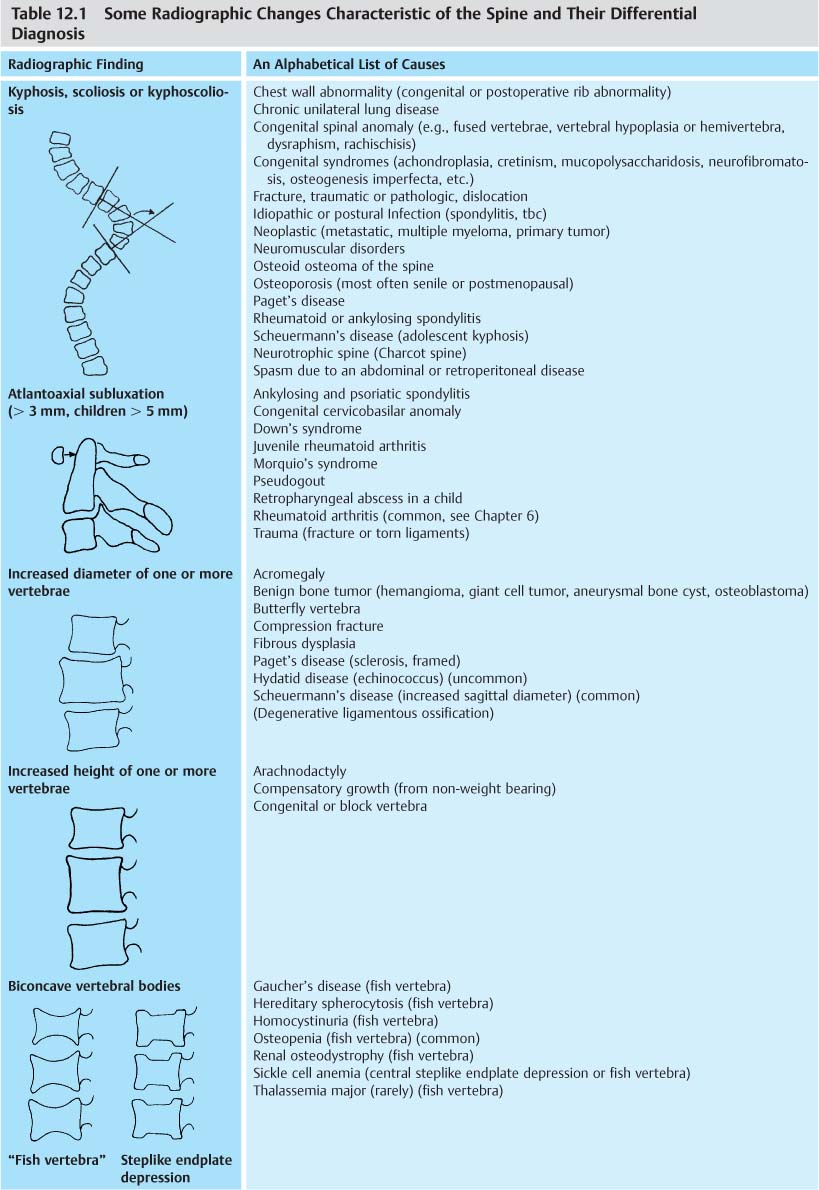
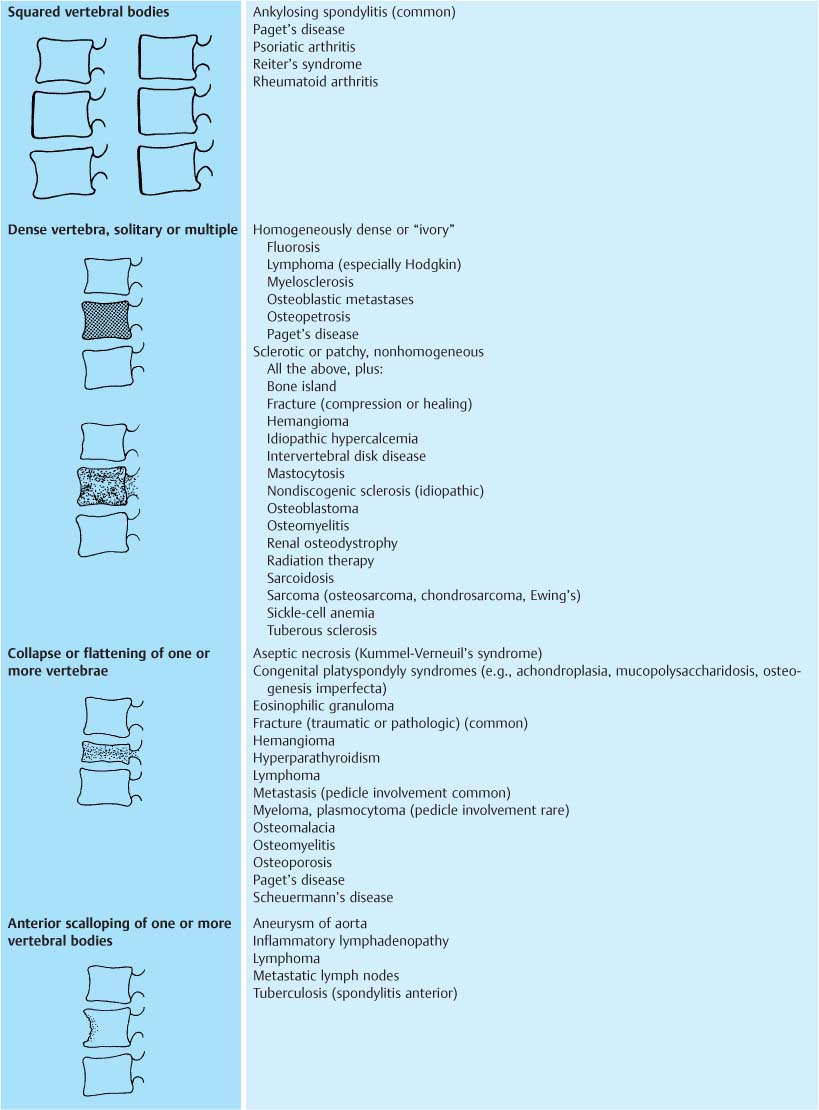
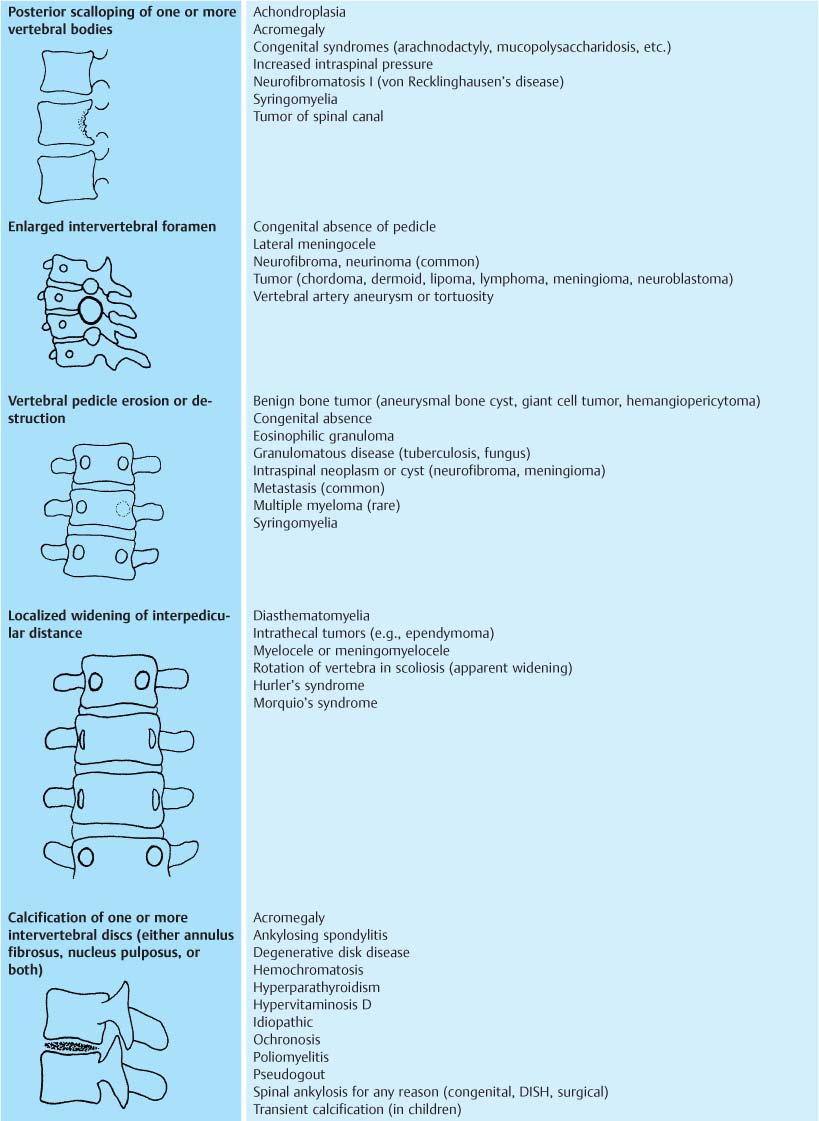
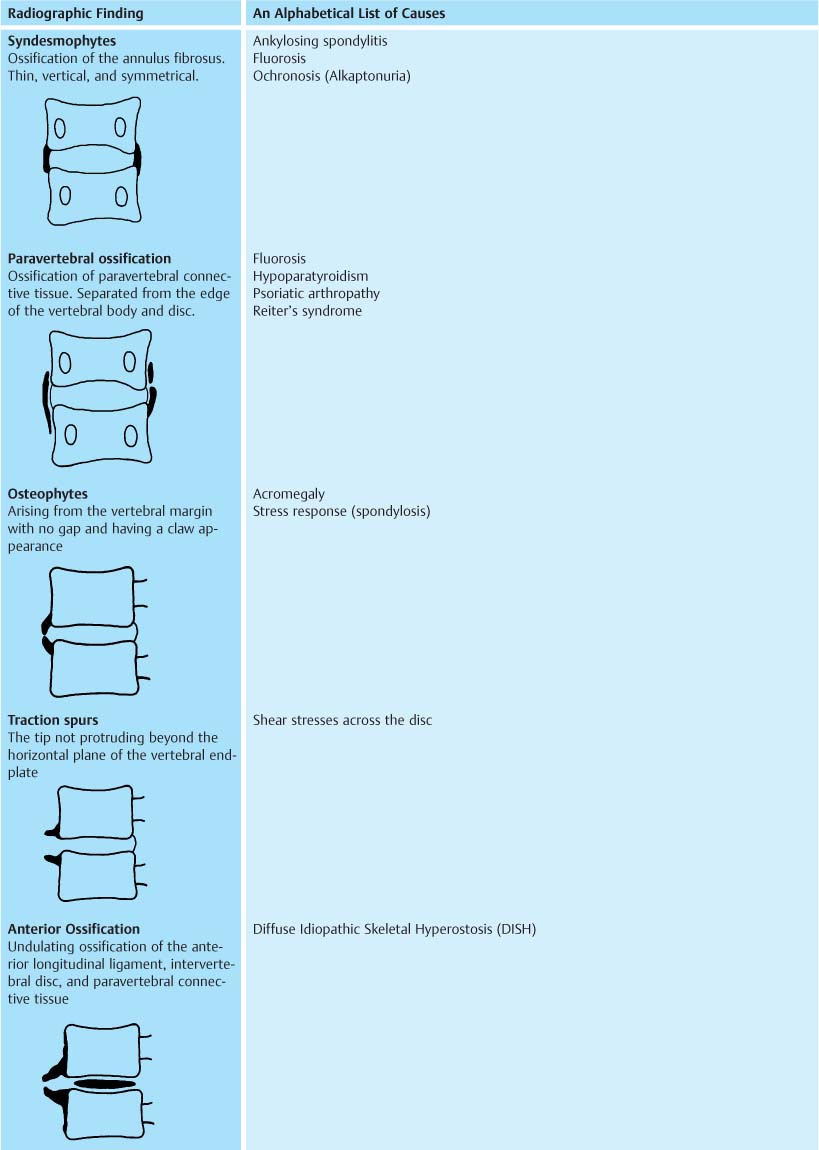
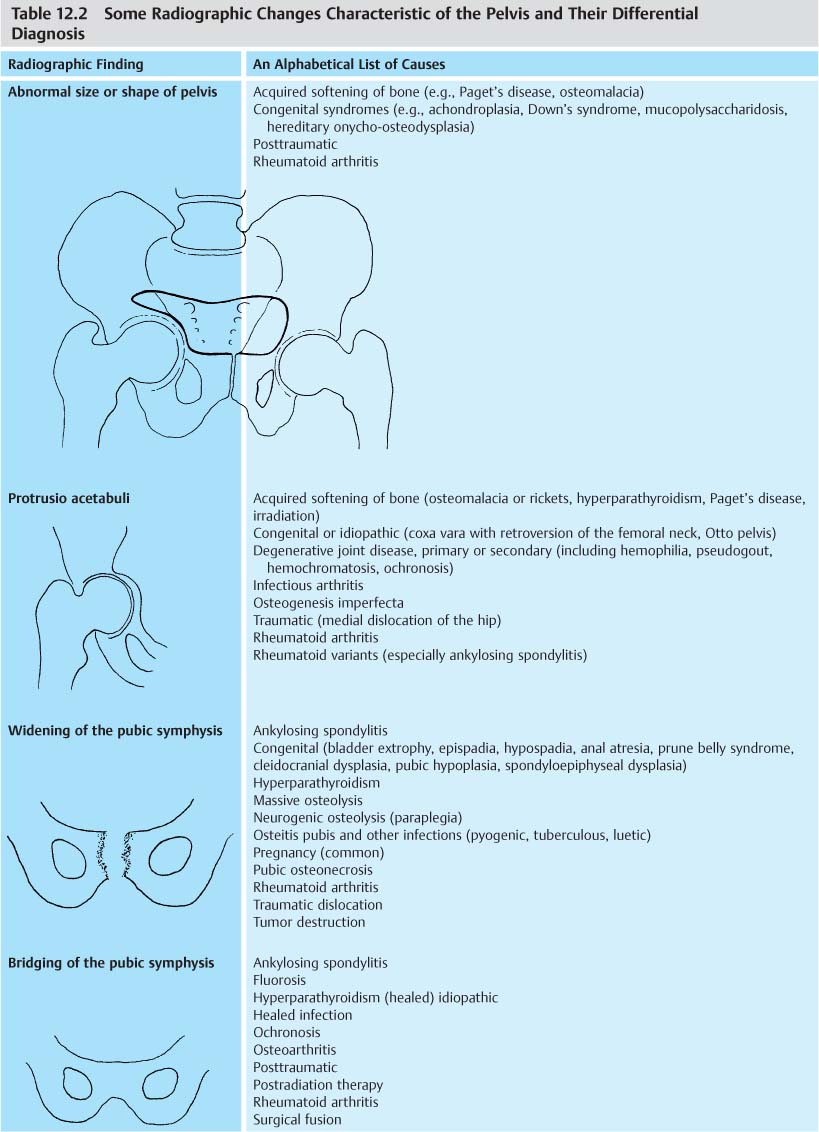
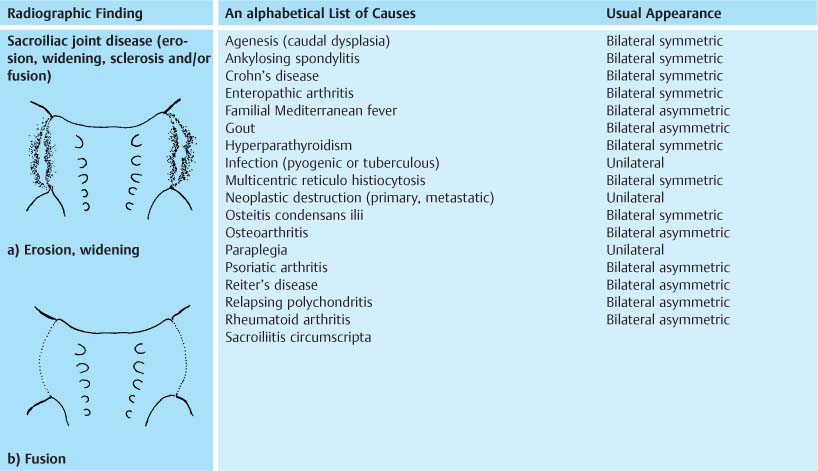
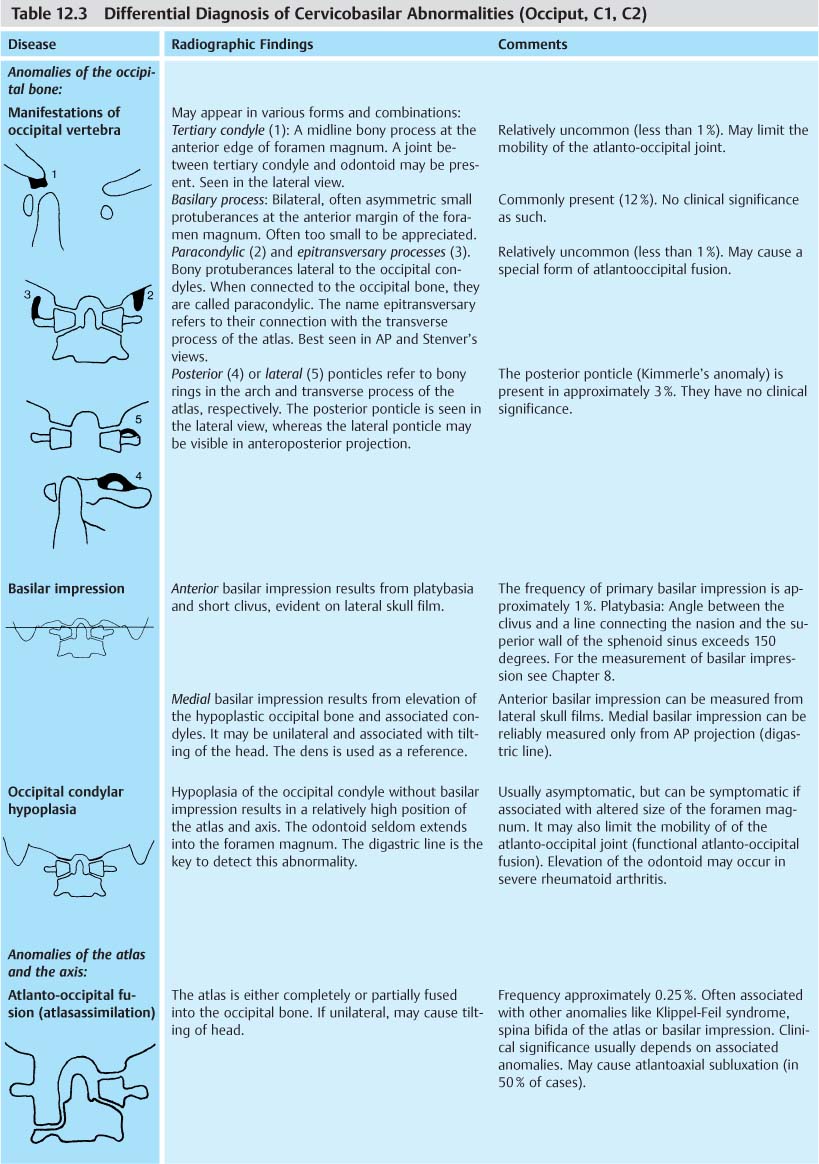
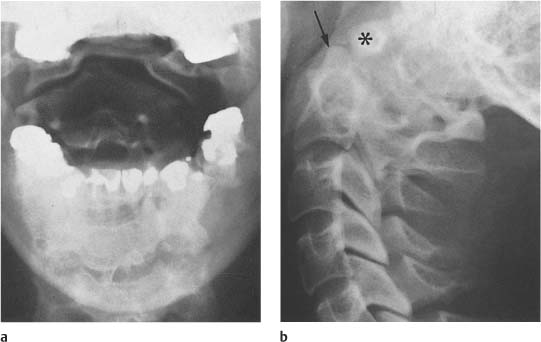
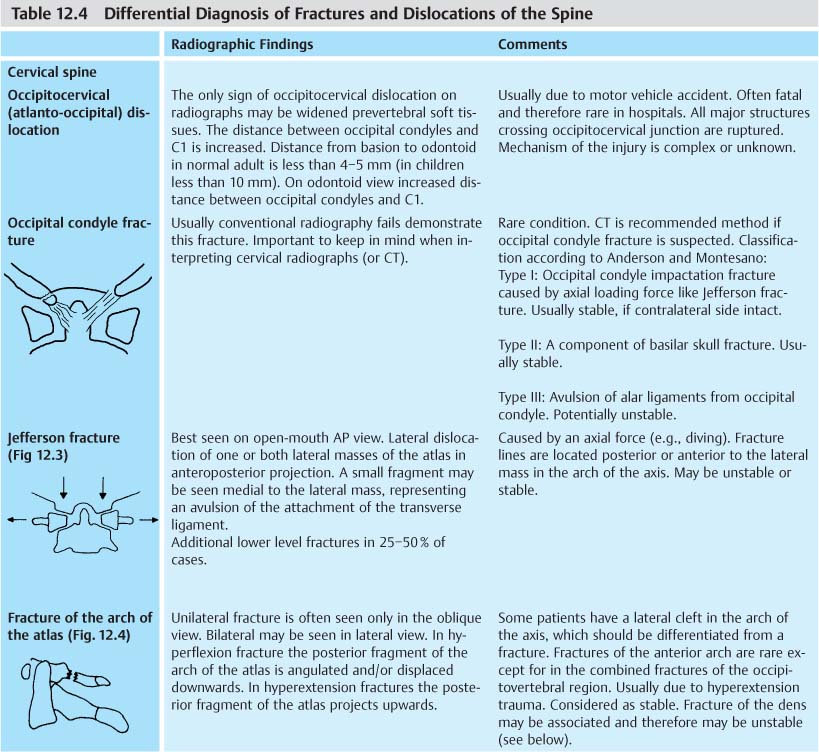
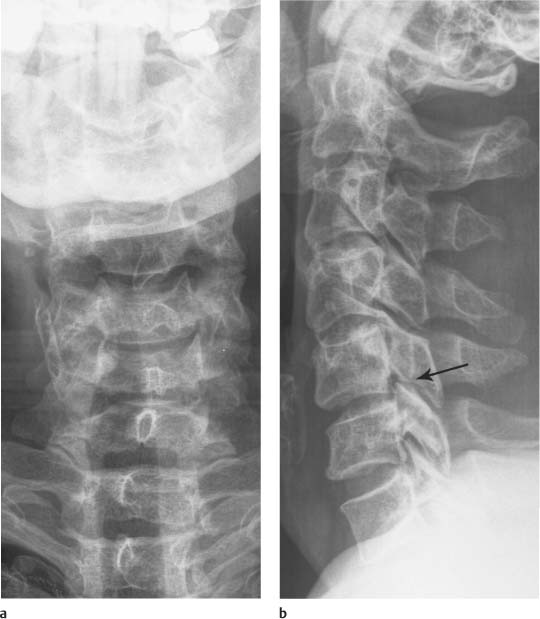
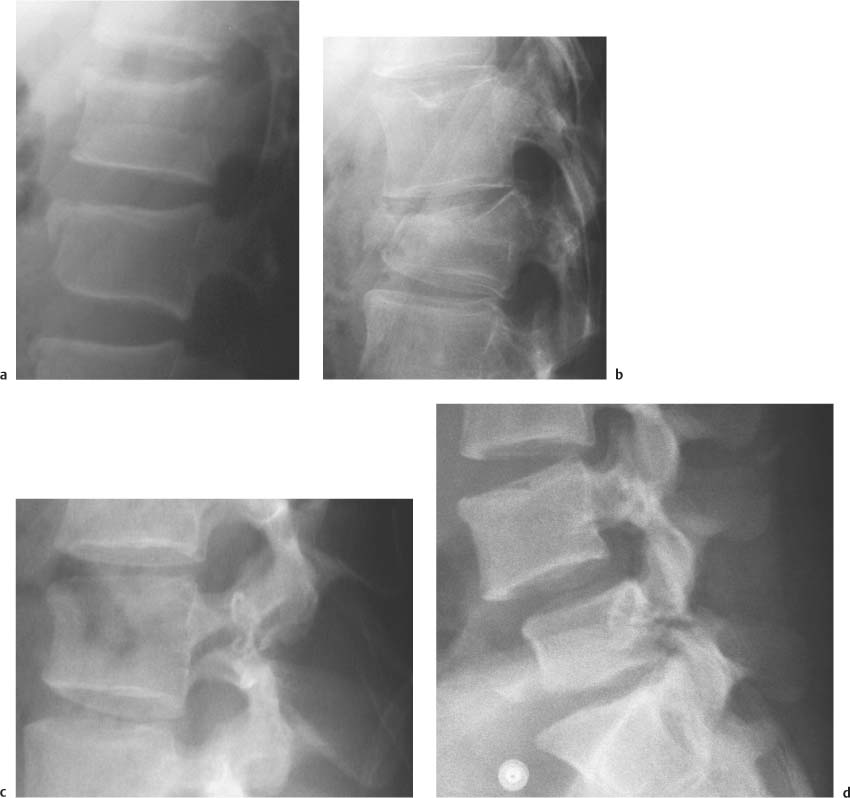
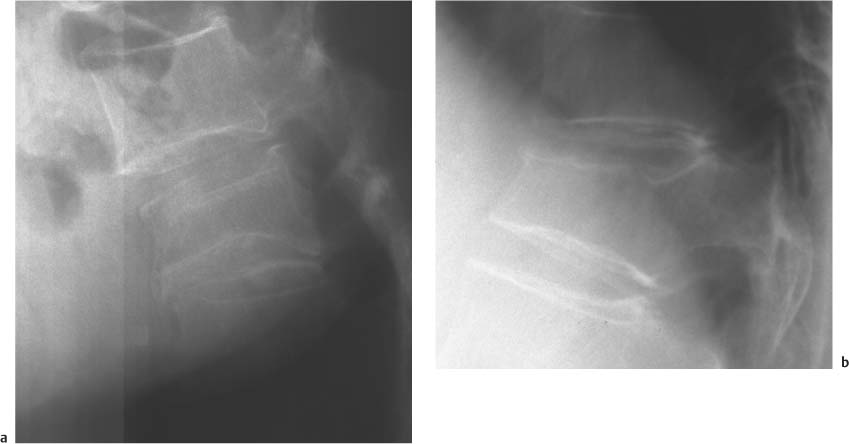
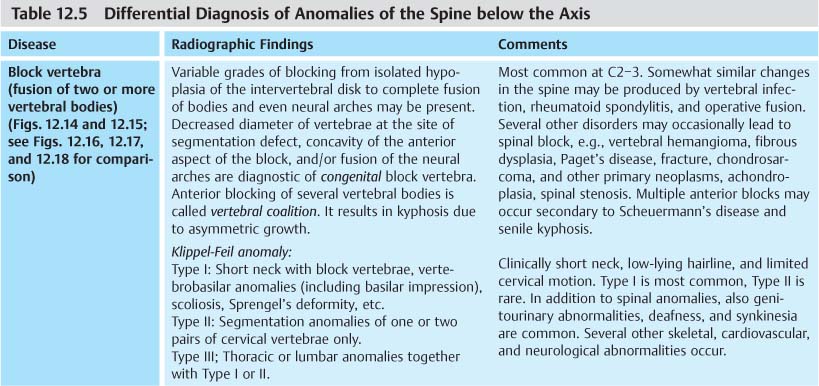
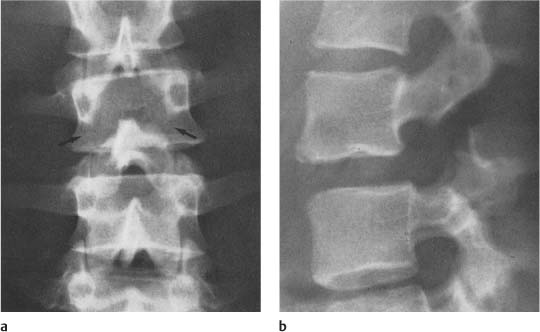
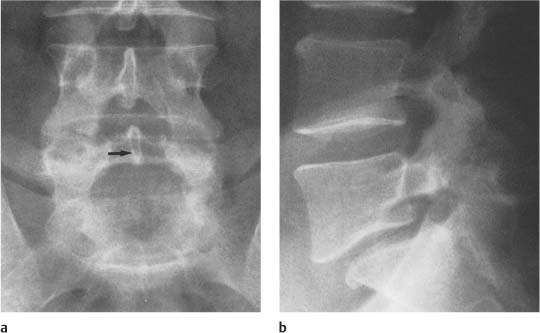
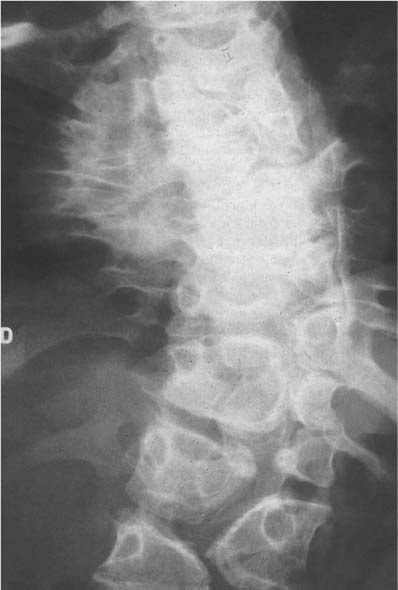
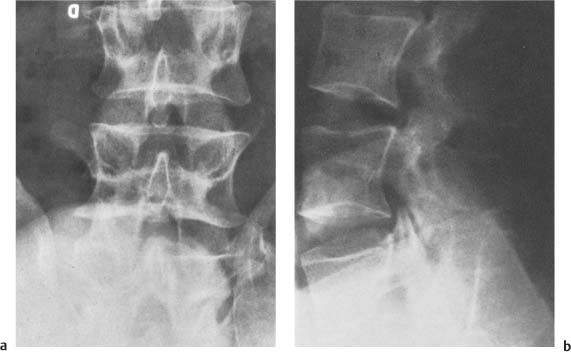
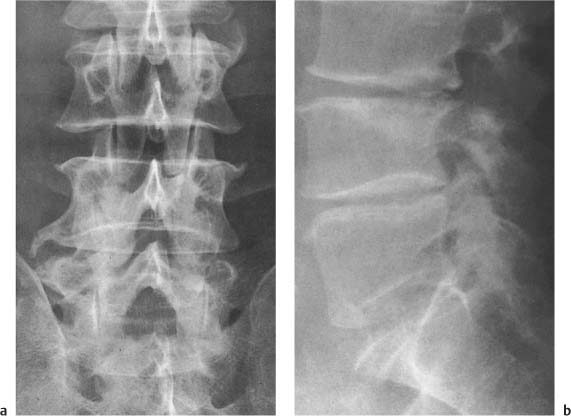
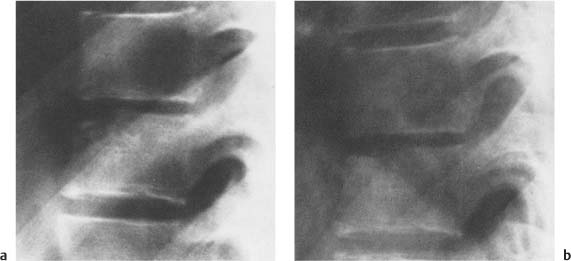
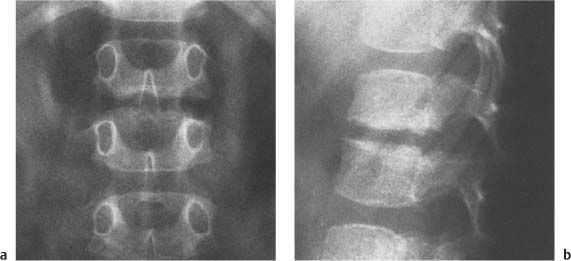
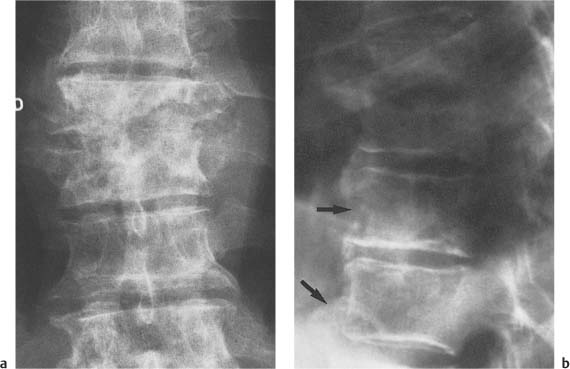
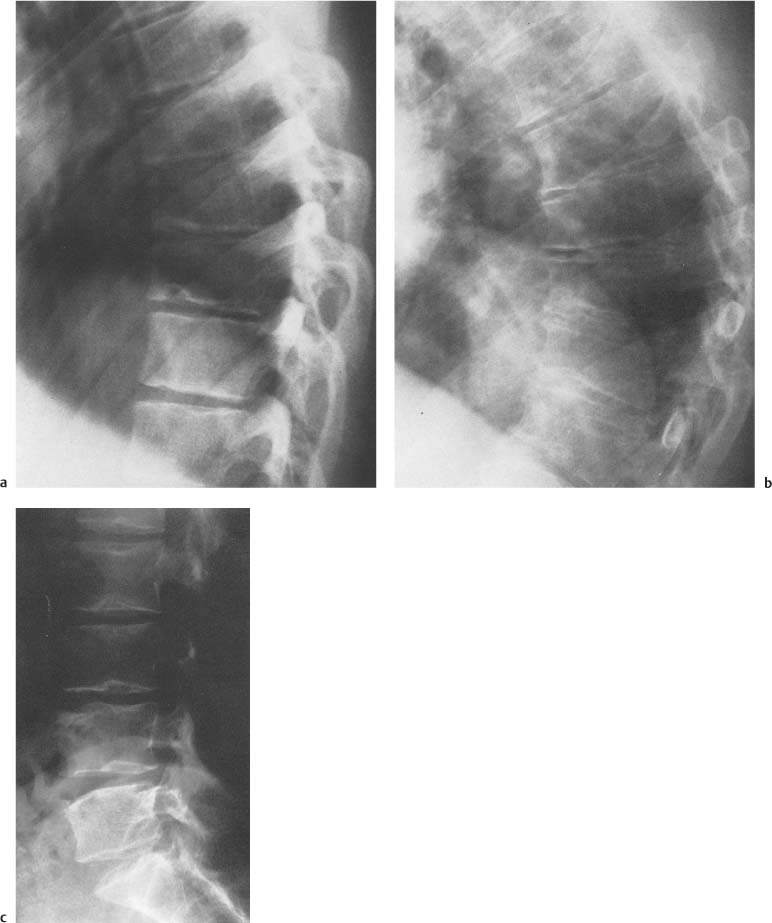
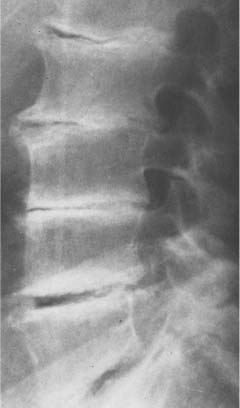
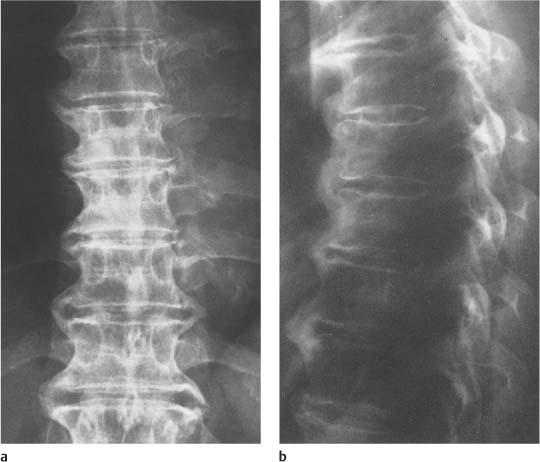
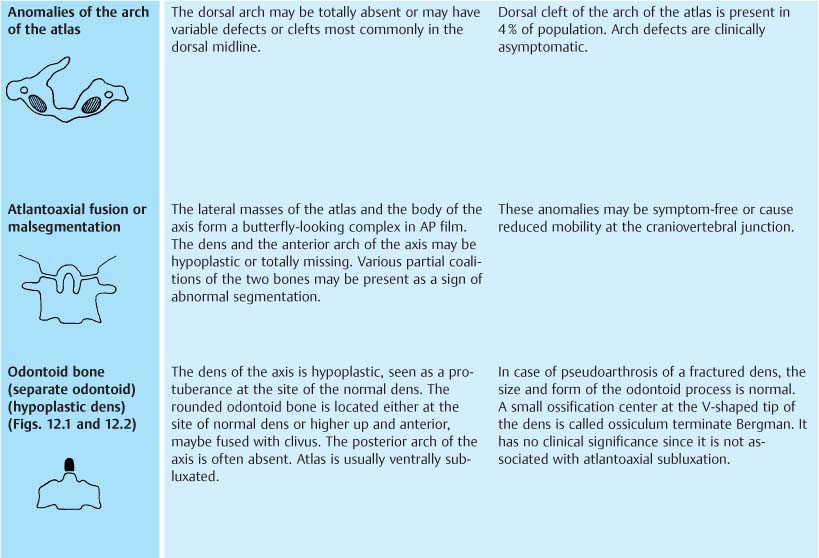
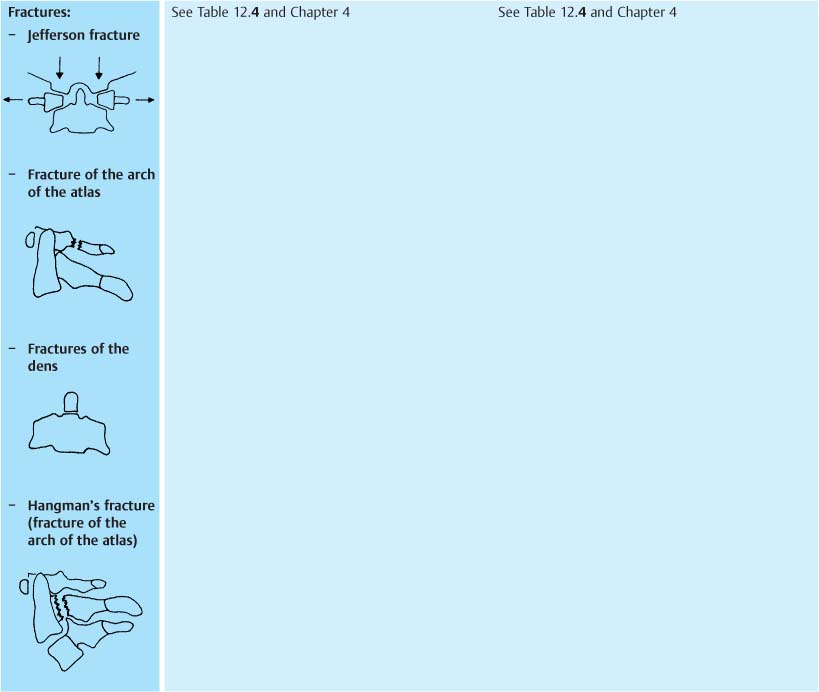
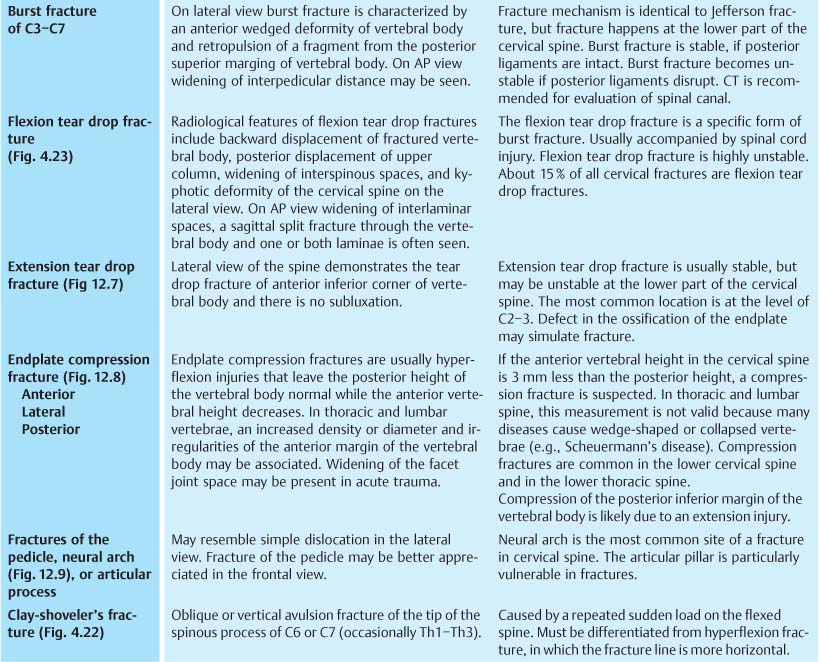
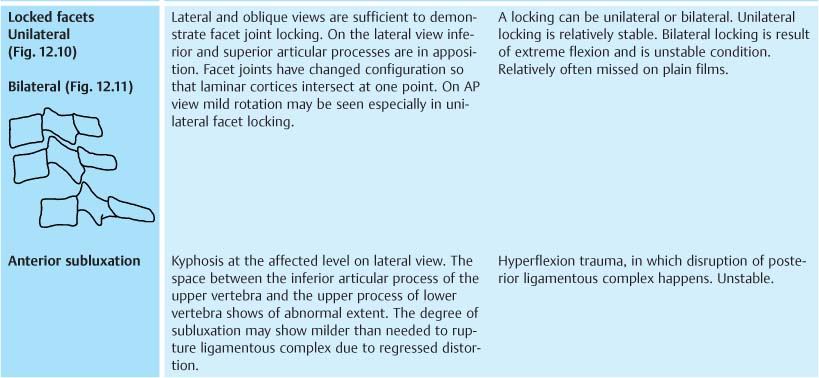
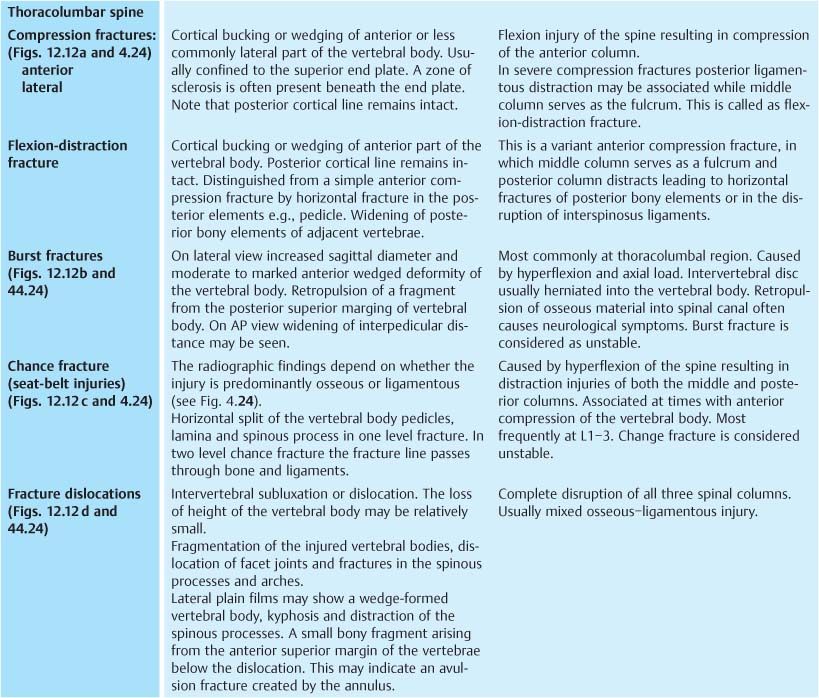
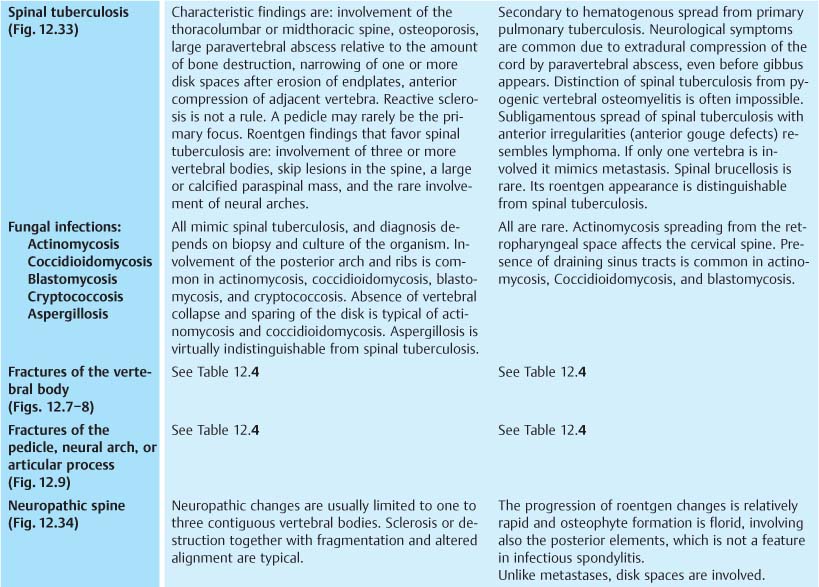
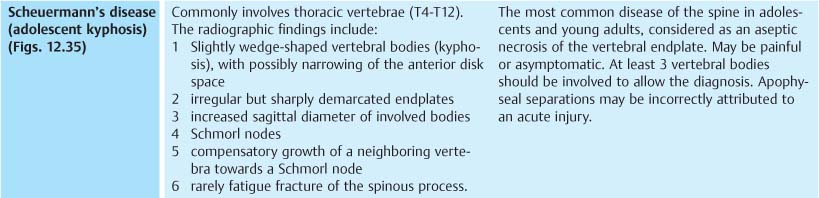
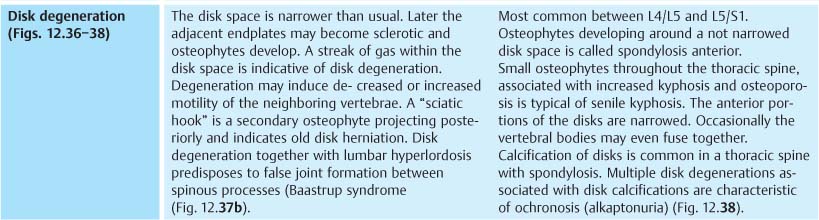
12 Spine and Pelvis The development, structure, and function of the spine is complex. Consequently a great number of either primary or secondary abnormalities are encountered in various portions of the spinal column. Intraspinal lesions may not cause an abnormality on plain films despite serious clinical symptoms. In such cases MRI is advisable. In order to detect all available information from plain films, one should inspect them in a systematic fashion, paying attention to a number of different features. The alignment of vertebrae in the normal spine includes a forward curvature (kyphosis) in the thoracic portion and a backward curvature (lordosis) in the cervical and lumbar portions. Loss of normal curve or straightening of the spine, often secondary to muscular spasm of variable etiology, may be difficult to evaluate in films taken on a Bucky table. The true extent of anteroposterior curves, as well as eventual lateral curvatures (scoliosis), is better evaluated in a weight-bearing (standing) position, if such positioning is not contraindicated by acute spinal trauma. Likewise, slippage of one vertebral body on the next either forward (spondylolisthesis) or backward may be better appreciated by taking flexion and extension views in a weight-bearing position. A number of congenital or acquired diseases cause either general or local changes in the size, shape, structure, and/or density of the vertebral bodies and neighboring disk spaces. Such changes may or may not involve the neural arch. Plain films do not show intervertebral disks. For the evaluation of disk degeneration, protrusion or prolapse, MRI should be used. Facet joints are seen in plain films but for accurate evaluation of facet joint abnormalities and associated effects on root channels or spinal canal, a multislice CT examination or MRI is required. Tables 12.1 and 12.2 are lists of some cardinal roentgen features of the spine and pelvis, respectively. They may serve as a reference point for differential diagnosis. The occipitovertebral junction is developmentally a specialized area presenting a number of congenital anomalies. The latter as well as some acquired abnormalities of the upper cervical spine have radiographic features not seen elsewhere in the spinal column, and are presented in Table 12.3. Table 12.5 presents a list of localized abnormalities involving the spine and their radiographic characteristics. Tumors involving the pelvis are presented together with tumors of the spine in Table 12.6. A more detailed discussion of bone tumors, including spine and pelvic bones, is found in Chapter 5. Cervical spine fractures are caused by hyperflexion, hyperextension, hyperrotation, hyperflexion and rotation, lateral hyperflexion, and vertical compression. Fractures of spinal column are summarized in Table 12.4. Sacrum and coccyx are an integral part of the pelvis, although they essentially belong to the spine. Localized abnormalities of the sacrum, coccyx, and the rest of the pelvic girdle are therefore presented here together. Localized processes in the pelvic bones are not different radiographically from similar lesions in any flat bone. Abnormal size and shape of the pelvis may be typical of some congenital syndromes. Involvement of sacroiliac joints may have great differential diagnostic significance. Early changes in the sacroiliac joints may be difficult to recognize, especially in young patients, whose sacroiliac joints are not completely ossified. CT and MRI cross-sectional images are helpful in demonstrating subtle changes. The involvement of sacroiliac joints in arthritides has been discussed already in Chapter 6, and is only briefly summarized in Table 12.2. Table 12.7 presents localized lesions usually involving the pelvis only. Abnormal size and shape of the pelvis may be typical of some congenital syndromes. Often they also present with spinal abnormalities. Many of the rare congenital syndromes are not included. The reader should consult texts of pediatric bone radiology in cases of rare congenital osteochondrodysplasias. Table 12.8 presents some congenital and acquired conditions with both pelvic and spinal radiographic findings. Fractures of the spine are summarized in Table 12.4. All seven cervical vertebral bodies must be visible on radiographs. In a case when good quality radiographs can not be obtained one has to consider CT imaging. Multiple fractures occur frequently. Multislice CT with reformats is nowadays highly recommended when serious spinal fracture is suspected. Multislice CT often reveals fractures not seen on radiographs. Fig. 12.1 a, b Hypoplastic dens (arrow) as seen a in AP and b lateral in projection. The atlas (asterisk) is posteriorly displaced. Fig. 12.2 Hypoplastic dens, fusion of C2 and C3 and anterior displacement of the atlas. The posterior arch of the atlas is lacking (Klippel-Feil anomaly, Type I). Fig. 12.3 Jefferson fracture. The space between left atlantoaxial facets has increased on AP view. Fig. 12.4 Hyperextension fracture of the arch of the atlas (arrows). The posterior fragment of the atlas projects characteristically upwards. Fig. 12.5 Fracture of the dens with anterior subluxation of the atlas and the dens. Fig. 12.6 Hangman’s fracture of the arch of the axis with anterior subluxation of the body of the axis. Fig. 12.7 Tear drop fracture of the anterior inferior margin of C4 resulting from extension injury. There is slight posterior dislocation of C4. Prevertebral soft tissue is thickened. Fig. 12.8 Compression fractures of the anterior superior margins of C6 and C7. The height of the anterior C6 body is decreased, whereas C7 has a chip fracture. Prevertebral soft-tissue thickening is also observed. Fig. 12.9 Fracture through the neural arch of C3 anterior dislocation of the body of C3. Fig. 12.10 Unilateral locking of facet. On AP view the spinous processes of lower cervical spine curve to the left. On lateral view unilateral locking of the facets between C5 and C6 can be seen (arrow). Fig. 12.11 Bilateral facet luxation. Fig. 12.12 a) Anterior compression fracture of upper end plate. The fracture does not extent to posterior margin of the body. b) Burst fracture of L1. A bony fragment is seen protruding into the spinal canal from superior posterior aspect of the body. c) Chance fracture. Mild wedging of the body of L3. Fracture extends through pedicles and transverse processes. d) Fracture dislocation between L4 and L5. The space between processus spinosus of L4 and L5 has increased and processus interarticularis fracture of L5 is visible. L5 body is in mild retroposition. Anterior compression fracture on upper end plate of L4. Fig. 12.13 a Biconcave (Cod fish) osteoporotic fracture. b An old wedge-shaped osteoporotic fracture of T12. Fig. 12.14 Congenital block vertebrae C4–5, C6–7, T1–2 (not shown), associated with posterior ponticle (foramen arcuale) (*) and a defect in the posterior arch of the atlas (arrow) (Klippel-Feil type III). Fig. 12.15 Severe segmentation anomalies of the vertebrobasilar junction and blocking of the cervical spine (KlippelFeil type I). Fig. 12.16 Tuberculous spondylitis of the cervical spine resulted in multiple block vertebrae, which resemble KlippelFeil anomaly. Fig. 12.17 Tuberculous block vertebra (T10 and T11) associated with a gibbus. Fig. 12.18 Posttraumatic block T11, T12, and partially L1. Fig. 12.19 a, b Spondylolysis with minimal Spondylolisthesis of L3. Bilateral defect in the pars interarticularis is well seen in both AP (a) and lateral (b) views. Fig. 12.20 a, b Spondylolisthesis. a The spinous process deviates slightly to the left (arrow) indicating shorter left pars interarticularis. b Anterior displacement of the characteristically wedge-shaped L5 on the lateral film. Fig. 12.21 a, b Spondylolisthesis. a Anterior slipping of L4 with disk degeneration and osteophytes both in spaces L4–L5 and L5–S1. b Spondylolisthesis of L5 in a patient with multiple calcified disk degenerations due to ochronosis. Fig. 12.22 Multiple clefts in the posterior neural arches (arrows) and widening of the spinal canal due to meningocele. Fig. 12.23 Meningocele. Defects in the neural arches are wide and involve three lumbar and all sacral segments. Fig. 12.24 Spina bifida occulta of L5. Fig. 12.25 Multiple segmentation anomalies throughout the spinal column. Not a single normal vertebral body is present. Rib fusions are an associated finding. Fig. 12.26 Lateral hemivertebra with scoliosis (arrow). Fig. 12.27 Narrowing and erosion of the arch of the axis and atlas due to neurinoma (arrows). Fig. 12.28 Neurofibroma. The neural foramen C6–C7 is enlarged (arrow). A dorsal cleft in the arch of the atlas is seen as an incidental finding. Fig. 12.29 a, b Spinal stenosis in achondroplasia. a Anteroposterior film demonstrates lateral narrowing of the spinal canal in L4 and 5. Hypoplastic sacrum is also obvious. b Lateral film of another patient demonstrates narrow sagittal diameter of the spinal canal and posterior scalloping of the vertebral bodies. Fig. 12.30 a, b Acquired spinal stenosis. a The lamina are convergent and the articular processes hypertrophic with superimposed spondylarthritis. b Short pedicles and decreased sagittal diameter of the spinal canal associated with narrowed disk spaces L3–L4 and L4–L5. Fig. 12.31 a, b Pyogenic spondylitis. a There is disk space narrowing, destruction of the anterior portion of two adjacent vertebral bodies, more so in the inferior. b Three months later, sclerotic new bone formation is seen as a sign of healing. Fig. 12.32 a, b Infectious diskitis in a child. Narrowing of the disk space with erosion and sclerosis of the adjacent end plates. Fig. 12.33 a, b Tuberculous spondylitis. Paravertebral abscess is demonstrated in the AP view. Extensive destruction of two adjacent vertebral bodies with surrounding sclerosis. Anterior defects are seen in two lower vertebral bodies (arrows). Fig. 12.34 Neuropathic spine. There is sclerosis, destruction, fragmentation and altered alignment, as well as spondylosis. Fig. 12.35 a–c Scheuermann’s disease. Irregular endplates, increased sagittal diameter of the vertebral bodies, and Schmorl nodes are observed, a Age 18, b age 41. Increased kyphosis due to wedge-shaped thoracic vertebral bodies, c Changes in the lumbar spine. Several endplates contain Schmorl nodes. Apophyseal separations in the upper anterior corners of L4 and L5 simulate fractures. Fig. 12.36 Disk degeneration between L4/L5. The disk space is narrow and contains gas. Fig. 12.37 a, b Multiple disk degenerations with scoliosis and extensive osteophytes. In the lateral view the osteophytes appear as sclerotic lines overlaying the vertebral bodies. Sclerosis in the adjacent spinous processes (arrow) indicates early Baastrup syndrome. Fig. 12.38 Multiple disk degenerations and calcification of disk spaces secondary to ochronosis. There is anteposition of L5 relative to S1 (pseudolisthesis) Fig. 12.39 a, b DISH. Extensive ankylosing osteophytes and calcification of disks, but the disk spaces are not narrowed. Fig. 12.40 Paget’s disease. Squared vertebral bodies have a framed appearance and coarse trabeculae. The process also involves the neural arches. Fig. 12.41 Paget’s disease.
Spine
Pelvis
Conditions Involving Both Spine and Pelvis
Fractures of Spine
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree