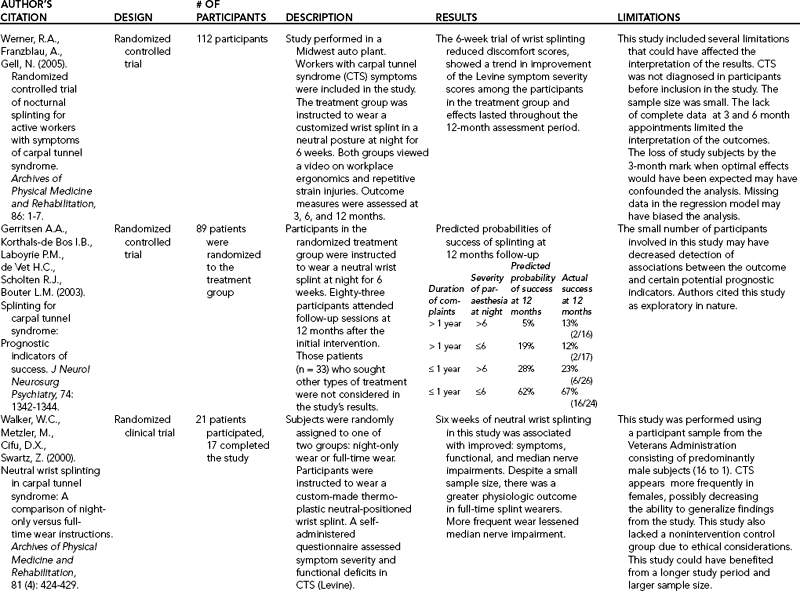
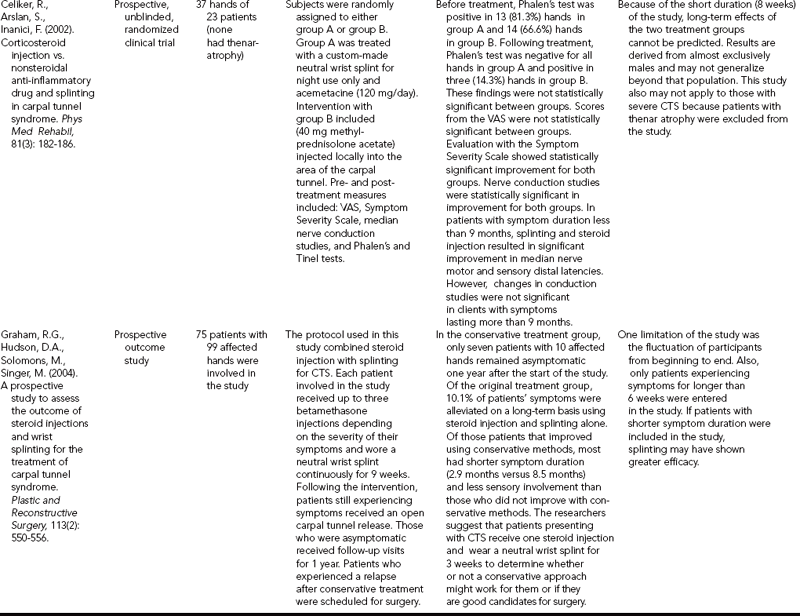
CHAPTER 7 1 Discuss diagnostic indications for wrist immobilization splints. 2 Identify reasons to serial splint with a wrist immobilization splint. 3 Identify major features of wrist immobilization splints. 4 Understand the fabrication process for a volar or dorsal wrist splint. 5 Relate hints for a proper fit to a wrist immobilization splint. 6 Review precautions for wrist immobilization splinting. 7 Use clinical reasoning to evaluate a problematic wrist immobilization splint. 8 Use clinical reasoning to evaluate a fabricated wrist immobilization splint. 9 Apply knowledge about the application of wrist immobilization splints to a case study. 10 Understand the importance of evidenced-based practice with wrist splint provision. 11 Describe the appropriate use of prefabricated wrist splints. Maintaining the wrist in proper alignment is important because the wrist is key to the health and balance of the entire hand. During functional activities, the wrist is positioned in extension for grasp and prehension. Therefore, the wrist extension immobilization type O splint [American Society of Hand Therapists 1992] or the wrist cock-up splint is the most common splint used in clinical practice. Wrist immobilization splints usually maintain the wrist in either a neutral or a mildly extended position, depending on the protocol for a particular diagnostic condition and the person’s treatment goals. A wrist immobilization splint immobilizes the wrist while allowing full metacarpophalangeal (MCP) flexion and thumb mobility. Thus, the person can continue to perform functional activities with the added support and proper positioning of the wrist the splint provides. Positioning the wrist in a splint in 0 to 30 degrees of wrist extension promotes functional hand patterns for completing functional activities [Palmer et al. 1985, Melvin 1989]. Therapists fabricate wrist immobilization splints to provide volar, dorsal, ulnar, circumferential forearm, wrist, hand, and (infrequently) radial support (see Figures 7-1 through 7-4). Therapists can also use wrist immobilization splints as bases for mobilization and static progressive splinting (see Chapter 11). Although some wrist immobilization splints are commercially available, they cannot provide the exact fit of custom-made splints. However, commercially available splints made from soft material may be more comfortable in certain situations, especially in a work or sports setting. Commercially available splints are not as restrictive and allow more functional hand use [Stern et al. 1994]. Some people with rheumatoid arthritis may also prefer the comfort of a soft wrist splint due to its ability to reduce pain and provide stability during functional activities [Nordenskiold 1990, Stern et al. 1997, Biese 2002]. This chapter primarily overviews wrist immobilization splints according to type, features, and diagnoses. The chapter also explores technical tips, trouble shooting, the use of prefabricated splints, the impact on occupations, and the application of a wrist mobilization and serial static approach. In clinical practice the therapist must decide whether to fabricate a volar, dorsal, ulnar, or circumferential wrist immobilization splint. Each has advantages and disadvantages [Colditz 2002]. The volar wrist immobilization splint (Figure 7-1) depends on a dorsal wrist strap to hold the wrist in extension in the splint. An appropriate design furnishes adequate support for the weight of the wrist and hand. In cases in which the weight of the hand (flaccidity) must be held by the splint or in which the person is pulling against it (spasticity), the strap is not adequate to hold the wrist in the splint. However, a well-designed volar wrist splint with a properly placed wide wrist strap will support a flaccid wrist [personal communication, K. Schultz-Johnson, April 6, 2006]. The volar design is best suited for circumstances that require rest or immobilization of the wrist when the person still has muscle control of the wrist [Colditz 2002]. In one study [Stern 1991], the volar wrist splint allowed the hand the best dexterity of custom-made wrist splints. A volar wrist splint’s greatest disadvantage is interference with tactile sensibility on the palmar surface of the hand and the loss of the hand’s ability to conform around objects [personal communication, K. Schultz-Johnson, April 6, 2006]. In the presence of edema, one must use this design carefully because the dorsal strap can impede lymphatic and venous flow [Colditz 2002]. To address the presence of edema, a strap adaptation can be made by fabricating a continuous strap. The therapist applies self-adhesive Velcro hooks along the radial and ulnar borders of the splint, which are attached by a flexible fabric to create a soft dorsal shell. Some therapists fabricate dorsal splints with a large palmar bar that supports the entire hand. This large palmar bar tends to distribute pressure well and is necessary for the comfort and function of the splint. However, a large palmar bar does not free up the palmar surface as much for sensory input as a dorsal splint fabricated with a thinner palmar bar (Figure 7-2). Dorsal wrist splints designed with a standard strap configuration can be better tolerated by persons who have edematous hands because of the pressure distribution. Either the volar or the dorsal design may be used as a base for mobilization (dynamic) splinting. However, these designs can sometimes lead to splint migration and suboptimal splint performance. The ulnar wrist splint is easy to don and doff and can be applied if the person warrants more protection on the ulnar side of the hand, such as with sports injuries (Figure 7-3). This splint design is sometimes used for a person who has carpal tunnel syndrome (CTS) or for ulnar wrist pain [LaStayo 2002]. It can also be used as a base for mobilization splinting. A circumferential splint is helpful in preventing migration, especially when used as a base for mobilization splints. It also provides good forearm support, controls edema, provides good pressure distribution, and avoids edge pressure [personal communication, K. Schultz-Johnson, April 1999]. Some people may feel more confined in a circumferential splint. When fabricating a circumferential splint, the therapist is conscious of a possible pressure area over the distal ulna and checks that the fingers and thumb have full motion [Laseter 2002] (Figure 7-4). One among many circumferential splint options is a “zipper” splint made out of perforated thermoplastic material (Figure 7-5). Understanding the features of a wrist immobilization splint helps therapists splint appropriately. Whether fabricating a volar, dorsal, ulnar, or circumferential wrist splint, the therapist must be aware of certain features of the various components of the wrist immobilization splint—such as a forearm trough, metacarpal bar, and hypothenar bar [Fess et al. 2005] (Figures 7-6 and 7-7). With a volar or dorsal immobilization splint the forearm trough should be two-thirds the length of the forearm and one-half the circumference of the forearm to allow for appropriate pressure distribution. It is sometimes necessary to notch the area near the distal ulna on the forearm trough to avoid a pressure point. The splintmaker should also carefully consider the application of straps to the wrist splint. The therapist applies straps at the level of the MP bar, exactly at the wrist level, and at the proximal end of the splint. The straps attach to the splint with pieces of self-adhesive Velcro hook. The therapist should note that the larger the piece of self-adhesive hook Velcro, the larger the interface between it and the splint thermoplastic material. This larger interface helps ensure that it will remain in place and not peel off. With the identification of the potential for pressure or shear problems, the therapist applies padding to the splint (see Figures 7-1, 7-6, 7-14, 7-15, 7-16). The specific wrist positioning depends on the diagnostic protocol, physician referral, and person’s treatment goals. When the goal is functional hand use during splint wear, the therapist must avoid extreme wrist flexion or extension because either position disrupts the normal functional position of the hand. These positions can contribute to the development of CTS [Gelberman et al. 1981, Fess et al. 2005]. An exception to this rule is when the splint goal is to increase passive range of motion (PROM). In that case, an extreme position may be indicated. However, extreme positions may preclude function. The therapist must judge whether the trade-off is worth the loss of function [personal communication, K. Schultz-Johnson, April 1999]. The therapist performs a thorough hand evaluation before fitting a person with a wrist immobilization splint and provides the person with a wearing schedule, instructions about splint maintenance and precautions, and an exercise program based on particular needs. Physicians and experienced therapists may have detailed guidelines for positioning and wearing schedules. Every hand is slightly different, and thus splint positioning and wearing protocols vary.Table 7-1 lists suggested wearing schedules and positioning protocols of common hand conditions that may require wrist immobilization splints. For CTS, splinting the wrist as close as possible to 0 degrees (neutral) helps avoid added pressure on the median nerve [Gelberman et al. 1981, Weiss et al. 1995, Kulick 1996]. One study using sonography to determine the best wrist position for splinting CTS found that the majority of subjects benefited from a neutral position. However, a few subjects improved from splinting in either a wrist position of 15 degrees extension or 15 degrees flexion [Kuo et al. 2001]. This suggests better front-end diagnostic procedures to determine the most accurate splinting position. One must be careful when applying prefabricated wrist immobilization splints for CTS because some splints place the wrist in a functional position of 20 to 30 degrees of extension [Weiss et al. 1995, Osterman et al. 2002]. Therefore, if it is possible to adjust the wrist angle of the splint it should be modified to a neutral position. Some of the prefabricated splints have a compartment in which a metal or thermoplastic insert is placed, and the insert allows adjustments for wrist position. However, prefabricated splints that have their angles adjusted may become looser, less rigid, and less comfortable than a custom molded splint [Walker et al. 2000]. Generally, custom splints are recommended for CTS because they provide better support, positioning [McClure 2003], and more constant allocation of pressure over the carpal tunnel than prefabricated splints—especially those that are incorrectly fitted [Hayes et al. 2002]. If a person does not tolerate a custom-made splint, the therapist may need to consider providing a prefabricated splint [personal communication, Lynn, 2003]. Another consideration with the wrist immobilization splint provision is the amount of finger flexion allowed. Recent research evidence suggests that finger flexion affects carpal tunnel pressure, especially if fingers fully flex to form a fist [Apfel et al. 2002]. That is because the lumbrical muscles may sometimes enter the carpal tunnel with finger flexion [Cobb et al. 1995, Seigel et al. 1995]. When splints are provided to clients with CTS, they should be instructed to not flex their fingers “beyond 75% of a full fist” [Apfel et al. 2002, p. 333]. Therefore, therapists should check finger position with splint provision. Osterman et al. [2002] advised therapists to fabricate a volar wrist splint with a metacarpal block to decrease finger flexion if CTS symptoms are not improving. When fabricating a splint for a person who has CTS, the therapist considers home and occupational demands carefully, keeping in mind that the wrist contributes to the overall function of the hand [Schultz-Johnson 1996]. If a splint is worn at work, durability of the splint and the ability to wash it may be salient. Some people may benefit from the fabrication of two splints (one for work and one for home), especially if their job demands are in an unclean environment. Many computer operators tolerate a splint that supports the wrist position in the plane of flexion and extension but allows 10 to 20 degrees of radial and ulnar deviation for effective typing. Fabricating a slightly wider metacarpal bar on a custom-made wrist splint allows for a small area of mobility on the radial and ulnar sides of the hand [Sailer 1996]. Finally, the therapist simulates work and home tasks with the wrist immobilization splint on the person to check for functional fit [Sailer 1996]. Therapists also take into account splint-wearing schedules. Options that can be prescribed are nighttime wear only, wear during activities that irritate the condition, a combination of the latter two schedules, or constant wear. In one study, subjects were found to benefit most from full-time wear of the splint, but wearing compliance was an issue [Walker et al. 2000]. This study further validated improvements in clients who wore a neutral position wrist splint for six weeks. Nevertheless, it is important to consider nighttime wear of splints because some people maintain extreme wrist flexion or extension postures during sleep [Sailer 1996]. An exercise program issued with a splint may be an effective conservative treatment [Rozmaryn et al. 1998]. In one study (n =197), a conservative treatment program for CTS that combined nerve and tendon gliding exercises with wrist immobilization splinting was found to be more effective in helping people avoid surgery than splint wear alone. It is hypothesized that these exercises help improve the excursion of the median nerve and flexor tendons because the exercises may contribute to the remodeling of the adhered tenosynovium [Rozmaryn et al. 1998]. Akalin et al. [2002] (n = 28) also studied tendon and nerve gliding exercises with splinting compared to splinting alone. Ninety-three percent of the splinting and exercise group participants reported good to excellent results compared to 72% of the splint-only group participants. However, the researchers did not consider the results statistically significant. Both studies accentuate the value of early conservative intervention. Other effective treatment measures for CTS are the modification of activities (so that the person does not make excessive wrist and forearm motions, especially wrist flexion). It is also important to avoid sustained pinch or grip activities and to use good posture whenever possible with all activities of daily living (ADL). Because CTS is generically a disease of decreased blood supply to the soft tissues. Nerves need blood supply and an environment that is cold will additionally deprive the nerve of blood. Thus, staying warm is an important part of CTS care and splints provide local warmth [personal communication, K. Schultz-Johnson, April 6, 2006]. When conservative measures are ineffective, surgery is an option. The goals of wrist splinting after carpal tunnel release surgery are to minimize pressure on the median nerve, prevent bowstringing of the flexor tendons [Cook et al. 1995], provide support during stressful activities, maintain gains from exercise [Messer and Bankers 1995; personal communication, K. Schultz-Johnson, April 1999], and rest the extremity during the immediate healing phase. Some therapists do not apply a wrist immobilization splint postoperatively because of concerns about the impact of immobilization on joint stiffness and muscle shortening [Hayes et al. 2002]. Findings from one study [Cook et al. 1995] (n=50) suggest that splinting post-surgery resulted in joint stiffness as well as delays with returning to work, recovering grip and pinch strength, and resuming ADL. These researchers concluded that if splinting is used it should be applied for one week only postoperatively to prevent tendon bowstringing and nerve entrapment. Splinting postoperatively is recommended to prevent extreme nighttime wrist postures (flexion and extension) or to manage inflammation [Hayes et al. 2002]. Therapists instruct the person to gradually wean away from the splint (when the splint is no longer meeting the person’s therapeutic goals) in order to prevent stiffness and allow the person to return to work and ADL more quickly. Weaning is often done over the course one week, gradually decreasing the hours of splint wear [personal communication, K. Schultz-Johnson, April 6, 2006]. A series of recent studies were conducted to examine splinting compared to other treatments, such as surgery or steroid injections (seeTable 7-2, which outlines the research evidence). The majority of studies comparing splinting to surgery favored surgery as the most effective treatment for CTS [Gerritsen et. al 2002, Verdugo et al. 2004]. Splinting did show some promising results, but was not as strong in efficacy as surgery. For example, with the Gerrtisen et al. [2002] study (n=178) after 18 months 75% of the subjects improved with splint wear as compared to 90% of the surgery group. The researchers recommended that splinting is beneficial while waiting for surgery, or if a client does not desire surgery. When considering the results of this study, therapists should recognize that 75% improvement with splinting is a high success rate and is less risky than having surgery. Some people do not want therapy, splinting, and activity modification and therefore may best benefit from a surgical approach [personal communication, K. Schultz-Johnson, April 6, 2006]. Therapists need to critically examine such studies for limitations when making an informed decision for clients. McClure [2003], in an article on evidenced-based practice, considered limitations of studies about splinting with CTS. For example, he questioned the results of the Verdugo et al. [2004] study. He queried whether the same results would have occurred with mild CTS symptoms and that the study was done with “only one small randomized trial” [McClure 2003, p. 259]. McClure [2003] also considered the limitations of the Gerritsen et al. [2002] study. He mentioned that information regarding the splint-wearing schedule, other treatments, how clients were classified, and symptom severity were missing from the study [McClure 2003]. Other researchers examined the effect of splinting and nonsteroidal anti-inflammatory drugs (n=33 hands) [Celiker et al. 2002, Graham et al. 2004]. Celiker et al. [2002] (n=99 hands) found that splinting along with steroid injections for clients who had symptoms less than nine months resulted in significant improvement. In another study, steroid injections and wrist splinting for three weeks was found to be effective in clients who had symptoms of less than three months duration and no residual sensory impairments [Graham et al. 2004]. Using only splints for CTS was also studied (n=66 subjects), with significant improvement after four weeks reported [O’Connor et al. 2003]. Gerritsen et al. [2003] (n=89 subjects) reported that the shorter duration of complaints and the severity of nocturnal parasthesias were positively related to splinting success. Therapists and physicians must be aware of current studies because these can influence treatment approaches. Therapists need to critically question how the studies were performed and be aware of limitations. As McClure [2003, p. 261] stated, “these details are important in deciding whether my patient is similar enough to those in the study to use these results with her.” Awareness of current research also points to the fact that many of these studies emphasize the importance of splinting with early intervention because splints are less beneficial with ongoing parasthesia [Burke et al. 2003]. Radial nerve injuries most commonly occur from fractures of the humeral shaft, fractures and dislocation of the elbow, or compressions of nerve [Skirven 1992]. Other reasons for radial nerve injuries include lacerations, gunshot wounds, explosions, and amputations. The classic picture of a radial nerve injury is a wrist drop position whereby the wrist and MCP joints are unable to actively extend. If the wrist is involved, sometimes a physician may order a wrist splint to place the wrist in a more functional position. The exact wrist positioning is highly subjective, and it is up to the therapist and the client to decide on the amount of extension that maximizes function. Commonly, 30 degrees of extension is considered a position of function because it facilitates optimum grip and pinch [Cannon 1985]. Although a wrist splint is one option that can be fabricated for this condition, there are many other options therapists should critically consider. These include the location of splinting (volar versus dorsal), type of splint (e.g., wrist immobilization, tendodesis, or a splint with static elastic tension), and whether to fabricate one or two splints. More details about these other types of splinting options for a radial nerve injury are discussed in Chapter 13. Tendinitis (inflammation of the tendon), tenosynovitis (inflammation of the tendon and its surrounding synovial sheath), and tendinosis (a non-inflammatory tendon condition that involves collagen degeneration and disorganization of blood flow) [Khan et al. 2000] are painful conditions that benefit from conservative management, including wrist splinting. These conditions commonly occur because of cumulative and repetitive motions in work, home, and leisure activities. Tendinosis is more chronic in nature than tendonitis or tenosynovitis and usually impacts the lateral and medial elbow and rotator cuff tendons of the upper extremity [Khan et al. 2000]. Having tendonitis and tenosynovitis can result in an overuse cycle. The overuse cycle begins with friction, microscopic tears, pain, and limitations in motion, followed by resting the involved area, avoidance of use, and development of weakness. When activities resume, the cycle repeats itself [Kasch 2002]. Tendinitis or tenosynovitis can occur in many of the muscles on the volar (flexor muscles) and dorsal (extensor muscles) surfaces of the forearm. These conditions often lead to substitution patterns and muscle imbalance [Kasch 2002]. Resting the hand in a splint helps to take tension off the muscle-tendon unit. Splinting for tendinitis or tenosynovitis minimizes tendon excursion and thus decreases friction at the insertion of the muscles. Splinting can serve as a reminder to decrease engagement in painful activities. It is beneficial to ask clients to pay attention to those activities that are limited by a splint because they are often aggravating factors for tendonitis. Clients should become more cognizant of aggravating activities and modify them so as not to enhance the condition [personal communication, K. Schultz-Johnson, April 6, 2006]. Clients should also be cautioned not to tense their muscles and thus fight against the splint when wearing it or it may aggravate the tendonitis. Rather, the muscles should be relaxed. Splints provided for tendonitis or tenosynovitis during acute flare-ups are worn continuously, with removal for hygiene and range-of-motion (ROM) exercises followed by gradual weaning. Generally, when splinting for flexor carpi radialis (FCR) tenosynovitis it is recommended that the person’s wrist be splinted at neutral to rest the tendons [Idler 1997]. Wrist extensor tendinitis can be splinted in 20 to 30 degrees of wrist extension, as this normal resting position provides a balance between the flexors and extensors.
Splints Acting on the Wrist
Volar, Dorsal, Ulnar, and Circumferential Wrist Immobilization Splints
Volar
Dorsal
Ulnar
Circumferential
Features of the Wrist Immobilization Splint
Diagnostic Indications
Wrist Splinting for Carpal Tunnel Syndrome
Wrist Splinting for Radial Nerve Injuries
Wrist Splinting for Tendinitis and Tenosynovitis
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine